Gaucher’s disease may mimic a primary bone tumor or metastasis and one should have a high index of suspicion in patients with multiple osteolytic lesions without any significant past history amongst patients of non-Ashkenazi Jewish descent.
Dr. Syed Hifzur Rahman, Department of Orthopaedics, Pandit Madan Mohan Malviya Shatabdi Centenary Hospital, Mumbai, Maharashtra, India. E-mail: drsyedhifzurrahman@gmail.com
Introduction: Gaucher’s disease is a congenital lysosomal storage disorder caused by an autosomal recessive mutation in B-glucocerebrosidase. It is a multi-system disease, wherein patients present with hematological abnormalities, joint pain, osteonecrosis, and developmental delay. We present a case of 38-year-old male with a painless solitary soft-tissue swelling over the left proximal tibia, eventually diagnosed it to be a case of Gaucher’s disease. This case is unique in the literature, because this subcutaneous Gaucher mass was not associated with a significant past history and was being evaluated as a standard approach to a bone tumor.
Case Presentation: A 38-year-old man presented to our outpatient department with a solitary, painless soft-tissue swelling of the left proximal tibia noticed 6 months back, which has gradually progressed to a present size of 9x5 cm over a period of 6 months. General physical examination revealed moderate splenomegaly. Radiographs showed an osteolytic lesion in the left proximal tibia without cortical erosion. Radiographs for skeletal survey revealed similar osteolytic lesions elsewhere. Hematological investigations revealed thrombocytopenia. A serum protein electrophoresis was found to be normal and the urine was negative for myeloma proteins. Blood workup for endocrine abnormalities was within normal limits. MRI of the lesion suggests bone infarct. Biopsy from the lesion showed a giant binucleate storage cell filled with glucocerebrosides suggestive of Gaucher’s disease. The diagnosis was confirmed by elevated plasma levels of glucocerebrosidases.
Conclusion: Gaucher’s disease is a rare metabolic disease of the bone which may mimic a primary bone tumor or metastasis. A step-wise meticulous approach with biopsy and elevated plasma levels of glucocerebrosidase helps establish the diagnosis. Once must have a high index of suspicion for Gaucher’s disease in an adult with multiple osteolytic lesions without any significant past medical and surgical history.
Keywords: Gaucher’s disease, lysosomal storage disease, autosomal recessive mutation, solitary musculoskeletal swelling, multiple osteolytic lesions, bone infarcts, soft-tissue mass, enzyme replacement therapy.
At present, there are more than 45 lysosomal storage disorders, of which Gaucher’s disease is the most prevalent in India and worldwide [1]. Gaucher’s disease is an autosomal recessive disorder, where the metabolic defect is due to an inherited deficiency of glucocerebrosidase caused by a mutation in the GBA1 (acid-β-glucosidase) gene causing accumulation of an abnormal lipid glucocerebroside in the lysosome of macrophages, leading to a wide spectrum of phenotypic manifestations [2]. There is a striking variation in its clinical manifestations, severity and course of the disease with different bone involvements can be confused with hematological diseases, infections, and malignancy. There are six different bony manifestations of Gaucher disease – bone marrow infiltration, avascular necrosis, bone crisis, pathological fractures, lytic lesions, and osteomyelitis [3]. We describe a case of Gaucher cell deposition in the subcutaneous soft-tissues overlying the proximal tibia mimicking neoplasm in an 38-year-old man without any significant past history.
A 38-year-old patient presented to us with a painless solitary swelling, over left upper leg (Fig. 1) which was insidious in onset, gradually progressed over a period of 6 months to present size of 9 x 5 cm. No other associated symptoms. No history of swelling elsewhere in the body. Clinically, there was no local warmth, tenderness, or crepitus. It was firm in consistency and uniform throughout. The range of motion at the knee joint was normal and painless.  Systemic examination revealed moderate splenomegaly. There were no palpable lymph nodes. Regional radiographs revealed a large lytic lesion with well-defined margins with narrow zone of transition without cortical breech or periosteal reaction in the metaphysio-diaphyseal region of left proximal tibia (Fig. 2). It was associated with diffuse osteopenia. Radiographs of skeletal survey revealed similar osteolytic lesions in both femur shaft, both proximal humerus and contralateral tibia (Fig. 3). There were no lytic lesions in the skull and the spine. Chest radiograph did not show any evidence of metastasis (Fig. 4). Laboratory investigations revealed thrombocytopenia. Hemoglobin, total leucocyte count, differential leucocyte count, total protein, serum creatinine, blood urea, serum calcium, and potassium were within normal limits. ESR and CRP were normal. Serum electrophoresis study was within normal limits, and the urine was negative for myeloma protein. Regional MRI of tibia showed ill-defined serpiginous areas of heterogenous T2 hyperintensity and T1 hypointensity involving left proximal tibia (Fig. 5).
Systemic examination revealed moderate splenomegaly. There were no palpable lymph nodes. Regional radiographs revealed a large lytic lesion with well-defined margins with narrow zone of transition without cortical breech or periosteal reaction in the metaphysio-diaphyseal region of left proximal tibia (Fig. 2). It was associated with diffuse osteopenia. Radiographs of skeletal survey revealed similar osteolytic lesions in both femur shaft, both proximal humerus and contralateral tibia (Fig. 3). There were no lytic lesions in the skull and the spine. Chest radiograph did not show any evidence of metastasis (Fig. 4). Laboratory investigations revealed thrombocytopenia. Hemoglobin, total leucocyte count, differential leucocyte count, total protein, serum creatinine, blood urea, serum calcium, and potassium were within normal limits. ESR and CRP were normal. Serum electrophoresis study was within normal limits, and the urine was negative for myeloma protein. Regional MRI of tibia showed ill-defined serpiginous areas of heterogenous T2 hyperintensity and T1 hypointensity involving left proximal tibia (Fig. 5).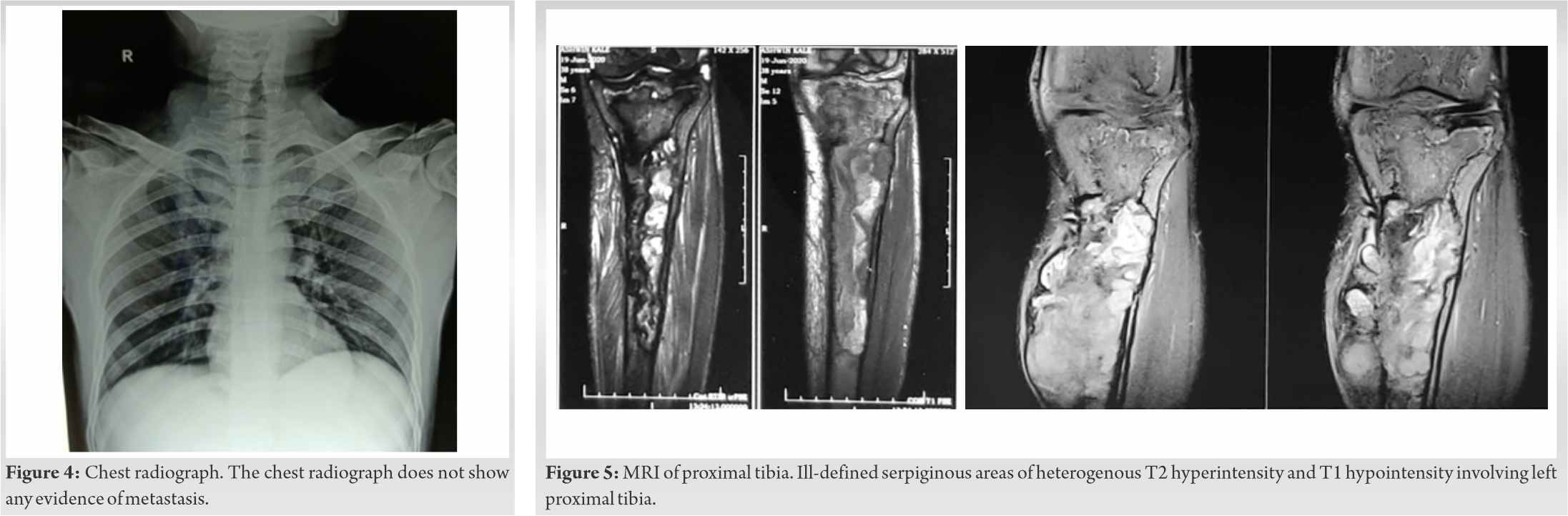 On post-contrast study, these areas show heterogenous enhancement. In the given clinical setting, the above findings were suggestive of bone infarcts. Cortical destruction and irregularity seen. Heterogenous T2 hyperintense and T1 hypointense subcutaneous collection was seen along the anterior aspect of the left tibia and seen communicating with marrow cavity through above-mentioned cortical defect. Finally, a biopsy was planned from the most representative part of the swelling. Four core samples were obtained using an 18-gauge biopsy device which showed confluent proliferation of well-demarcated giant binucleate storage cells bearing small, irregular nuclei, and fibrillary cytoplasm reminiscent of “wrinkled tissue paper” on hematoxylin and eosin staining filled with glucocerebrosides suggestive of Gaucher’s disease (Fig. 6).
On post-contrast study, these areas show heterogenous enhancement. In the given clinical setting, the above findings were suggestive of bone infarcts. Cortical destruction and irregularity seen. Heterogenous T2 hyperintense and T1 hypointense subcutaneous collection was seen along the anterior aspect of the left tibia and seen communicating with marrow cavity through above-mentioned cortical defect. Finally, a biopsy was planned from the most representative part of the swelling. Four core samples were obtained using an 18-gauge biopsy device which showed confluent proliferation of well-demarcated giant binucleate storage cells bearing small, irregular nuclei, and fibrillary cytoplasm reminiscent of “wrinkled tissue paper” on hematoxylin and eosin staining filled with glucocerebrosides suggestive of Gaucher’s disease (Fig. 6).  The diagnosis was confirmed by elevated plasma levels of glucocerebrosidase. The treatment basically involves a multidisciplinary approach to address orthopedic manifestations, hematologic abnormalities and neurologic abnormalities in a few subset of patients. Enzyme replacement therapy is the crux of treatment in our case. Following biopsy, the decision was made to follow this lesion clinically and to maintain the patient on the baseline level of enzyme therapy. Given the unique quality of this case, the anticipated natural course of this mass in the absence of additional treatment is not known. Further, evaluation with regular follow-up with imaging will be required if the mass undergoes any clinical changes.
The diagnosis was confirmed by elevated plasma levels of glucocerebrosidase. The treatment basically involves a multidisciplinary approach to address orthopedic manifestations, hematologic abnormalities and neurologic abnormalities in a few subset of patients. Enzyme replacement therapy is the crux of treatment in our case. Following biopsy, the decision was made to follow this lesion clinically and to maintain the patient on the baseline level of enzyme therapy. Given the unique quality of this case, the anticipated natural course of this mass in the absence of additional treatment is not known. Further, evaluation with regular follow-up with imaging will be required if the mass undergoes any clinical changes.
Bony manifestations in Gaucher’s disease are common, but extraosseous extension is unusual.
Extraosseous Gaucher cell deposits are a rare feature of Gaucher’s disease that can mimic malignancy [4]. The osseous manifestations of Gaucher’s disease are the major determinants of morbidity and functional outcome in those affected [5]. Most cases of bone involvement with extraosseous extension have been described in type I Gaucher disease which is the most common type [6]. Type I disease accounts for more than 99% of Gaucher disease cases, which spares the central nervous system and is often diagnosed later in life. As such, its primary manifestations are often due to bone marrow replacement and ensuing hematopoietic effects or bony deformity or fracture [7]. Type II and III Gaucher disease are both characterized by neurologic involvement. Type III Gaucher’s disease carries a less favorable prognosis and progresses more rapidly than type II. Types II and III are rare and do not demonstrate any ethnic predilection, in contrast to the increased incidence of type I disease amongst patients of Ashkenazi Jewish descent [8]. The medullary expansion is related to the replacement of the bone marrow by Gaucher cells manifesting as an enlargement of the bone shaft and cortical thinning. In rare instances, the expansion of the medullary cavity may lead to cortical destruction and may result in the extraosseous extension of Gaucher cell deposits mimicking malignancy [9]. In such instances, a meticulous step-wise examination helps in the establishment of the diagnosis and decreases the incidence of errors especially when there is not significant history suggestive of Gaucher’s disease. An approach to a solitary musculoskeletal swelling should be followed. A biopsy should be done only after clinical and radiological diagnosis is established and biopsy is used to confirm the diagnosis rather than establishing the diagnosis as a shortcut [10]. Observation and supportive therapy is the mainstay in the absence of pathological fracture and disabling deformity. As the patient is highly prone for pathological fractures, fracture management requires pre-operative optimization with enzyme therapy [11]. Availability of additional blood, clotting factors, and platelets due to increased bleeding risk and the anesthesiologist to maintain adequate oxygenation to avoid precipitating bone crisis [12]. There is also an increased risk of infection in such patients [13].
Gaucher’s disease is a rare metabolic disease of the bone which may mimic a primary bone tumor or metastasis. It can be a rare cause of a solitary musculoskeletal swelling in an adult without any history suggestive of Gaucher’s disease. A step-wise meticulous approach with general physical examination, radiology, hematology, and finally biopsy and elevated plasma levels of glucocerebrosidase helps establish the diagnosis. Once must have a high index of suspicion for Gaucher’s disease in an adult with multiple osteolytic lesions without any significant medical and surgical history.
Solitary musculoskeletal swelling requires a meticulous step-wise approach to arrive at a diagnosis. Gaucher’s disease may mimic a primary bone tumor or metastasis and one should have a high index of suspicion in patients with multiple osteolytic lesions without any significant history amongst patients of non-Ashkenazi Jewish descent.
References
- 1.Nagral A. Gaucher disease. J Clin Exp Hepatol 2014;4:37-50. [Google Scholar | PubMed]
- 2.Stirnemann J, Belmatoug N, Camou F, Serratrice C, Froissart R, Caillaud C, et al. A review of Gaucher disease pathophysiology, clinical presentation and treatments. Int J Mol Sci 2017;18:441. [Google Scholar | PubMed]
- 3.Goldblatt J, Sacks S, Beighton P. The orthopedic aspects of Gaucher disease. Clin Orthop Relat Res 1978;137:208-14. [Google Scholar | PubMed]
- 4.Meyer BJ, Mills AM, Gaskin CM. Extraosseous Gaucher cell deposition without adjacent bone involvement. Skeletal Radiol 2014;43:1495-8. [Google Scholar | PubMed]
- 5.Cox TM, Schofield JP. Gaucher’s disease: Clinical features and natural history. Baillieres Clin Haematol 1997;10:657-89. [Google Scholar | PubMed]
- 6.Mikosch P, Hughes D. An overview on bone manifestations in Gaucher disease. Wien Med Wochenschr 2010;160:609-24. [Google Scholar | PubMed]
- 7.Wenstrup RJ, Roca-Espiau M, Weinreb NJ, Bembi B. Skeletal aspects of Gaucher disease: A review. Br J Radiol 2002;75:A2-12. [Google Scholar | PubMed]
- 8.Nalysnyk L, Rotella P, Simeone JC, Hamed A, Weinreb N. Gaucher disease epidemiology and natural history: A comprehensive review of the literature. Hematology 2017;22:65-73. [Google Scholar | PubMed]
- 9.Manz M, Riessen R, Poll L, Dohmen B, Kaiserling E, Krück W, et al. High‐grade lymphoma mimicking bone crisis in Gaucher’s disease. Br J Haematol 2001;113:191-3. [Google Scholar | PubMed]
- 10.Agarwal MG, Nayak P. Management of skeletal metastases: An orthopaedic surgeon’s guide. Indian J Orthop 2015;49:83-100. [Google Scholar | PubMed]
- 11.Pastores GM, Patel MJ, Firooznia H. Bone and joint complications related to Gaucher disease. Curr Rheumatol Rep 2000;2:175-80. [Google Scholar | PubMed]
- 12.Pastores GM, Weinreb NJ, Aerts H, Andria G, Cox TM, Giralt M, et al. Therapeutic goals in the treatment of Gaucher disease. In: Seminars in Hematology. Vol. 41. United States: WB Saunders; 2004. p. 4-14. [Google Scholar | PubMed]
- 13.Noyes FR, Smith WS. Bone crises and chronic osteomyelitis in Gaucher’s disease. Clin Orthop Relat Res 1971;79:132-40. [Google Scholar | PubMed]