Periprosthetic distal femur fracture is an rare entity.It is very difficult to manage. Open reduction and internal fixation with locking plate provides anatomical reduction of the fracture side and we can assess the position of the implant in the same incision.It provides excellent clinical and radiological outcome.
Dr. Amey Sadar,
Resident doctor, Department of Orthopaedics, Grant Government Medical College and J.J. Group of Hospitals, Room Number 727, 300 Resident Hostel, Hospital, Mumbai – 400 008,
Maharashtra, India.
E-mail: ameyyysadarrrr@gmail.com
Introduction: Distal femur periprosthetic fractures are rare entityies and difficult to manage. Supracondylar femur fractures are most common amongst periprosthetic fractures. They can be managed by various modalities. These fractures are often difficult to treat because of various factors likesuch as osteoporosis, communication, female gender, and poor bone stock. Fixation of supracondylar femur fracture by locking plate provides excellent results in terms of radiological and clinical outcomes.
Case Report: We report a case of a 70 year -year-old female with pain and swelling in the right knee since for 1 day. She had a history of fall in bathroom 1 day back. The patient was operated with total knee replacement 6 years back for grade Grade 3 osteoarthritis of the knee. The patient was known case of hypertension and was on medication for the same. We operated the patient by open reduction and internal fixation with distal femur locking plate and it provided excellent clinical outcome.
Conclusion: Periprosthetic supracondylar femur fractures are rare entity entities and generally difficult to manage, especially in elderly patient, due to poor bone quality. The choice of implant used to treat such fractures depends on the surgeon’s choice and patient’s compliance. Open reduction and internal fixation with a locking plate is a good entity as it provides excellent clinical and radiological outcome.
Keywords: Distal femur, supracondylar, periprosthetic fracture, total knee replacement, open reduction and internal fixation.
Periprosthetic fractures are rare entities [1,2] most common type of periprosthetic fracture in the distal femur are supracondylar femur fractures [1,2,3]. Factors responsible for the development of these fractures are many [3,4,5,6]. These include osteoporosis, female gender, poor patient compliance, inflammatory conditions such as rheumatoid arthritis (RA), intraoperative cortical perforation, preoperative femoral deformities, altered biomechanics of the limb after joint arthroplasty, especially after revision surgery [3,4,5,6]. This fractures provides many challenges due to its anatomical location and limited bone stock available for implant fixation. Various modalities are available for fixation. They can be divided into conservative and operative modality. Conservative modalities are obsolute [7,8,9] these days because of longer duration of immobilization, failure of union of fracture, and poor patient compliance. Operative management provides early range of motion, lesser duration of immobilization, and early weight-bearing. Various methods are employed for fixation. Distal femur nail, anatomical locking plate, liss (less invasive stabilization system) are generally used. Distal femur nail provides good stability with minimal damage to soft tissue but all total knee replacement prosthesis are not compatible with distal femur nail design. In such cases, fixation of the fracture with locking plate is preferred. Open reduction and internal fixation (ORIF) with locking plate provide anatomical reduction under vision and early mobilization of the patient . Although it is not devoid of complications as it usually involves soft tissue stripping near the prosthesis, causing devascularization of the already weakened supracondylar femoral region [3,6]. Extensive stripping sometimes is needed to attain good anatomic reduction and due to the associated severe comminution, there is a high risk of delayed union and nonunion [8,10,11].
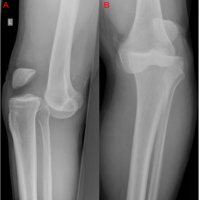
A 60-year-old female presented with complaints of pain and swelling in the right knee for 1 day. The patient was operated with total knee replacement 6 years back for Grade 3 osteoarthritis of the knee. The patient was known case of hypertension and was on medication for the same. On clinical examination, the patient presented withlocalized tenderness and painful restriction of movement around the knee joint. An old scar mark of total knee replacement was present. The scar mark was clean and healthy. Plain radiographs of the right knee with a total length of the femur was taken in ap and lateral view. The radiographs showed extraarticular long oblique distal femur fracture with the prosthesis in situ. On radiographs, Tkr implant was stable and no loosening was observed. CT scan was done to know the extent of the fracture and congruity of the condyles. Blood investigations were done to rule out the infections and they were observed normal. Hypertension was controlled before the planned surgery. Swabs were sent from the axilla, groin, nasal cavity, and ear to rule out any superficial skin infection with due consent. Patient was planned for open reduction and internal fixation with a locking plate. Under all aseptic precautions, the patient was kept in the supine position. The knee was placed in 30 degree flexion. Incision was taken on the lateral aspect of the thigh with schwas-buckler approach.
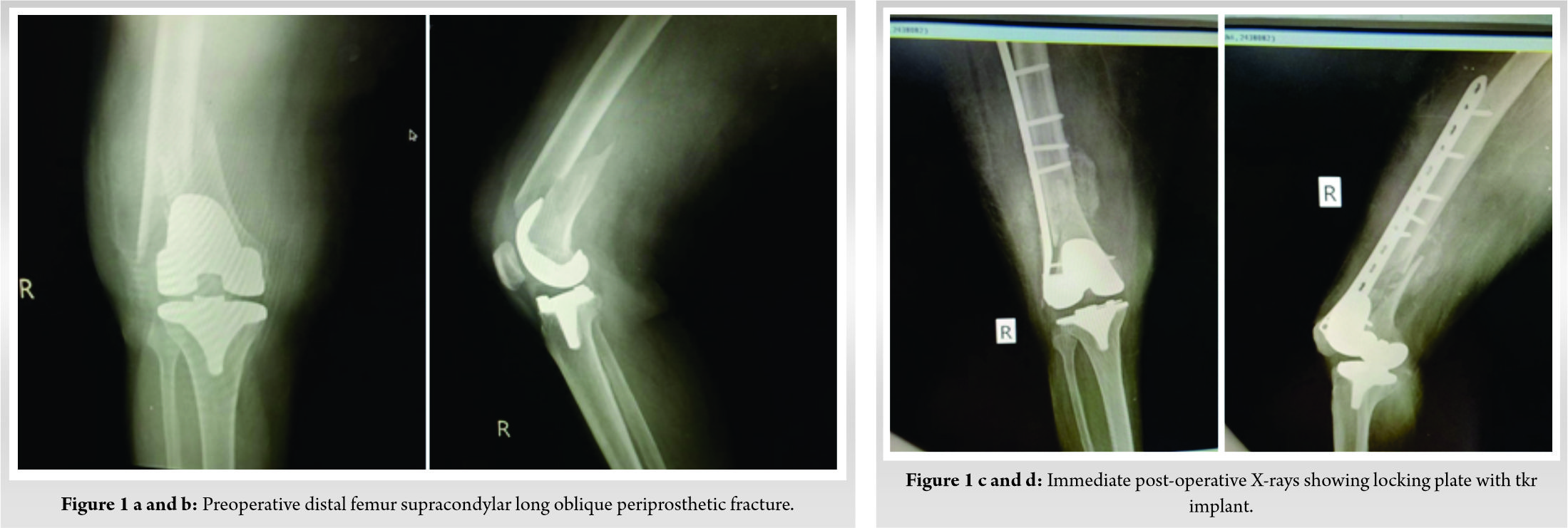
Soft tissue was dissected in layers and fracture site was identified. Hematoma was removed and edges were freshened. The reduction was obtained with bone holding clamps, confirmed under c arm guidance. Temporary thick K wires were placed for holding the reduction. Distal femur locking plate of 11 holes with locking screw was used for fixation. Formal inspection of the tkr implant was done to know the position and any signs of loosening. Procedure was uneventful and wound was closed in layers. The limb was protected with a rigid long knee brace. Check dress was done on day 5 and it was healthy. Patient was discharged on day 12 with all sutures removed. Patient was kept on nil weight bearing on the affected limb with the help of walker for 1 month . Physiotherapy for operated limbs was advised. Follow-up was taken on day 21, 1 month, and 3 months, respectively. Follow-up X-rays were taken with respective visits. Patient being housewife by profession went back to her routine life.
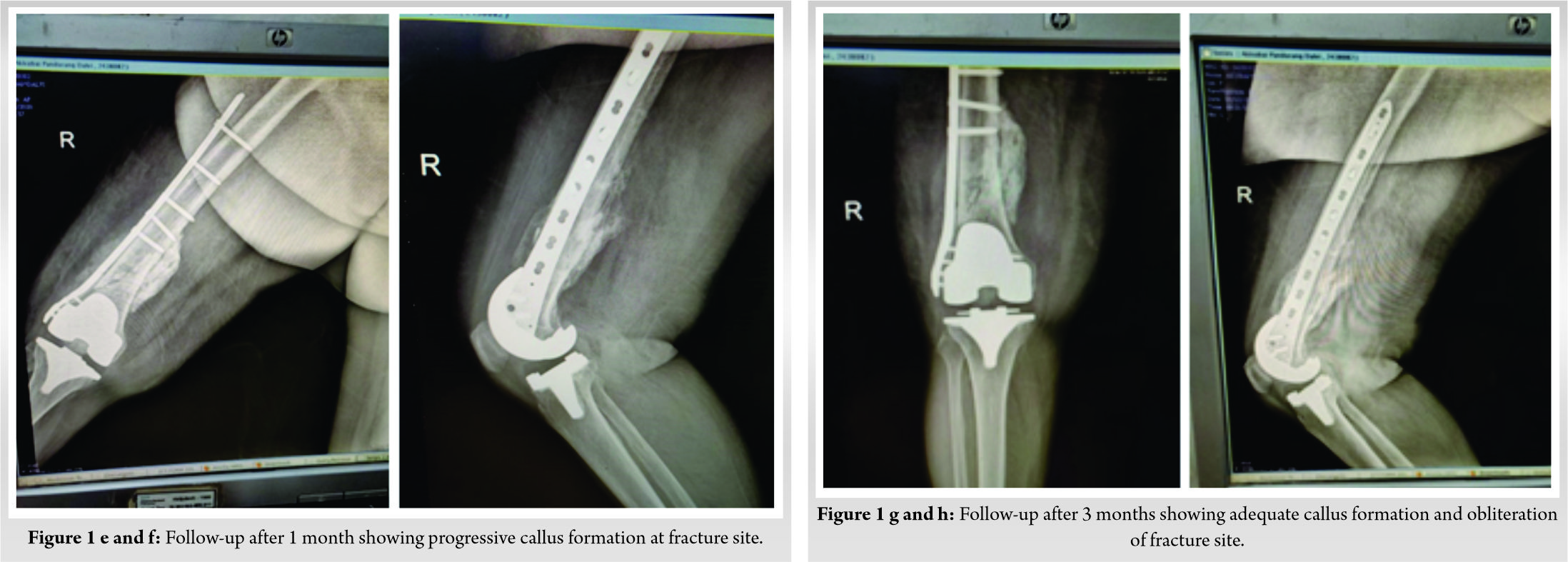
Periprosthetic fractures are rare entities in total knee replacement. The incidence of periprosthetic fractures in TKA is increasing. These fractures are classified according to their location and prosthesis integrity. In the setting of a supracondylar fracture about a well-fixed prosthesis, plate and nail fixation of the fracture present themselves as good options, each having its own unique benefits and pitfalls. Various factors are responsible for causing periprosthetic fracture such as female gender, osteoporosis, limited bone stock, and recent corticosteroid treatment [1,12]. Advanced age is a major risk factor regarded as an individual risk factor itself, as well as a risk factor for osteoporosis and recurrent falls, each of which on their own are qualified as risk factors for periprosthetic fractures. Challenges in the surgical management of fractures by ORIF are associated comminution at the fracture with bone impaction and bone loss, at times [5]. Consequently, this fixation may need to be protected in a brace till radiological evidence of bone healing. Plate fixation is regarded as an acceptable operative procedure in an elderly patient with periprosthetic femoral fractures, even with slightly loosened prostheses [13,14,15]. The aim of treatment in fractures of the distal femur proximal to the TKA prosthesis is to achieve a painless stable knee without any residual malalignment and malfunction [3,8,12]. Early mobilization is essential in obtaining a good result.
Distal femur periprosthetic fractures are rare. In an elderly patient with TKR prosthesis, it is difficult to manage. The choice of implant used for managing such fractures depends on the surgeon’ choice and patient’s compliance. Locking plate osteosynthesis in periprosthetic fracture provides excellent anatomical reduction with good clinical and radiological outcome, especially in osteoporotic bone. Other operative methods can be employed according to the requirement of the patient each having its own advantages and pitfalls.
Periprosthetic fracture is a difficult entity to manage. Careful preoperative evaluation and planning are essential to get the best outcomes. The operating surgeon may choose between closed and open reduction techniques both having its own advantages and disadvantages.
References
- 1.Berry DJ. Epidemiology: Hip and knee. Orthop Clin North Am 1999;30:183-90. [Google Scholar | PubMed]
- 2.Rorabeck CH, Taylor JW. Periprosthetic fractures of the femur complicating total knee arthroplasty. Orthop Clin North Am 1999;30:265-77. [Google Scholar | PubMed]
- 3.Parvizi J, Jain N, Schmidt AH. Periprosthetic knee fractures. J Orthop Trauma 2008;22:663-71. [Google Scholar | PubMed]
- 4.Ritter MA, Faris PM, Keating EM. Anterior femoral notching and ipsilateral supracondylar femur fracture in total knee arthroplasty. J Arthroplasty 1988;3:185-7. [Google Scholar | PubMed]
- 5.Su ET, DeWal H, di Cesare PE. Periprosthetic femoral fractures above total knee replacements. J Am Acad Orthop Surg 2004;12:12-20. [Google Scholar | PubMed]
- 6.Backstein D, Safir O, Gross A. Periprosthetic fractures of the knee. J Arthroplasty 2007;22 Suppl 1:45-9. [Google Scholar | PubMed]
- 7.Chmell MJ, Moran MC, Scott RD. Periarticular fractures after total knee arthroplasty: Principles of management. J Am Acad Orthop Surg 1996;4:109-16. [Google Scholar | PubMed]
- 8.Althausen PL, Lee MA, Finkemeier CG, Meehan JP, Rodrigo JJ. Operative stabilization of supracondylar femur fractures above total knee arthroplasty: A comparison of four treatment methods. J Arthroplasty 2003;18:834-9. [Google Scholar | PubMed]
- 9.Lindahl H, Malchau H, Odén A, Garellick G. Risk factors for failure after treatment of a periprosthetic fracture of the femur. J Bone Joint Surg Br 2006;88:26-30. [Google Scholar | PubMed]
- 10.Giannoudis PV, Kanakaris NK, Tsiridis E. Principles of internal fixation and selection of implants for periprosthetic femoral fractures. Injury 2007;38:669-87. [Google Scholar | PubMed]
- 11.Zdero R, Walker R, Waddell JP, Schemitsch EH. Biomechanical evaluation of periprosthetic femoral fracture fixation. J Bone Joint Surg Am 2008;90:1068-77. [Google Scholar | PubMed]
- 12.Kim KI, Egol KA, Hozack WJ, Parvizi J. Periprosthetic fractures after total knee arthroplasties. Clin Orthop Relat Res 2006;446:167-75. [Google Scholar | PubMed]
- 13.Herrera DA, Kregor PJ, Cole PA, Levy BA, Jönsson A, Zlowodzki M. Treatment of acute distal femur fractures above a total knee arthroplasty: Systematic review of 415 cases (1981-2006) Acta Orthop 2008;79:22-7. [Google Scholar | PubMed]
- 14.Erhardt JB, Grob K, Roderer G, Hoffmann A, Forster TN, Kuster MS. Treatment of periprosthetic femur fractures with the noncontact bridging plate: A new angular stable implant. Arch Orthop Trauma Surg 2008;128:409-16. [Google Scholar | PubMed]
- 15.Jamali AA, Lee MA, Donthineni R, Meehan JP. Minimally invasive management of a floating prosthesis injury with locking plates. J Arthroplasty 2007;22:928-33. [Google Scholar | PubMed]