Debridement and Removal of sequestrum with appropriate antibiotics for 6 weeks gives excellent outcomes in chronic osteomyelitis.
Dr. Pranay Kondewar, Department of orthopedics, Grant Government Medical College, Mumbai, Maharashtra, India. E-mail: pranaypk1@gmail.com
Introduction: Osteomyelitis of the humerus shaft after local skin infection is rare clinical entity, all the principles of tibia and femur osteomyelitis are used in the humerus osteomyelitis. Early detection is best done by the magnetic resonance imaging. Surgical debridement and curettage with IV antibiotics gives good clinical outcome in the patient.
Case Report: A 35-year-old female presented with discharging sinus over posterior aspect of the humerus for 1 year. Diagnosis done based on X-ray and clinical examination. The patient managed with local debridement and saucerization, on follow-up patient is doing all the daily activities and no sign of recurrence at 18 months post-operative.
Conclusion: Local debridement saucerization and course of IV antibiotics according to culture sensitivity give good clinical outcome in cases of humerus osteomyelitis.
Keywords: Humerus, osteomyelitis, bone infections, saucerization, antibiotics.
Bone infections are very difficult to treat and are challenging to deal with for a surgeon. The antibiotics alone give good results against the infections elsewhere in the body but bone infections show variable response because of its physiologic and anatomic characteristics [1]. The standard protocol for surgical intervention in a humerus osteomyelitis is well obtained from the literature available on infections of other long bones such as femur and tibia because the cases of humerus osteomyelitis requiring surgical intervention are not much common in literature and the number of publications is limited [2].
The term osteomyelitis was first used by French surgeon Edouard Chassaignac in 1852 [3]. Compound fractures and open wounds after trauma are the main etiological factors for humerus osteomyelitis. Other etiologies include post-operative infections, spread from local skin infection, and rarely the osteomyelitis after hematogenous seeding of long bones during an episode of bacteremia. Often, osteomyelitis results in the formation of sequestra (termed by John Hunter [4]. In 1764, describing pockets of dead cortical bone with abscess) and involucrum, or new bone formed in response to the sequestrum.
The main reason behind osteomyelitis being difficult to treat is the presence of avascular sequestrum. Treatment is focused on clearing of infection and improving the patient’s functional outcome. Management option for humerus osteomyelitis includes intravenous antibiotics as per culture sensitivity for 6 weeks, when there is a sequestered bone inside one need to remove it by surgical debridement and saucerization, the cavity created can be filled with antibiotic bone cement [5,6]. When active infection is present, antibiotic cement bead can be placed for 6 weeks which elutes antibiotic in area of 2–3 cm around it at concentration very much higher (200 times) than systemic antibiotic [7].
A 35-year-old female came with complaints of localized pain and on and off pus discharge from the wound over the left arm over posterior aspect. The patient was apparently alright 1 year back when she had superficial skin infection (of hair follicle) over the posterior aspect of the arm for which pus drainage was done and antibiotics treatment was given at local hospital. Three months later, she started having pus discharge from the same wound, then she went to another orthopedic surgeon where she underwent surgery for the same. The patient was asymptomatic for few months but again started having pus discharge on and off. On examination, scar mark of previous surgery and a sinus was noted over posterior aspect of the arm 1 cm in size with no active discharge at that time. X-ray showed presence of a sequestered bone in region of humerus shaft extending distally for about 5 cm (Fig. 1). Erythrocyte sedimentation rate and C-reactive protein were mildly elevated. The patient was then planned for debridement and saucerization.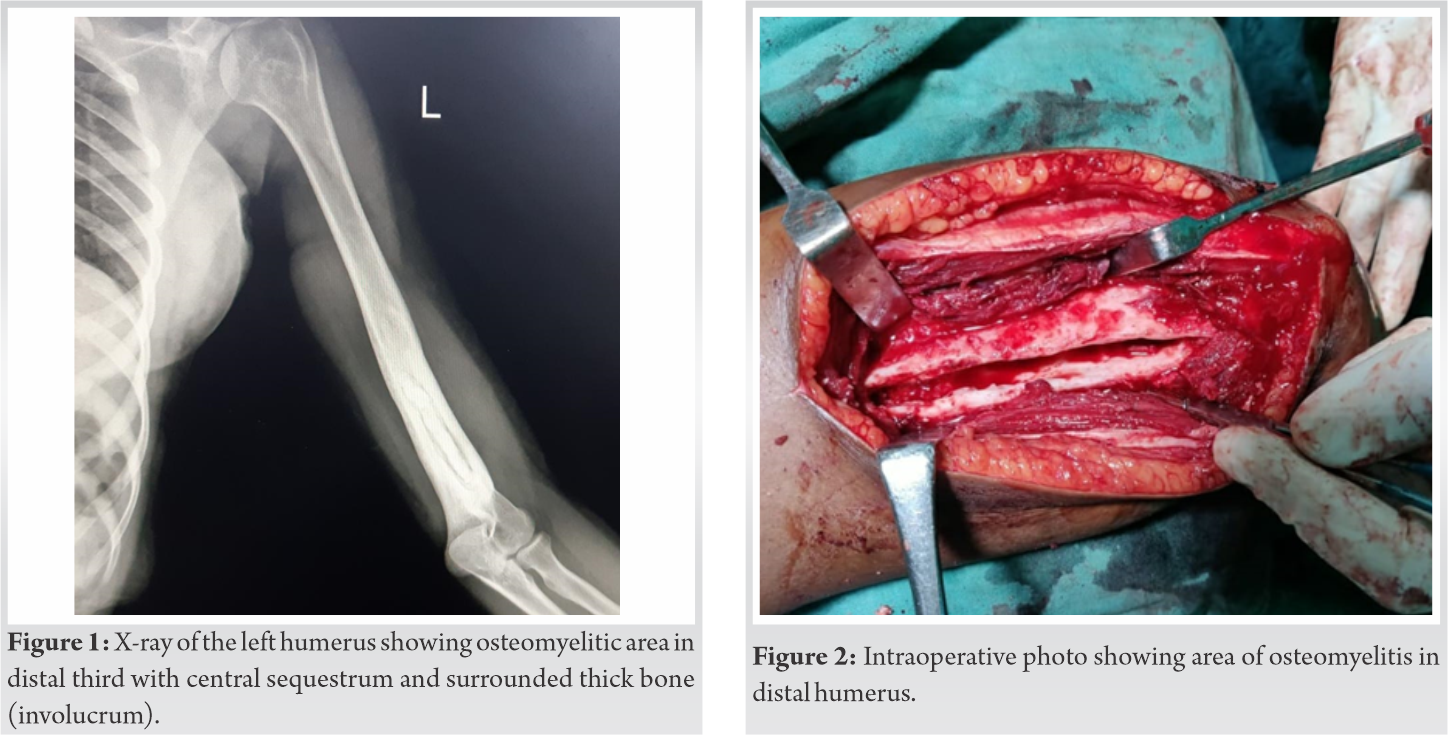
The patient was operated in lateral decubitus position under regional anesthesia, posterior approach for humerus was used, on exposure, pus pockets were noticed in muscle plane and sinus tract traced down till posterior surface of bone. Radial nerve was isolated and kept protected throughout the surgery. Cortical window was created 3 cm in diameter and debridement and curettage was done (Fig. 2). Till, paprika sign is seen. Sequestered bone was removed and sent for histopathological analysis and culture sensitivity. Sinus tract excised and betadine wash was given, drain was put and wound closed in layers. In post-operative period, arm was immobilized till suture removal (Fig. 3). 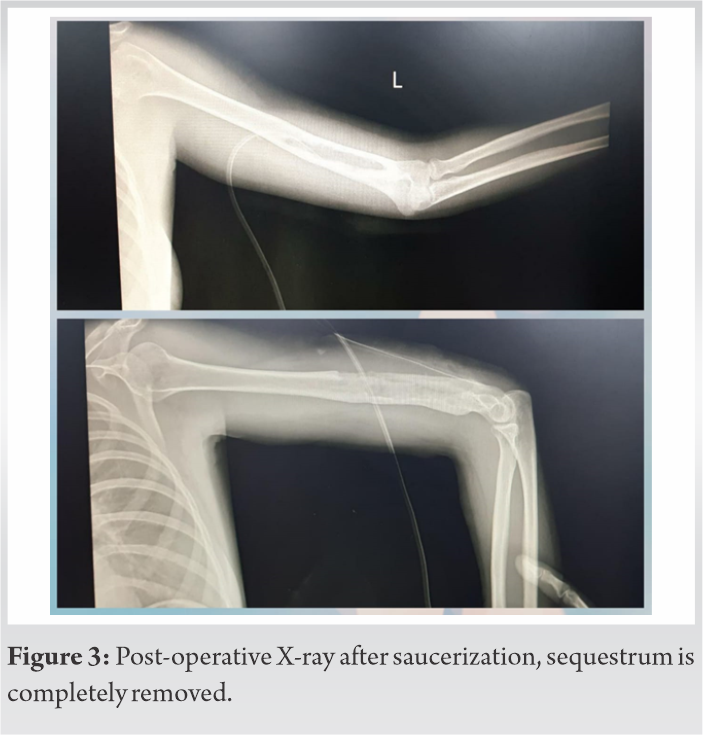 Attention was given to nutritional supplements and protein deficit to improve immunity and host response.
Attention was given to nutritional supplements and protein deficit to improve immunity and host response.
Drain removed on day 3 and suture removal on day 10. Culture showed Staphylococcus aureus and intravenous antibiotics (piperacillin and tazobactam) were given as per sensitivity for 6 weeks. Protected mobilization started after suture removal increased gradually, 6 monthly follow-up was taken and there is no recurrence till now (post-operative 18 months). The patient is doing all the daily activities without any problem. Recent X-ray shows previous cavity being filled with bone formation (Fig. 4 and 5).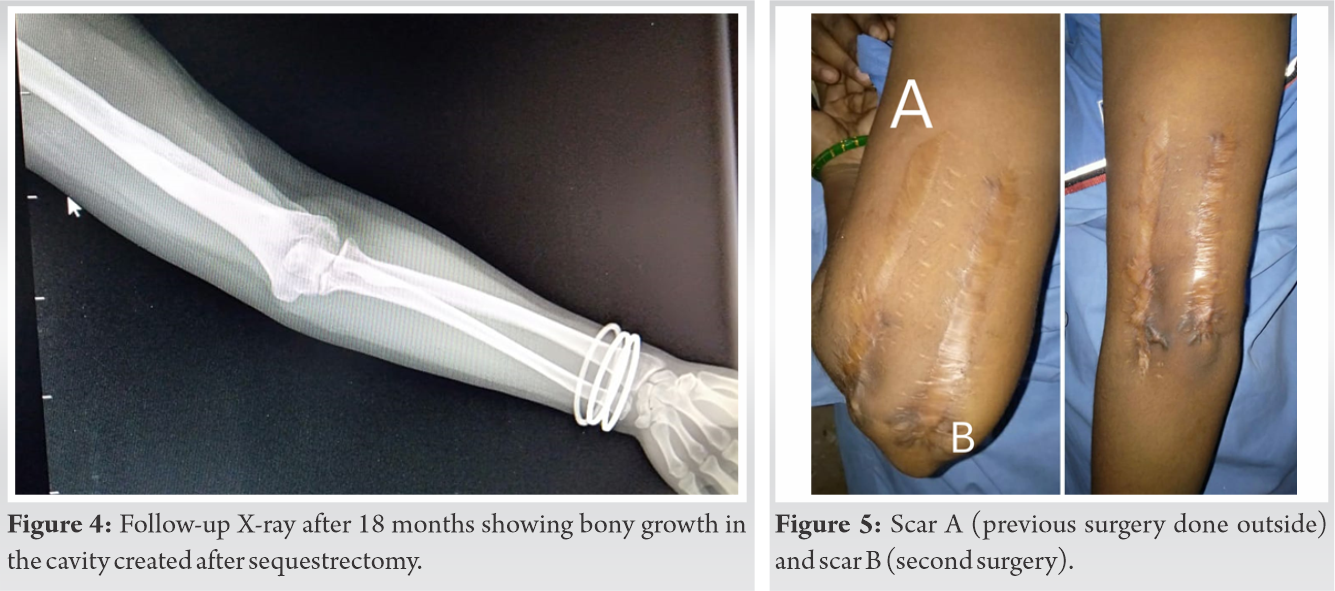
Osteomyelitis of long bones can be secondary to trauma after compound wounds as seen in adults or can be due to hematogenous spread of the bacteria from another site in body as seen in children.
Osteomyelitis involving humerus is rare clinical entity and management is derived from osteomyelitis involving tibia and femur, the overall incidence is 3.4% [8]. The patient presented with osteomyelitis secondary to local skin and soft-tissue infection which is less common than the post-traumatic forms presented in the literature [9]. Most of the case of osteomyelitis are managed with antibiotics alone, but when there is wide involvement and infection is chronic; surgical management is needed to remove foci of infection that is sequestrum.
The sequestrum is the nidus of infection, and due to its avascular nature, antibiotics do not reach till there and bacteria continue to replicate and may develop antibiotics resistance. The sinus tract should be completely excised. Care should be taken while performing bony debridement as excessive bone removal can lead to loss of structural support and fracture and inadequate removal can cause recurrence of the infection, clearing of infection should be the main priority. Surgeon should keep in mind about the need of giving structural support in the form of plate or bone graft if more bone is to be removed. One may place antibiotics cement beads for local drug delivery. The 4–6 weeks of duration of antibiotics are based on the fact it takes time for bone to revascularize after debridement.
The cavity created after saucerization may be filled with antibiotic bone cement, vascularized or non-vascularized fibula bone graft, local muscle flap, or can be left as it is provided that soft-tissue cover is adequate. A normal drain or continuous suction irrigation drain can be placed depending on level of contamination and infection. When the cortical bone is weakened after removal of sequestrum; additional support in the form of plating using (dynamic compression plate) or external fixator can be given to avoid fractures.
Surgical debridement relying on the Cierny-Mader classification and staged approach is general guides for the management of chronic osteomyelitis [10,11]. While treating humerus osteomyelitis, anatomic advantages are a good soft-tissue envelope and good blood supply which helps in early healing. A care should be taken to avoid the iatrogenic damage to the radial nerve. Magnetic resonance imaging (MRI) and radio nucleotide scan give early diagnosis in cases of osteomyelitis [12]. In this case, it was not done as history and clinical evidences were adequate enough.
Osteomyelitis after local soft-tissue infection is very rare, especially in upper limbs. MRI is very helpful in early detection of infection. Management includes IV antibiotics with or without local debridement in early cases. In chronic osteomyelitis, one needs to remove the infective foci, the sequestrum, and excise the draining sinus tract. Humerus having adequate soft-tissue cover and blood supply shows good outcome with simple saucerization and antibiotics treatment and gives good clinical results.
Osteomyelitis involving long bones like humerus is managed with intravenous antibiotics alone, when involving active pus discharge with dead sequestrum inside, surgical treatment is more promising and gives good results.
References
- 1.Lew DP, Waldvogel FA. Osteomyelitis. Lancet 2004;364:369-79. [Google Scholar | PubMed]
- 2.Ferreira N, Marais LC, Serfontein C. Two stage reconstruction of septic non-union of the humerus with the use of circular external fixation. Injury 2016;47:1713-8. [Google Scholar | PubMed]
- 3.Chassaignac E. De l’osteo-Myelite. Paris: Bull Mem Soc Chir 1852. p. 431-6. [Google Scholar | PubMed]
- 4.Hunter J. A Treatise on the Blood, Inflammation and Gun-shot Wounds. London: George Nicol; 1764. p. 521-67. [Google Scholar | PubMed]
- 5.5. Zalavras CG, Patzakis MJ, Holtom P. Local antibiotic therapy in the treatment of open fractures and osteomyelitis. Clin Orthop Relat Res 2004;427:86-93. [Google Scholar | PubMed]
- 6.Pan C, Zhou Z, Yu X. Coatings as the useful drug delivery system for the prevention of implant-related infections. J Orthop Surg Res 2018;13:220. [Google Scholar | PubMed]
- 7.Conterno LO, da Silva Filho CR. Antibiotics for treating chronic osteomyelitis in adults. Cochrane Database Syst Rev 2009;3:CD004439. [Google Scholar | PubMed]
- 8.Wu H, Yu S, Fu J, Sun D, Wang S, Xie Z, et al. Investigating clinical characteristics and prognostic factors in patients with chronic osteomyelitis of humerus. Burn Trauma 2019;7:34. [Google Scholar | PubMed]
- 9.Birt MC, Anderson DW, Bruce Toby E, Wang J. Osteomyelitis: Recent advances in pathophysiology and therapeutic strategies. J Orthop 2016;14:45-52. [Google Scholar | PubMed]
- 10.McNally MA, Small JO, Tofighi HG, Mollan RA. Two-stage management of chronic osteomyelitis of the long bones. The Belfast technique. J Bone Joint Surg Br 1993;75:375-80. [Google Scholar | PubMed]
- 11.Cierny G 3rd, Mader JT, Penninck JJ. A clinical staging system for adult osteomyelitis. Clin Orthop Relat Res 2003;414:7-24. [Google Scholar | PubMed]
- 12.Jaramillo D. Infection: Musculoskeletal. Pediatr Radiol 2011;41 Suppl 1:S127-34. [Google Scholar | PubMed]