Rupture of the quadriceps post-TKR in a morbidly obese patient can be managed successfully by early diagnosis, surgical management using suture anchors, and a guarded physiotherapy regimen.
Dr. Amyn M Rajani, Consultant Orthopaedic Surgeon, M.S. Orthopaedics, OAKS Clinic, 707 Panchshil Plaza, N S Patkar Marg, opp. Ghanasingh Fine Jewels, Next to Dharam Palace, Gamdevi, Mumbai, Maharashtra, India. E-mail: dramrajani@gmail.com
Introduction: Quadriceps rupture after a total knee arthroplasty is a rare complication. In addition, morbid obesity confounds the early diagnosis of any loss of function of the extensor mechanism. Poor tendon quality, fraying, and retraction of the tendon pose a distinctive challenge while repair, predisposing it to failure. The literature is devoid of reports highlighting this complication in a morbidly obese patient and its subsequent successful management.
Case Report: Through this case, we report a morbidly obese 71-year-old who underwent an uneventful left sided total knee arthroplasty and suffered from an atraumatic quadriceps rupture on post-operative day 17. The diagnosis was confirmed on ultrasound followed by magnetic resonance imaging. An innovative technique of repair incorporating two, 5 mm suture anchors for fixing the ruptured quadriceps into the patella, and subsequent fortification of the repair was undertaken, followed by a guarded physiotherapy regimen. At 10 weeks post-repair, the patient started walking without any assistive device and achieved excellent clinical and functional outcome without any complications.
Conclusion: Post-total knee arthroplasty quadriceps rupture is a rare but dangerous complication, even more so in a morbidly obese patient due to the inherent weakness of the muscles and tendons. Timely diagnosis and adequate repair using the innovative technique described in this study, along with a guarded physiotherapy regimen that can help in dealing with such complications successfully, as shown in this case.
Keywords: Quadriceps, rupture, repair, total knee replacement, total knee arthroplasty, complication, suture anchor, acute, obese.
Total knee arthroplasty (TKA) has been established as the go-to treatment modality for favorable long-term clinical and radiological outcomes in patients with severe, tricompartmental osteoarthritis of the knee joint [1,2]. Precise bone cuts, balancing of soft tissues, as well as proper implant placement, are the keys to achieving good outcomes. An array of complications may follow a TKA due to various factors; however, quadriceps rupture, despite its minuscule prevalence of 0.29% in the early post-operative period, is one of the most feared and potentially debilitating complication [3,4,5]. The condition can be prevented by maintaining the integrity of the quadriceps tendon, while simultaneously attaining good exposure during surgery, In situations with inadequate exposure, several surgical techniques such as V-Y quadricepsplasty, quadriceps snip, and tibial tubercle osteotomy have been reported in the literature, with good resultant functional outcomes [6,7,8,9]. Quadriceps rupture can still occur despite maintaining all surgical precautions, either atraumatically or following a direct traumatic injury. Implant loosening and periprosthetic fractures could also accompany soft-tissue injuries, especially in morbidly obese patients.
A 71-year-old female patient with a body mass index of 49.5 kg/m2 underwent a TKA of her left knee in view of tricompartmental osteoarthritis. The patient had not undergone any intervention in the left knee previously. The intraoperative, perioperative, and immediate post-operative period was uneventful up to the 17th day post-surgery. The patient gave a history of a sudden popping sensation on the 17th post-operative day while walking at her house. It was immediately followed by pain and inability to bear weight on the left leg, leading to a fall on the ground. She was unable to perform straight leg raising as well as active quadriceps contraction while retaining other ranges of movement. On clinical examination, weak flickering of the quadriceps was seen. Subsequently, she was advised ultrasound and then magnetic resonance imaging (MRI) to assess the status of the quadriceps tendon.
On ultrasound evaluation, the quadriceps tendon was found to be completely torn, coiled, and retracted 5 cm proximally, up to the middle of the thigh. The diagnosis of the ruptured quadriceps was confirmed on the MRI. The patient was then planned for a re-exploration and primary repair surgery of the quadriceps tendon by reattachment to the superior pole of the patella using 2 corkscrew double-loaded suture anchors.
In supine position, an incision was taken over the previous scar. Patellar attachment of quadriceps tendon was found to be lost. Thin, frayed, and torn ends of quadriceps were seen, retracted up to 5 cm proximally.
Step 1: The quadriceps tendon was isolated with the proximal stump visualized to be frayed and of poor quality. Edges of the proximal stump were freshened and the reducibility was checked on the patella in extension and 40° knee flexion (Fig. 1).
Step 2: Two, 5.0 mm corkscrew, double-loaded suture anchors were inserted in the superior pole of the patella keeping the anchors engaged in such a position that it does not hamper the positioning of the replaced patella.
Step 3: From each anchor, two sutures were suspended. From each anchor, one suture was passed through the medial and lateral retinacula. Two remaining sutures, one from each anchor, are then passed through the proximal quadriceps stump.
Step 4: The sutures were passed in the central substance of the quadriceps tendon with the Krackow locking technique. These sutures were then tied on the distal remnant over the patella in 40° of knee flexion.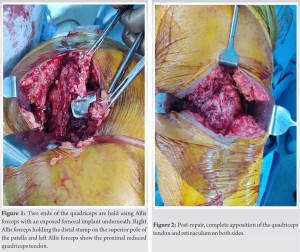
Step 5: After fixation of the proximal stump on the distal, the retinaculum was tied to close the joint. Two free suture tapes were then passed from the medial patellofemoral retinaculum to the quadriceps tendon to the lateral patellofemoral retinaculum and tied to reinforce the fixation (Fig. 2).
The skin was, then, closed in layers using retention stitches [10] and the patient was advised to wear a long knee brace for 4 weeks postoperatively. Thereafter, graduated knee bending was started passively from 4th week post-repair, active from 6th week post-repair, and progressed to active knee bending from 7th week in supine and while sitting at the edge of the bed. At 8 weeks postoperatively, the patient developed 50° active knee bending and 90° knee bending while doing the edge of the bed sitting, and full extension with straight leg raising (Fig. 3, 4, 5).

The patient was advised to continue walking with a long knee brace until the strength of the quadriceps was regained. Progressive knee bending was encouraged with the target flexion in the supine position set at around 90–100° (functional range of motion). The MRI scan taken 3.5 months after the repair was suggestive of low signal intensity in the middle one third of the transverse dimension with good healing in the medial and lateral one-third of the transverse diameter. The patient was able to walk without a brace or any additional support device at 10 weeks post-surgery. At 6 months postoperatively, the patient recovered substantially, regaining 90° knee flexion in the supine position and 110° knee flexion while sitting on the edge of the bed. She had a Tegner Lysholm score of 88 (/100), falling into the good category of the Tegner Lysholm grading [11].
Extensor mechanism injury post-TKA can be a challenge for the surgeon as it is commonly associated with poor long-term outcomes. It can result from various causes ranging from iatrogenic to traumatic disruption. This dysfunction may be acute, subacute, or chronic and can involve any of the anatomical components of the extensor mechanism. Adequate repair or reconstruction is considered paramount for achieving good functional outcome and helping the patient return to daily activities [12].
Obesity has been known to compromise not just the bone quality, but also the requisite tendon strength in such patients, making a surgery like TKA tricky in the intraoperative as well as post-operative rehabilitation period, as documented by Abate [13]. Another stumbling block in such patients is the ease of diagnosis of quadriceps injury if and when it manifests, thereby warranting high degree of suspicion. Difficulty in identifying the defect on palpation in these patients is a potential problem as was encountered in this case. In addition, post-operative quadriceps weakness can potentially mask the diagnosis of quadriceps rupture. In this case too, the diagnosis was made early due to the acumen of the surgeon in identifying the injury based on flickering contractions in the quadriceps on trying to extend the knee, and the inability to do straight leg raises. Based on our observation, when such a complication is suspected, especially in a background of trauma, we recommend ultrasound scanning as a primary modality for definitive diagnosis in all patients with post-operative extensor weakness. This can prevent a delay in the diagnosis and repair of the quadriceps tendon, and resultantly a long-term morbidity [14].
The previously reported cases of this complication have shown satisfactory results by repair in the early stages of rupture and reconstruction in the late stages as stated in the extensive systemic review done by Vajapey et al. [15]. However, treatment modality used in morbidly obese patients has barely been reported. We successfully managed our case using two suture anchors and fortification of the repair using two suture tapes as aforementioned. Despite the MRI at 3.5 months post-repair showing a low signal in the central third substance, the patient regained functional ranges and power by 6 months, presumably due to the integrity of the lateral and medial fixation, and the subsequent fibrotic healing of the central substance. The guarded physiotherapy protocol in the aftermath of the repair further helped in a more pragmatic rehabilitation. With a dearth in literature regarding the management of such complications and an increasing rate of TKAs being done in high body mass index patients, a high degree of suspicion combined with the surgical technique and physiotherapy protocol highlighted in this case report can be of great help to the patient and surgeons alike.
Quadriceps rupture is a rare but potentially debilitating complication after a TKA surgery. Morbidly obese patients are at a higher risk to this owing to their inherently weak extensor apparatus and the higher propensity to a traumatic injury. In case of a tear in such cases, prompt clinical and ultrasound assistance diagnosis is a must. Subsequent repair with anchor sutures and further fortification of the retinaculum and the repair provides excellent results. A guarded rehabilitation protocol after the TKA can help prevent the complication, as well as help with a satisfactory recovery in case of a repair.
Management of acute quadriceps rupture post-TKA starts with its early diagnosis by maintaining a high degree of suspicion and taking radiological assistance for its confirmation. Repair of such tears using anchor sutures in morbidly obese patients, coupled with guarded physiotherapy regimen, gives excellent functional results in the short and long term.
References
- 1.Callahan CM, Drake BG, Heck DA, Dittus RS. Patient outcomes following tricompartmental total knee replacement. A meta-analysis. JAMA 1994;271:1349-57. [Google Scholar | PubMed]
- 2.Skou ST, Roos EM, Laursen MB, Rathleff MS, Arendt-Nielsen L, Simonsen O, et al. A randomized, controlled trial of total knee replacement. N Engl J Med 2015;373:1597-606. [Google Scholar | PubMed]
- 3.Gustillo R, Thompson R. Quadriceps and patellar tendon ruptures following total knee arthroplasty. In: Rand JA, Dorr LD, editors. Total Arthroplasty of the Knee: Proceedings of the Knee Society, 1985-1986. Rockville: Aspen; 1987. p. 41-7. [Google Scholar | PubMed]
- 4.Lynch AF, Rorabeck CH, Bourne RB. Extensor mechanism complications following total knee arthroplasty. J Arthroplasty 1987;2:135-40. [Google Scholar | PubMed]
- 5.Yun AG, Rubash HE, Scott RD, Laskin RS. Quadriceps rupture associated with a proximal quadriceps release in total knee arthroplasty. A report of three cases. J Bone Joint Surg Am 2003;85-A:1809-11. [Google Scholar | PubMed]
- 6.Garvin KL, Scuderi G, Insall JN. Evolution of the quadriceps snip. Clin Orthop Relat Res 1995;321:131-7. [Google Scholar | PubMed]
- 7.Scott RD, Siliski JM. The use of a modified V-Y quadricepsplasty during total knee replacement to gain exposure and improve flexion in the ankylosed knee. Orthopedics 1985;8:45-8. [Google Scholar | PubMed]
- 8.Whiteside LA. Exposure in difficult total knee arthroplasty using tibial tubercle osteotomy. Clin Orthop Relat Res 1995;321:32-5. [Google Scholar | PubMed]
- 9.Trousdale RT, Hanssen AD, Rand JA, Cahalan TD. V-Y quadricepsplasty in total knee arthroplasty. Clin Orthop Relat Res 1993;286:48-55. [Google Scholar | PubMed]
- 10.Rajani AM, Thakkar CJ, Shah UA, Punamiya M. Retention stitches: A concept of wound closure of knee arthroplasty in obese patients. Indian J Orthop 2022;56:1048-52. [Google Scholar | PubMed]
- 11.Mitsou A, Vallianatos P, Piskopakis N, Maheras S. Anterior cruciate ligament reconstruction by over-the-top repair combined with popliteus tendon plasty. J Bone Joint Surg Br 1990;72:398-404. [Google Scholar | PubMed]
- 12.Vyas P, Cui Q. Management options for extensor mechanism discontinuity in patients with total knee arthroplasty. Cureus 2020;12:e9225. [Google Scholar | PubMed]
- 13.Abate M. How obesity modifies tendons (implications for athletic activities). Muscles Ligaments Tendons J 2014;4:298-302. [Google Scholar | PubMed]
- 14.Soong J, Silva A, Andrew TH. Disruption of quadriceps tendon after total knee arthroplasty: Case report of four cases. J Orthop Surg (Hong Kong) 2017;25:2309499017717206. [Google Scholar | PubMed]
- 15.Vajapey SP, Blackwell RE, Maki AJ, Miller TL. Treatment of extensor tendon disruption after total knee arthroplasty: A systematic review. J Arthroplasty 2019;34:1279-86. [Google Scholar | PubMed]









