Ochronotic hip arthropathy – A case report.
Dr. Nirvin Paul, Department of Trauma Surgery, All India Institute of Medical Science, Rishikesh, Uttarakhand, India. E-mail: drnirvinpaul@gmail.com
Introduction: Ochronotic arthropathy is a rapidly progressive sequelae of alkaptonuria. This is a rare autosomal recessive condition caused by a mutation in the homogentisate 1,2 dioxygenase (HGD) gene leading to HGD enzyme deficiency. Here, we report a case of neck femur fracture in a patient with ochronotic arthropathy managed by primary hip arthroplasty.
Case Report: A 62-year-old gentleman presented with complaints of pain in his left groin area and difficulty in weight bearing on his left lower limb for 3 weeks. The pain was sudden in onset and started while he was on his morning walk. He did not have any problems with his left hip before this episode and he did not give a history of any significant trauma. History, radiological, and intraoperative findings revealed ochronotic hip arthropathy.
Conclusion: Ochronotic arthropathy is relatively rare and is seen in isolated communities. The treatment options are similar to primary osteoarthritis and the outcome is comparable to arthroplasty done for osteoarthritis.
Keywords: Ochronotic arthropathy, alkaptonuria, ochronosis, blackening of urine
Ochronotic arthropathy is a rapidly progressive sequelae of alkaptonuria. This is a rare autosomal recessive condition caused by a mutation in the homogentisate 1,2 dioxygenase (HGD) gene leading to HGD enzyme deficiency [1], which has a role in phenylalanine and tyrosine amino acid metabolism [1]. The classically described clinical trial of the disease includes (1) excretion of excess homogentisic acid (HGA) in urine, which causes the urine to turn dark on standing, due to oxidation (Alkaptonuria), (2) progressive deposition of HGA products as a polymer or quinone intermediary (ochronotic pigment) in tissues leading to dark pigmentation (Ochronosis), and (3) rapidly progressive arthropathy due to joint cartilage’s brittleness caused by the accumulation of HGA products (Ochronotic arthropathy) [2].
A 62-year-old gentleman presented with complaints of pain in his left groin area and difficulty in weight bearing on his left lower limb for 3 weeks. The pain was sudden in onset and started while he was on his morning walk. He did not have any problems with his left hip before this episode and he did not give a history of any significant trauma. At the time of presentation to the clinic, he was able to take a few steps – but with extreme pain. Examination revealed a shortened, externally rotated left lower limb with restriction of movements of his left hip due to severe pain. The patient also complained of back pain and bilateral knee pain for the past 10 years while walking – but this did not limit his activities significantly. On enquiry about his personal habits, he mentioned that he had a past history of “blackening of urine” since childhood but had not had any treatment for the same. X-rays revealed a subcapital fracture of the left neck of the femur with partial destruction of the femoral head (Fig. 1).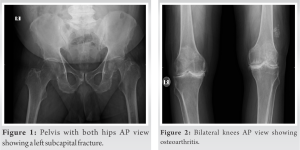 Bilateral knee radiographs confirmed the clinical diagnosis of chronic arthritis (Fig. 2). X-ray of the lumbosacral spine showed gross calcification in the disc, vacuum phenomenon, and loss of height of the intervertebral discs accompanied by fusion (pseudo-block) vertebrae formation (Figs. 3 and 4). Following routine evaluation, he underwent an uncemented total hip arthroplasty of his left hip under general anesthesia.
Bilateral knee radiographs confirmed the clinical diagnosis of chronic arthritis (Fig. 2). X-ray of the lumbosacral spine showed gross calcification in the disc, vacuum phenomenon, and loss of height of the intervertebral discs accompanied by fusion (pseudo-block) vertebrae formation (Figs. 3 and 4). Following routine evaluation, he underwent an uncemented total hip arthroplasty of his left hip under general anesthesia. No special precautions were taken for the surgery. The hip joint was found to have black pigmentation of the femur head which was partially destroyed, along with degenerated pigmented articular cartilage (Figs. 5 and 6). The acetabulum was also black, but the underlying bone quality was good.
No special precautions were taken for the surgery. The hip joint was found to have black pigmentation of the femur head which was partially destroyed, along with degenerated pigmented articular cartilage (Figs. 5 and 6). The acetabulum was also black, but the underlying bone quality was good.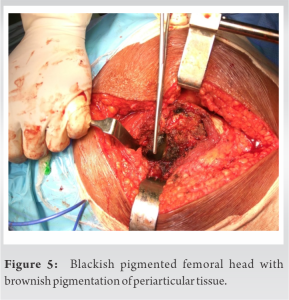 An uncemented hip was implanted (Depuy-Corrail Pinnacle, with a ceramic head and ALTRX polyethylene liner). Screws were added for additional stability of the cup (Fig. 7).
An uncemented hip was implanted (Depuy-Corrail Pinnacle, with a ceramic head and ALTRX polyethylene liner). Screws were added for additional stability of the cup (Fig. 7). 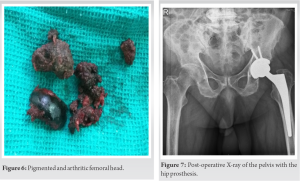 The surgical time was 45 min and blood loss was only 250 ml. There were no pre-operative complications. Post-operative drain output was minimal and the drain was removed at 48-h post-operative. The patient was ambulated on the 2nd post-operative day and was discharged without any complications.
The surgical time was 45 min and blood loss was only 250 ml. There were no pre-operative complications. Post-operative drain output was minimal and the drain was removed at 48-h post-operative. The patient was ambulated on the 2nd post-operative day and was discharged without any complications.
The first recorded case of the disease dates back to 1500 BC in an Egyptian mummy. Core biopsies of the hip revealed that the mummy had ochronosis [3]. Boedeker first coined the term Alkaptonuria in 1859, after he discovered unusual reducing properties in the urine of a patient (Laboratory proof of alkaptonuria is based on reducing properties of HGA when mixed with Fehling’s solution to turn a characteristic black and brown color). Ochronosis was first named and described by Virchow in 1866 when he noted the HGA pigment in the costochondral cartilage that appeared ochre (yellow/brown) in colorunder the microscope [4]. The worldwide prevalence of alkaptonuria is one in 250 000–1 000 000 births [5]. It is reported to be more prevalent in Slovakia, the Dominican Republic, India, and Jordan. The highest prevalence is in Slovakia where up to one in 19,000 are affected [6]. The reported cases are usually found in hamlets or more isolated communities which may suggest the role of genetic isolation or rather lack of genetic variability in the propagation of the disease. Ochronotic arthropathy results from the deposition of the HGA polymer within hyaline articular cartilage. Pigmentation is widespread, with all tissues of the joint organ being affected. The affected tissues often become weak, brittle, and prone to chipping, fracturing, and cracking, causing rapid joint degeneration, which leaves the patient profoundly disabled at a young age. The disease does not affect the longevity of the patient but can have a severe negative impact on the quality of life [7]. Typically, the pigment is seen clearly in the eyes and ears of patients but is also present in bodily fluids, including perspiration, which often results in skin discoloration. Organs affected include the large joints of the body, cardiovascular system, kidney, skin, and glands. Other manifestations include renal, prostate, gall bladder, and salivary gland stones, ruptures of tendons and ligaments, osteopenia, and fractures. Patients with ochronotic arthropathy usually present with lumbar back pain. Larger weight-bearing joints tend to be affected later in life. The most commonly affected joints are the knees (64%), shoulders (43%), and hips (35%) [8]. In the early stages, ochronotic arthropathy may often be misdiagnosed as osteoarthritis or ankylosing spondylitis. Usually, the involvement of these joints is severe and often requires joint replacement [5,9]. The literature on surgical management of ochronotic arthropathy is limited to a few case studies without long-term follow-up and furthermore, there is no mention of complications. Spencer et al. [9] reported in their case series of three patients who underwent 11 arthroplasties in both upper and lower limbs that the implant survival rates are comparable to that of arthroplasties carried out for osteoarthritis. Abimbola reported a similar finding in a single case of knee replacement [10], as did Ozmanevra et al. who reported on a single case of bilateral knee replacement [11]. There is no effective medical management for alkaptonuria. Dietary restriction of tyrosine and phenylalanine will reduce the excretion of HGA, although the clinical effect is limited. The arthropathy is mostly not reversible, although it is possible that diet may prevent further progression. Ascorbic acid, which inhibits the enzyme that catalyzes the oxidation of HGA to the polymer with an affinity for collagen, is given by some clinicians, but its efficacy has not been demonstrated for ochronosis. Nitisinone, which inhibits the second enzyme in the tyrosine catabolic pathway, decreased urinary HGA levels by 95% in one short-term study [12]. However, no clinical benefits (range of motion and other measures of musculoskeletal function) were demonstrated in a randomized trial in patients who already had arthritis [13]. It is unknown whether early treatment before the development of musculoskeletal symptoms would be beneficial.
Management of ochronotic arthropathy is usually symptomatic, with anti-inflammatory drugs and pain killers for the early stages of the disease, with appropriate bracing. As in osteoarthritis, arthroplasty surgery in advanced disease can be offered when indicated. There is not enough literature to comment on long-term survival, but case reports suggest that survival is like in other arthritic conditions.
Ochronotic arthropathy is relatively rare and primary arthroplasty can be performed when indicated. The outcome is similar to arthroplasty done for osteoarthritis based on available literature.
References
- 1.Zatková A, de Bernabé DB, Poláková H, Zvarík M, Feráková E, Bosák V, et al. High frequency of alkaptonuria in Slovakia: Evidence for the appearance of multiple mutations in HGO involving different mutational hot spots. Am J Hum Genet 2000;67:1333-9. [Google Scholar | PubMed]
- 2.Doganavsargil B, Pehlivanoglu B, Bicer EK, Argin M, Bingul KB, Sezak M, et al. Black joint and synovia: Histopathological evaluation of degenerative joint disease due to Ochronosis. Pathol Res Pract 2015;211:470-7. [Google Scholar | PubMed]
- 3.Stenn FF, Milgram JW, Lee SL, Weigand RJ, Veis A. Biochemical identification of homogentisic acid pigment in an ochronotic Egyptian mummy. Science 1977;197:566-8. [Google Scholar | PubMed]
- 4.Bhattar PA, Zawar VP, Godse KV, Patil SP, Nadkarni NJ, Gautam MM. Exogenous ochronosis. Indian J Dermatol 2015;60:537-43 [Google Scholar | PubMed]
- 5.Phornphutkul C, Introne WJ, Perry MB, Bernardini I, Murphey MD, Fitzpatrick DL, et al. Natural history of alkaptonuria. N Engl J Med 2002;347:2111-21. [Google Scholar | PubMed]
- 6.Ranganath L, Taylor AM, Shenkin A, Fraser WD, Jarvis J, Gallagher JA, et al. Identification of alkaptonuria in the general population: A United Kingdom experience describing the challenges, possible solutions and persistent barriers. J Inherit Metab Dis 2011;34:723-30. [Google Scholar | PubMed]
- 7.Fisher AA, Davis MW. Alkaptonuric ochronosis with aortic valve and joint replacements and femoral fracture: A case report and literature review. Clin Med Res 2004;2:209-15. [Google Scholar | PubMed]
- 8.Takagi M, Ida H, Kobayashi S, Ishii M, Osanai T, Konttinen YT. Ochronotic spondylarthropathy: Two case reports of progressive destructive changes in the hip. Mod Rheumatol 2003;13:81-6. [Google Scholar | PubMed]
- 9.Spencer J, Gibbons CL, Sharp R, Carr A, Spencer J, Gibbons CL, et al. Arthroplasty for ochronotic arthritisNo failure of 11 replacements in 3 patients followed 6-12 years Arthroplasty for ochronotic arthritis No failure of 11 replacements in 3 patients followed 6-12 years. 2009;6470. [Google Scholar | PubMed]
- 10.Abimbola O, Hall G, Zuckerman JD. Degenerative arthritis of the knee secondary to ochronosis. Bull NYU Hosp Jt Dis 2011;69:331-4. [Google Scholar | PubMed]
- 11.Ozmanevra R, Güran O, Karatosun V, Günal I. Total knee arthroplasty in ochronosis: A case report and critical review of the literature. Eklem Hastalik Cerrahisi 2013;24:169-72. [Google Scholar | PubMed]
- 12.Suwannarat P, O’Brien K, Perry MB, Sebring N, Bernardini I, Kaiser-Kupfer MI, et al. Use of nitisinone in patients with alkaptonuria. Metabolism 2005;54:719-28. [Google Scholar | PubMed]
- 13.Introne WJ, Perry MB, Troendle J, Tsilou E, Kayser MA, Suwannarat P, et al. A 3-year randomized therapeutic trial of nitisinone in alkaptonuria. Mol Genet Metab 2011;103:307-14. [Google Scholar | PubMed]









