This article describes a 6-pin technique in the management of proximal humerus fracture with a JESS fixator and its outcome at a 1-year follow-up.
Dr. Baskar Chockalingam, Parvathy Nursing Home, Tirunelveli, Tamil Nadu, India. E-mail: orthobaskey@gmail.com
Introduction: Proximal humerus fractures account for 4–5% of the fractures in long bones with a bimodal distribution. A wide spectrum of options are available in its management ranging from conservative to total shoulder replacement. We aim to demonstrate a minimally invasive simple 6-pin technique in the management of proximal humerus fracture using Joshi external stabilization system (JESS).
Case Report: We report the results of ten patients (M: F = 4:6) with proximal humerus fractures of age range between 19 and 88 years managed with the 6-pin technique JESS under regional anesthesia. Of the included patients, 4, 3, and 3 cases belonged to Neer Type II, III, and IV, respectively. On analysis of outcomes based on the Constant-Murley score, we noted excellent outcomes and good outcomes in 6 (60%), and 4 (40%) patients, respectively, at 12 months. Fixator was removed after the radiological union between 8 and 12 weeks. Complications noted include pin tract infection in 1 (10%) and malunion in 1 (10%) case.
Conclusion: JESS fixation by 6-pin technique remains a viable minimally invasive cost-effective treatment option in the management of proximal humerus fractures.
Keywords: JESS, proximal humerus fractures, 6-pin technique, minimally invasive, case series.
Proximal humerus fractures account for 4–5% of the fractures [1] and are the third most common fracture of insufficiency following the hip and distal radius fracture [2]. Although bimodal distribution is noted, it is more common in older osteoporotic individuals following trivial falls [3,4]. Although minimally displaced fractures can be managed by non-operative measures, displaced comminuted fractures necessitate surgical management for optimal outcomes [5]. The fractures that mandate surgical management is compounded with vascular compromise from injury to the circumflex humeral artery from the trauma resulting in avascular necrosis of the humeral head in 12–34% of three-part and 41–59% of four-part proximal humerus fractures [6,7]. Hence, an ideal management strategy in such fractures needs to be minimally invasive and promote earlier mobilization to obtain optimal outcomes. Conservative management mandates prolonged shoulder immobilization [8], while open surgical management with plating would involve excessive soft-tissue dissection which further increases the risk of avascular necrosis [9,10] Hence, we aim to demonstrate a minimally invasive simple 6-pin technique in the management of proximal humerus fracture using Joshi external stabilization system (JESS).
We report the results of ten patients (M: F = 4:6) with proximal humerus fractures of age range between 19 and 88 years managed prospectively with 6-pin technique JESS under regional anesthesia. We included adult patients presenting with acute displaced proximal humerus fracture and excluded undisplaced or pathological or compound fractures of the proximal humerus. Of the included patients, 4, 3, and 3 cases belonged to Neer Type II, III, and IV, respectively. Following the initial radiological examination with the anteroposterior and axillary views, computed tomography was taken when necessary to understand the fracture geometry.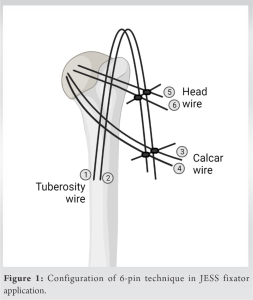
6-pin technique JESS
The patient is positioned supine with sandbag under the affected shoulder. The standard 6-pin technique JESS fixation starts by bringing the head into position by the joystick method using thick K-wires and temporary fixation with the glenoid in unstable situations. The first 2-pins are the tuberosity wires introduced from greater tuberosity to the medullary cavity to align the neck with the distal shaft. The next 2-pins are the calcar wires introduced to stabilize the head fragment with the shaft of the humerus. The two sets of pins are connected by bending the core wires and locked to the calcar wires by disimpacting the head in valgus. This forms a tension system to keep the stabilized fragments in place, as shown in Fig. 1. The final 2-pins are the neck wires that stabilize the head to the shaft of the humerus. Necessary modifications can be done as per the fracture geometry and bone quality to add additional stability to the assembly. The final stability is assessed under fluoroscopy and pin tract dressing is applied and an arm sling is applied. We used 2.5 mm pins in this technique. Simple sling was continued for 3 weeks with pin tract dressing done every 3 days. Mobilization was started on the 2nd post-operative day with flexion, extension, and pendulum exercises. Isometric exercises along with abduction exercises were started cautiously from 3rd week. The serial assessment was made at 6 weeks, 3 months, 6 months, and 1 year using radiographs and functional outcome with Constant-Murley scoring (excellent>85; good 71–85; fair 50–70; and poor <50) [11]. On analysis of outcomes based on the Constant-Murley score, we noted excellent and good outcomes in six patients (60%), and four patients (40%), respectively, at 12 months. We did not note any poor outcomes. The improvement in the outcome scores at individual follow-up time points is given in Table 1. Fixator was removed after the radiological union between 8 and 12 weeks. Complications noted include pin tract infection in 1 (10%), pin loosening in 1 (10%), and malunion in 1 (10%) case. None of the cases went to non-union. An illustrative case example of a 3-part proximal humerus in a 65-year-old male is presented in Fig. 2.
The currently available management methods for displaced proximal humerus fracture range from non-operative treatment to total shoulder replacement [4,12]. There is an ongoing debate on the best available treatment method in its management [12,13]. Although undisplaced fractures are more commonly managed non-operatively, displaced fractures necessitate surgical management for restoring the anatomic configuration to the proximal humerus [14]. The Neer’s classification [15] considers the four key anatomic regions such as the anatomic neck, surgical neck, greater tuberosity, and lesser tuberosity, and their displacement of more than 1 cm or 45° angulation to classify these fractures [16]. Conservative management in displaced fractures reports complications such as non-union, stiffness, malunion, avascular necrosis of the humeral head, and impingement syndromes [1,8]. To preserve the residual vascularity of the proximal humerus, minimally invasive fixation systems were on the rise in the management of proximal humerus fractures. Hoffman fixator system was introduced on that ideology, but the Steinman pins used were bulky which also increases the soft-tissue injury and limits the available space for the application of multiple pins [17]. Moreover, they reported a high risk of pin tract infections and loosening [6]. JESS developed by Joshi [18] in 1987 is a minimally invasive system using k-wires of 2–2.5 mm in diameter that provides stable fixation of the reduction achieved intraoperatively in the management of proximal humerus fractures based on the ligamentotaxis principle [19]. The minimal dimensions of the wires used make them amenable to usage in various planes without the risk of soft tissue or neurovascular injury when applied appropriately. The 6-pin technique described is a simple technique taking into consideration of the key fracture fragments that need stabilization to achieve a tensile construct that maintains the reduction achieved intraoperatively. The soft-tissue dissection is further reduced thereby increasing the chances of union and preserving the vascularity. Moreover, the current system facilitates early rehabilitation due to the uninjured rotator cuff following closed reduction and JESS fixation. Our study validated the use of the JESS system in the displaced proximal humerus fractures using a minimal 6-pin technique demonstrating excellent to good outcomes in all the included patients. The advantages of the proposed technique of fixation include maintaining an intact fracture hematoma facilitating fracture union, stable osteosynthesis without immobilizing the adjacent joint, minimal invasiveness, and less implant footprint. Moreover, if necessary adjustment of the construct is possible at later date without anesthesia. Similarly, implant removal can also be done without anesthesia. It can be implemented even in a low-resource setting without compromising the outcomes. Although there is a risk of pin-tract infection, it can be effectively prevented by regular pin-site dressing and managed with antibiotic therapy. The reported outcomes were comparable to the previous reports on the fixation system for proximal humerus fractures [19,20,21].
JESS fixation by 6-pin technique remains a viable minimally invasive cost-effective treatment option in the management of proximal humerus fractures.
The 6-pin technique of the JESS fixator application is a simple, cost-effective, and minimally invasive treatment option in the management of proximal humerus fractures.
References
- 1.Handoll HH, Gibson JN, Madhok R. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev 2003;4:CD000434. [Google Scholar | PubMed]
- 2.Court-Brown CM, Garg A, McQueen MM. The epidemiology of proximal humeral fractures. Acta Orthop Scand 2001;72:365-71. [Google Scholar | PubMed]
- 3.Chu SP, Kelsey JL, Keegan TH, Sternfeld B, Prill M, Quesenberry CP, et al. Risk factors for proximal humerus fracture. Am J Epidemiol 2004;160:360-7. [Google Scholar | PubMed]
- 4.Bell JE, Leung BC, Spratt KF, Koval KJ, Weinstein JD, Goodman DC, et al. Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. J Bone Joint Surg Am 2011;93:121-31. [Google Scholar | PubMed]
- 5.Helmy N, Hintermann B. New trends in the treatment of proximal humerus fractures. Clin Orthop Relat Res 2006;442:100-8. [Google Scholar | PubMed]
- 6.Hintermann B, Trouillier HH, Schäfer D. Rigid internal fixation of fractures of the proximal humerus in older patients. J Bone Joint Surg Br 2000;82:1107-12. [Google Scholar | PubMed]
- 7.Zyto K, Ahrengart L, Sperber A, Törnkvist H. Treatment of displaced proximal humeral fractures in elderly patients. J Bone Joint Surg Br 1997;79:412-7. [Google Scholar | PubMed]
- 8.Soler-Peiro M, García-Martínez L, Aguilella L, Perez-Bermejo M. Conservative treatment of 3-part and 4-part proximal humeral fractures: A systematic review. J Orthop Surg Res 2020;15:347. [Google Scholar | PubMed]
- 9.Wijgman AJ, Roolker W, Patt TW, Raaymakers EL, Marti RK. Open reduction and internal fixation of three and four-part fractures of the proximal part of the humerus. J Bone Joint Surg Am 2002;84:1919-25. [Google Scholar | PubMed]
- 10.Clavert P, Adam P, Bevort A, Bonnomet F, Kempf JF. Pitfalls and complications with locking plate for proximal humerus fracture. J Shoulder Elbow Surg 2010;19:489-94. [Google Scholar | PubMed]
- 11.Vrotsou K, Ávila M, Machón M, Mateo-Abad M, Pardo Y, Garin O, et al. Constant-Murley Score: Systematic review and standardized evaluation in different shoulder pathologies. Qual Life Res 2018;27:2217-26. [Google Scholar | PubMed]
- 12.Handoll HH, Elliott J, Thillemann TM, Aluko P, Brorson S. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev 2022;6:CD000434. [Google Scholar | PubMed]
- 13.Edelson G, Safuri H, Salami J, Vigder F, Militianu D. Natural history of complex fractures of the proximal humerus using a three-dimensional classification system. J Shoulder Elbow Surg 2008;17:399-409. [Google Scholar | PubMed]
- 14.Gaebler C, McQueen MM, Court-Brown CM. Minimally displaced proximal humeral fractures: Epidemiology and outcome in 507 cases. Acta Orthop Scand 2003;74:580-5. [Google Scholar | PubMed]
- 15.Neer CS 2nd. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am 1970;52:1077-89. [Google Scholar | PubMed]
- 16.Carofino BC, Leopold SS. Classifications in brief: The neer classification for proximal humerus fractures. Clin Orthop Relat Res 2013;471:39-43. [Google Scholar | PubMed]
- 17.Martin C, Guillen M, Lopez G. Treatment of 2-and 3-part fractures of the proximal humerus using external fixation: A retrospective evaluation of 62 patients. Acta Orthop 2006;77:275-8. [Google Scholar | PubMed]
- 18.Kaushik S. Dr. B.B. Joshi-a visionary hand surgeon. Indian J Plast Surg 2011;44:176-7. [Google Scholar | PubMed]
- 19.Gupta AK, Gupta M, Sengar G, Nath R. Functional outcome of closed fractures of proximal humerus managed by Joshi’s external stabilizing system. Indian J Orthop 2012;46:216-20. [Google Scholar | PubMed]
- 20.Ghosh S, Ghosh D, Datta S, Chaudhuri A, Roy DS, Chowdhury A. External fixation by Joshi’s external stabilizing system in cases of proximal humerus fractures in elderly subjects. J Sci Soc 2013;40:99. [Google Scholar | PubMed]
- 21.Das H, Laskar AH. Results of modified JESS augmentation for fracture proximal humerus stabilized with percutaneous K-wires. INDJST 2019;5:32-5. [Google Scholar | PubMed]