In the presence of sickle cell anemia, COVID-19 infection may trigger avascular necrosis of the femoral head independently of steroid use.
Dr. Selim Ergün, Department of Orthopaedic Surgery, Kartal Dr. Lutfi Kirdar City Hospital, D-100 Guney Yanyol No:47 Cevizli Mevkii, Kartal, Istanbul - 34865, Turkey. E-mail: drselimergun@gmail.com
Introduction: The COVID-19 pandemic has affected many people around the world with its primary and secondary consequences. The use of high-dose steroids in its treatment brought along steroid-related femoral head avascular necrosis (AVN) complication.
Case Presentation: We present a case of bilaterally developed femoral head AVN following COVID-19 infection in a patient with sickle cell disease (SCD), without the history of steroid use.
Conclusion: With this case report, we aimed to raise awareness that COVID-19 infection may trigger AVN of the hip joint in SCD patients.
Keywords: COVID-19, avascular necrosis, femoral head, sickle cell disease.
The COVID-19 (SARS CoV-2) pandemic continues to be effective all over the world, causing vital morbidity and severe morbidity. The clinical features of COVID-19 infection vary from mild to critical symptoms. It is known that those critical symptoms are more commonly seen in adults with advanced age and those with underlying comorbidities [1] Sickle cell disease (SCD) is an important one of these comorbidities. During the COVID-19 pandemic, an increased number of acute chest syndrome and vasoocclusive attacks have been reported in infected SCD patients [2,3,4]. As well as the acute chest syndrome and vasoocclusive attacks, osteonecrosis is also a severe complication of SCD, and its prevalence has varied from 2% to 17% [5]. As it is known that COVID-19 infection increases the number of vasoocclusive attacks in these patients, it may also increase the risk of developing acute osteonecrosis in these patients [3]. We report on the first documented case of a patient with SCD who developed acute hip pain that started with COVID-19 infection, and was diagnosed with bilateral avascular necrosis (AVN) of the femoral heads. The aim of this case report was to raise awareness in SCD patients that COVID-19 infection may trigger AVN of the hip joint.
A 51-year-old female patient with a known SCD, on maintenance deferasirox and hydroxyurea therapy, presented to our outpatient service with the complaint of bilateral hip pain. Patient’s surgical history contained splenectomy and cholecystectomy. There was no prior use of steroid for any medical condition in patient’s medical history according to national health insurance system database. In the emergency room, where she admitted with cough and fever, COVID-19 swab test had been performed and PCR results came positive for COVID-19 2 months before her first orthopedic consultation. She was hospitalized with the diagnosis of pneumonia for 7 days. Although there was no lung involvement in her chest computer tomography images, D-Dimer, and C-reactive protein levels were high in laboratory tests, 690 ng/L and 12,8 mg/L, respectively. Low molecular weight heparin, Proton Pump Inhibitor, and Favipiravir medications were added to her treatment.
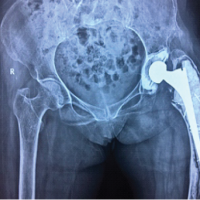
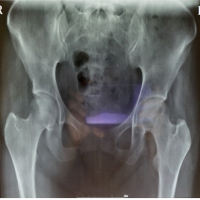
After discharge, she complained of bilateral hip pain. She admitted to orthopedic outpatient clinic 2 months after the first sign of COVID-19 infection. On physical examination, she could not bear her weight on her right lower extremity and had difficulty even walking. Plain radiographs (Fig. 1) and magnetic resonance imaging (Fig. 2) revealed bilateral Stage I AVN of the femoral heads according to the Modified Ficat classification [6]. Core decompression was been planned and performed on the right hip with guidance C-Arm. 4,5 mm drill was used to decompress the femoral head in two different locations. Weight bearing was not allowed for the post-operative first 6 week, immediate physical therapy was for range of motion. Follow-up examination at 10 weeks showed that she had less pain, pre-operative VAS score improved from 8 to 3, and was able to walk without crutches. At the end of the 1st post-operative year, VAS score improved to 2, and WOMAC hip score for functional status improved from 14.8 to 54.7. No femoral head subchondral bone collapse was observed in the anteroposterior radiograph of the pelvis for radiological (Fig. 3). This case report was conducted in accordance with the Helsinki Declaration of Principles and informed consent has been obtained from the patient.
SCD is one of the important risk factors to develop AVN of the femoral head, even though trauma and steroid use are the leading causes. In the current literature, there are reports that aimed to raise awareness about the fact that high-dose steroid use appears to increase the prevalence of osteonecrosis [7,8]. Regardless of steroid use, this case report indicates that COVID-19 infection may trigger femoral head AVN in individuals with thrombosis-prone hereditary diseases such as SCD.
SCD patients are known to be prone to vasoocclusive attacks and thromboembolic complications [9]. Although the impact of COVID-19 on morbidity and mortality associated with SCD is not clear yet, the question of whether the COVID-19 infection increased these vasoocclusive attacks was one of the curiosities of the pandemic process. To clarify this unknown, Alkindi et al. aimed to assess the impact of COVID-19 on the morbidity and mortality of vasoocclusive attacks in SCD patients. They found that COVID-19 infection increased the number of vasoocclusive attacks in SCD patients; however, it did not significantly influence vasoocclusive attack related morbidity or mortality in their SCD cohort [3].
There was no case report to the best of our knowledge that COVID-19 infection caused or triggered AVN of the hip joint. Our patient’s history of SCD would have facilitated femoral head osteonecrosis because sickle cell anemia is one of the known causes of femoral head AVN [10]. However, there was no history of hip pain or steroid use before and after our patient suffered from COVID-19 infection according to national health insurance system database. Although this coincidence might be incidental, COVID-19 infection might have triggered AVN of the femoral head in this SCD patient.
We treated our patient surgically by core decompression. Surgical management of AVN of the hip is still controversial but highlighted by Mukisi-Mukaza et al. that core decompression has good results in short-term period [11]. Similarly, we had good result in our patient but we do not know the consequences of the core decompression in the long-term.
In patients with SCD, COVID-19 infection may trigger bone osteonecrosis more easily compared to healthy individuals and may trigger AVN of the hip independent of steroid use in the treatment.
While the pandemic has not yet ended, it should be kept in mind that femoral head AVN may develop in patients with COVID-19 infection and presenting with hip pain. Regardless of the use of steroids in the treatment, thrombosis-prone diseases such as SCD should be questioned in these patients.
References
- 1.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China. JAMA 2020;323:1239-42. [Google Scholar | PubMed]
- 2.Beerkens F, John M, Puliafito B, Corbett V, Edwards C, Tremblay D. COVID-19 pneumonia as a cause of acute chest syndrome in an adult sickle cell patient. Am J Hematol 2020;95:E154-6. [Google Scholar | PubMed]
- 3.Alkindi S, Elsadek RA, Al-Madhani A, Al-Musalhi M, AlKindi SY, Al-Khadour G, et al. Impact of COVID-19 on vasooclusive crisis in patients with sickle cell anaemia. Int J Infect Dis 2021;106:128-33. [Google Scholar | PubMed]
- 4.Hussain FA, Njoku FU, Saraf SL, Molokie RE, Gordeuk VR, Han J. COVID-19 infection in patients with sickle cell disease. Br J Haematol 2020;189:851-2. [Google Scholar | PubMed]
- 5.Daltro G, Franco BA, Faleiro TB, Rosário DA, Daltro PB, Fortuna V. Osteonecrosis in sickle cell disease patients from Bahia, Brazil: A cross-sectional study. Int Orthop 2018;42:1527-34. [Google Scholar | PubMed]
- 6.Jawad MU, Haleem AA, Scully SP. In brief: Ficat classification: Avascular necrosis of the femoral head. Clin Orthop Relat Res 2012;470:2636-9. [Google Scholar | PubMed]
- 7.Zhang B, Zhang S. Corticosteroid-ınduced osteonecrosis in COVID-19: A call for caution. J Bone Miner Res 2020;35:1828-9. [Google Scholar | PubMed]
- 8.Zhang S, Wang C, Shi L, Xue Q. Beware of steroid-ınduced avascular necrosis of the femoral head in the treatment of COVID-19-experience and lessons from the SARS epidemic. Drug Des Devel Ther 2021;4:983-95. [Google Scholar | PubMed]
- 9.Steinberg MH. Management of sickle cell disease. N Engl J Med 1999;340:1021-30. [Google Scholar | PubMed]
- 10.Barney J, Piuzzi NS, Akhondi H. In: Hughes E, Rubio G, editors. Femoral Head Avascular Necrosis. Treasure Island, FL: StatPearls; 2021. p. 1-22. [Google Scholar | PubMed]
- 11.Mukisi-Mukaza M, Manicom O, Alexis C, Bashoun K, Donkerwolcke M, Burny F. Treatment of sickle cell disease’s hip necrosis by core decompression: A prospective case-control study. Orthop Traumatol Surg Res 2009;95:498-504. [Google Scholar | PubMed]