Presentation of a rare systemic disease; Management of the progressive degenerative arthropathy of alkaptonuria.
Dr. Carolina Tiago Afonso, Department of Orthopaedics and Traumatology, Unidade Local de Saúde Nordeste, Rua Antero Quental 2, 5340-232, Macedo de Cavaleiros, Portugal. E-mail: carolinatiagoafonso@gmail.com
Introduction: Alkaptonuria (AKU) is a rare autosomal recessive disorder in which tyrosine metabolism is altered. There is a deficiency of the Homogentisate 1,2-dioxygenase enzyme (homogentisic acid oxidase) This enzyme is responsible for the metabolism of the tyrosine - homogentisic acid - in maleylacetoacetic acid. Accumulation of homogenous acid occurs in urine and conjunctival tissue in the second with important deleterious effects on cartilage and bone. The most limiting complication is progressive degenerative arthropathy, especially in the axial and load load-bearing joints, with a lower tendency to affect the shoulder. Because of its rarity little is known about the results of arthroplasties in these patients.
Case Report: A 60 -years -old man, retired, with a history of right knee arthroplasty 6 years ago (performed in another hospital). Sent to the orthopedic consultation due to intense shoulder pain. The case was revealed to be a rare disease: arthropathy due AKU. He was treated with total shoulder reverse arthroplasty. Currently with two 2 years of follow-up, with excellent functional results.
Conclusion: The most commonly performed procedure, in this patients, is the hip prosthesis and there are few reported cases of shoulder arthroplasty. However, the results of our follow follow-up are good and encouraging.
Keywords: Alkaptonuria; , shoulder arthropathy; , total shoulder reverse arthroplasty.
Alkaptonuria (AKU) is a rare inherited autosomal recessive disease [1]. It can rarely be transmitted in an autosomal dominant manner [2]. It was the first autosomal recessive disease that proved to follow a Mendelian distribution [3]. It has an incidence of 1: 250,000–1,000,000, being more common in certain areas of Eastern Europe and the Dominican Republic [1,4,5]. It also affects men as women, although this disease appears to have more manifestations in men [2]. In this disease, tyrosine metabolism is altered with a deficiency of the homogentisic 1,2-oxidase acid (HGO) [6], whose gene is located in band 2 of the long arm of chromosome 3 (3q2) [1]. At least 129 mutations in the HGO gene are known, and all produce the AKU phenotype. There appears to be no correlation between the type of mutation and the severity of the phenotype [7]. This enzyme is responsible for the metabolism of the intermediate tyrosine-homogenous acid in maleylacetoacetic acid. Homogeneous acid accumulation occurs in urine and connective tissue – in the latter, with important deleterious effects on cartilage and bone. In the cartilaginous tissue, the homogentisic acid breaks down the crosslinks of the collagen, which, in turn, leads to erosions of the cartilage with subsequent early degenerative changes [8]. Clinically is characterized by the triad: dark urine (present birth), ochronosis that refers to the connective tissue of bluish pigmentation (beginning between 20 and 30 years) [9], and arthritis (present in approximately 40 years). Ocrose has been first described in 1866 by Virchow [10]. The most limiting complication is progressive degenerative arthropathy, especially in the axial and load joints, with a lower tendency to affect the shoulder [11]. Due to its rarity, little is known about the results of arthroplasties in these patients. The most commonly performed is the hip prosthesis and there are few reported cases of shoulder arthroplasty. However, the results of your follow-up are good and encouraging. We present a case report of shoulder arthropathy in a patient with alcaptonuria treated with a reverse shoulder arthroplasty.
A 60-year-old man, retired, with a personal history of right knee arthroplasty 6 years ago (performed in another hospital). Sent to the Orthopedic consultation due to intense bilateral, long-term oxygenesis, worse to the right, incapacitating, that did not give in to analgesics. On objective examination, he had shoulders with rigidity and limited mobility. The Rx showed important signs of arthrosis (Fig. 1), and was therefore proposed for total shoulder prosthesis. Intraoperatively, there was extensive bone and soft tissue invasion of dark material of unknown etiology. Soft tissues and bone samples were collected for anatomopathological study. It was decided to abort the procedure until a definitive diagnosis was made. Magnetic resonance imaging of the shoulder was requested (Fig. 2), which was inconclusive. The result of the pathological anatomy revealed only venous hemangioma.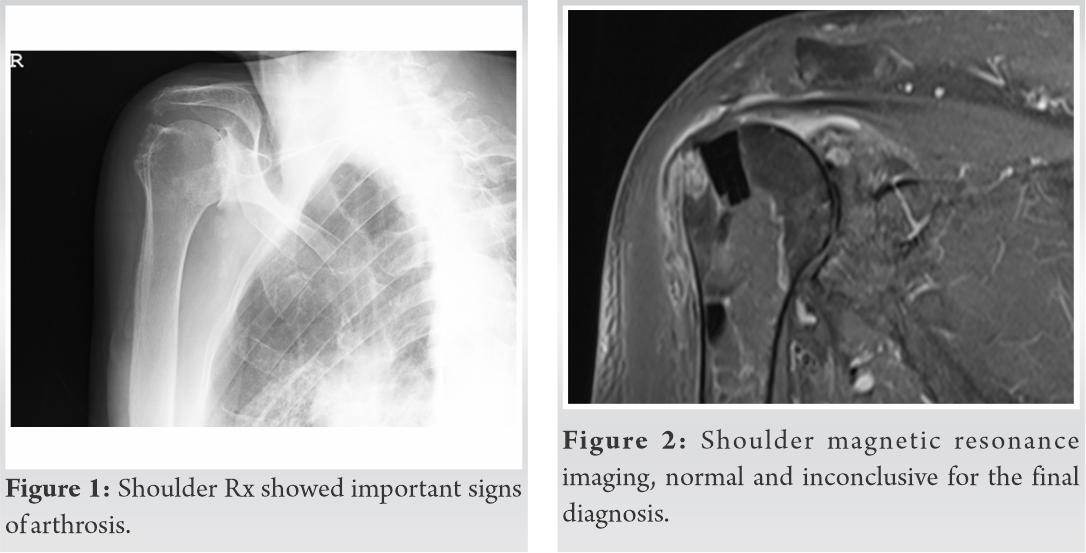 At the follow-up visit, the patient revealed a previously unknown personal history: a brother diagnosed with AKU followed in another hospital. Given the maintenance of painful complaints and after review of the literature, it was decided to perform total reverse shoulder prosthesis (TSRA) (Fig. 3 and 4).
At the follow-up visit, the patient revealed a previously unknown personal history: a brother diagnosed with AKU followed in another hospital. Given the maintenance of painful complaints and after review of the literature, it was decided to perform total reverse shoulder prosthesis (TSRA) (Fig. 3 and 4).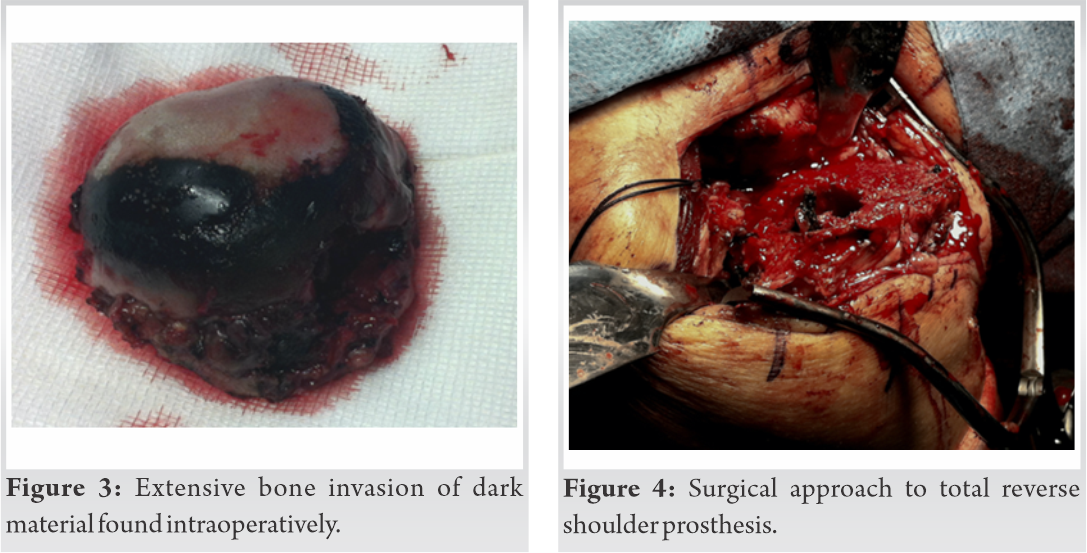 The procedure went well, with optimal postoperative radiological result (Fig. 5). The patient started passive mobilization exercises in the postoperative period and later followed a physical rehabilitation program. After 3 years of TSRA there was no record of complications.
The procedure went well, with optimal postoperative radiological result (Fig. 5). The patient started passive mobilization exercises in the postoperative period and later followed a physical rehabilitation program. After 3 years of TSRA there was no record of complications.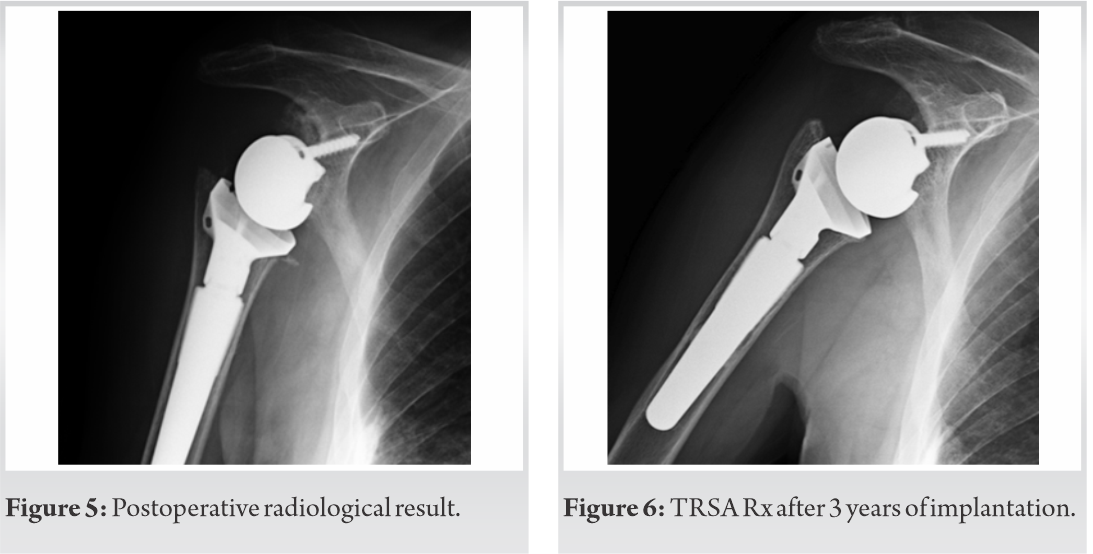 Clinically and functionally, the patient does not present pain relief complaints. It presents a Constant Score of 10 points (excellent) and American Shoulder and Elbow Score of 78 points. Radiologically, the prosthesis remains stable (Fig. 6), osseointegrated, with no signs of detachment or infection, and does not appear to be affected by ochronosis.
Clinically and functionally, the patient does not present pain relief complaints. It presents a Constant Score of 10 points (excellent) and American Shoulder and Elbow Score of 78 points. Radiologically, the prosthesis remains stable (Fig. 6), osseointegrated, with no signs of detachment or infection, and does not appear to be affected by ochronosis.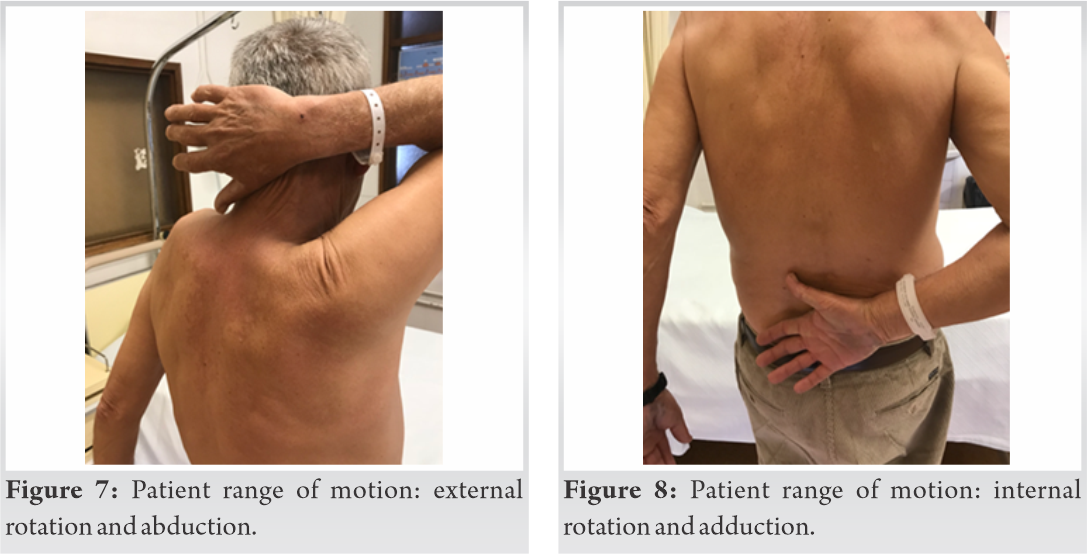 The patient is able to do his daily life activities without pain (Fig. 7-10).
The patient is able to do his daily life activities without pain (Fig. 7-10).
The ACU courses with the accumulation of homogentisic acid, in the form of dark blue pigmentation in the connective tissue with loss of its elasticity and in the cartilage with progression to arthropathy. Patients are generally asymptomatic up to the fourth decade of life [1] at which point changes in urine, arthritis in the large joints, and a lumbar spine with joint stiffness begin. This seems to be explained by the fact that the tubular excretion of homogentisic acid is effective in the young. With aging, the excretion processes deteriorate, accumulation of homogenous acid is more rapid with subsequent accumulation of the pigment in the cartilages [12]. In our case, the patient complained of long-standing and disabling malaise. ACU’s tendency to affect the shoulder in a very severe manner, with very intense and disabling pain, distinguishes it from osteoarthrosis [11]. The extra-articular manifestations are bluish pigmentation of the ears, sclera and skin, dark urine after contact with the ambient air, and aortic stenosis. The results obtained are favorable, however, the follow-up period is still short. There were resolution of painful complaints and functionally the patient is evolving well, due to their low functional demands. The results of arthroplasty of the shoulder by arthropathy caused by alcaptonuria are similar to those of shoulder arthroplasties due to primary osteoarthrosis or cochlear arthropathy.
The prosthesis does not appear to be affected by the accumulation of homogentisic acid.
Although there is no curative treatment for this disease, shoulder arthroplasty seems to be the definitive effective treatment for the arthropathy of the shoulder by alcaptonuria. This treatment improves patients’ quality of life by eliminating pain and improving joint function.
AKU is a rare disease that mainly affects the weight-bearing joints, with less tendency to affect the shoulder. It is important to recognize this arthropathy and treat it. Arthroplastic replacement is an effective treatment that improves the patient’s quality of life.
References
- 1.Mannoni A, Selvi E, Lorenzini S, Giorgi M, Airo P, Cammelli D, et al. Alkaptonuria, ochronosis and ochronotic arthropathy. Semin Arthritis Rheum 2004;33:239-48. [Google Scholar | PubMed]
- 2.Aynasi O, Onder C, Turhan AU. Bilateral hip arthtropaplasty for ochronic arthropathy. Clin Rheumatol 2000;19:150-2. [Google Scholar | PubMed]
- 3.Garrod E. The incidence of alkaptonuria: A study in chemical individuality. Lancet 1902;2:1616-20. [Google Scholar | PubMed]
- 4.Janocha S, Wolz W, Srsen S, Srsnova K, Montagutelli X, Guenet JL, et al. The human gene for alkaptonuria (AKU) maps to chromosome 3q. Genomics 1994;19:5-8. [Google Scholar | PubMed]
- 5.Demir S. Alkaptonuric ochronosis: A case with multiple joint replacement arthroplasties. Clin Rheumatol 2003;22:437. [Google Scholar | PubMed]
- 6.Phornphutkul C, Introne WJ, Perry MB, Bernardini I, Murphey MD, Fitzpatrick DL, et al. Natural history of alkaptonuria. N Engl J Med 2002;347:2111-21. [Google Scholar | PubMed]
- 7.Nemethova M, Radvanszky J, Kadasi L, Ascher DB, Pires DE, Blundell TL, et al. Twelve novel HGD gene variants identified in 99 alkaptonuria patients: Focus on ‘black bone disease’ in Italy. Eur J Hum Genet 2016;24:66-72. [Google Scholar | PubMed]
- 8.Tracker M, Gurude S, Puri A. Ochronotic arthropathy: Arthroscopic findings in the shoulder and the knee. Arthroscopy 2003;19:E70. [Google Scholar | PubMed]
- 9.Wagner LR, Knott JL, Machaffie RA, Walsh JR. Clinical and pathological findings in ochronosis. J Clin Pathol 1960;13:22-6. [Google Scholar | PubMed]
- 10.Laskar FH, Sargison KD. Ochronotic arthropathy. J Bone Joint Surg Br 1970;52:653-66. [Google Scholar | PubMed]
- 11.Fisher AA, Davis MW. Alkaptonuric ochronosis with aortic valve and joint replacements and femoral fracture. Clin Med Res 2004;2:209-15. [Google Scholar | PubMed]
- 12.Hamdi N, Cooke TD, Hassan B. Ochronotic arthropathy: Case report and review of the literature. Int Orthop 1999;23:122-5. [Google Scholar | PubMed]