This case emphasizes the need for clinicians to consider the diagnosis of septic arthritis in a patient presenting with joint pain following a urologic procedure.
Dr. Kristina Domanski, Department of Emergency Medicine, Kirk Kerkorian School of Medicine at UNLV, Las Vegas, NV. E-mail: khdomanski@gmail.com
Introduction: Septic arthritis (SA) is a rare clinical entity that can lead to significant morbidity and mortality. Recent years have seen a rise in minimally invasive surgical therapy for the treatment of benign prostatic hyperplasia, including prostatic urethral lift. We report a case of bilateral simultaneous SA of the knees, following a prostatic urethral lift procedure. SA following a urologic procedure has not previously been reported.
Case Report: A 79-year-old male presented to the Emergency Department through an ambulance with bilateral knee pain with associated fever and chills. Two weeks before presentation, he had undergone a prostatic urethral lift, cystoscopy, and Foley catheter placement. The examination was remarkable for bilateral knee effusions. Arthrocentesis was performed, and the synovial fluid analysis was consistent with a diagnosis of SA.
Conclusion: This case emphasizes the need for frontline clinicians to consider SA in patients presenting with joint pain as a rare complication of prostatic instrumentation.
Keywords: Septic arthritis, knee joint, prostatic urethral lift.
Joint pain is a common presentation to the Emergency Department (ED). Septic arthritis (SA) is a rare clinical entity, but an important consideration, as it can lead to significant morbidity and mortality. SA is estimated to have a mortality of 11%, increasing to 50% in the case of polyarticular arthritis [1]. In 2012, SA was diagnosed in approximately 16,000 ED visits, accounting for 0.01% of all visits [2]. Incidence in the US is 6–10 cases/100,000 [3] with 40–50% affecting the knee [4] and 10–20% being polyarticular [3]. An estimated 70% of SA cases are caused by bacteremia, with other causes, including contiguous spread from local infections or direct inoculation from trauma [5]. Benign prostatic hyperplasia (BPH) is a common disease in men. Recent years have seen a rise in minimally invasive surgical therapy (MIST) for the treatment of BPH, including prostatic urethral lift [6,7,8]. We report a case of bilateral simultaneous SA of the knees, following a prostatic urethral lift procedure.
A 79-year-old male presented to the ED through an ambulance with bilateral knee pain with associated fever and chills. He was unable to weight bear due to pain and denied any history of trauma. Symptoms had been present for 2 days. His medical history was significant for diabetes mellitus type II, hypertension, hyperlipidemia, and paroxysmal atrial fibrillation. He reported a surgical history of prostatic urethral lift, cystoscopy, and Foley catheter placement performed 2 weeks before presentation. On arrival, the patient was febrile with an oral temperature of 101.6 F (38.7°C) and tachycardic with a heart rate of 105 bpm. The patient’s bilateral knees were warm to touch with no overlying cellulitis. He had bilateral knee effusions with positive bulge and patellar tap tests. Laboratory studies showed white blood count of 17,700/mL, erythrocyte sedimentation rate of >140 mm/h, and C-reactive protein of 26.70 mg/dL. Blood glucose was 94 mg/dL. Renal function and electrolytes were within normal limits. Arthrocentesis was performed on both knees by the emergency physician. Turbid synovial fluid was aspirated from both knees and sent for analysis. Results of the synovial fluid analysis are shown in Table 1 and are consistent with a diagnosis of SA. The patient was commenced on broad-spectrum antibiotic therapy with vancomycin and piperacillin/tazobactam. The orthopedic service was consulted, and the patient underwent operative management as well as continued antibiotic therapy. The patient was taken for bilateral arthroscopic washout and right knee medial meniscectomy the following day. Intra-operative findings included diffuse synovitis, degenerative changes, and 50–60 cc of purulent fluid in each knee, which was sent for Gram stain and culture. Each knee was lavaged with a total of 6 L normal saline. Synovial fluid samples obtained intra-operatively were again sent for analysis. Results are shown in Table 2. Gram stain was negative. Culture of synovial fluid as well as blood cultures showed no bacterial growth at 7 days. After consultation with the infectious diseases service, the patient was continued on broad-spectrum antibiotics for 7 days. He was discharged to an inpatient rehabilitation facility.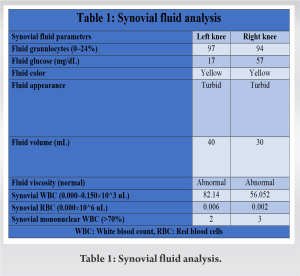
Minimally invasive surgical therapies, including prostatic urethral lift, are increasingly used for the treatment of BPH, and adverse effects are typically mild and transient [9]. Our patient’s history was significant for a prostatic urethral lift procedure, cystoscopy, and placement of a urinary catheter performed 2 weeks before his presentation to the ED. SA is most commonly caused by bacteremia [5]; however, other risk factors include diabetes, intra-articular corticosteroid injections, intravenous drug use, joint prosthesis, rheumatoid arthritis, and osteoarthritis [1]. Our patient had a history of diabetes, and changes consistent with osteoarthritis were noted on arthroscopy during this hospitalization. However, the patient had a surgical history of recent prostatic urethral lift and cystoscopy; after which he had been discharged home with a urinary catheter. Bacteremia following surgical instrumentation of the prostate is well-documented, with 23% of patients developing bacteremia from urine or prostatic flora, following transurethral resection of the prostate (TURP) [10]. It has also been described following transurethral instrumentation as done in other procedures like cystoscopy [1]. In one study, cystoscopy caused bacteremia at a rate of about half that which was found in TURP [9]. Although these studies show that the bacteremia is mostly transient with few cases of septicemia, we speculate that this was the most likely cause of this patient’s illness. SA is primarily caused by Staphylococcus aureus, followed by Streptococcus, making 91% of cases [11]. Other causes include Neisseria gonorrhoeae, fungal infections, mycobacterial, and spirochetes [12]. In this case, no bacterial growth was noted on blood cultures, joint aspirate cultures, or samples obtained during intra-operative washout. One possibility is a SA mimic, like reactive arthritis. However, only 50% of SA cases have a positive Gram stain [11], and culture is only 76% sensitive [13]. This patient had no risk factors for fungal infection, and the authors consider the cause of the patient’s symptoms to be bacterial according to the temporal sequence of events. The patient began to develop symptoms 12 days after a prostatic urethral lift procedure, which may have caused bacteremia and hematogenous spread to his knees. Polyarticular SA is rare. SA of both knees was seen in a patient with surgical wound infection following bicuspid aortic valve replacement. In that case, the hematogenous spread was postulated as the cause [12]. Bilateral pneumococcal SA has been described in an immunocompetent 60-year-old male with no extra-articular infective source, despite a thorough investigation [14].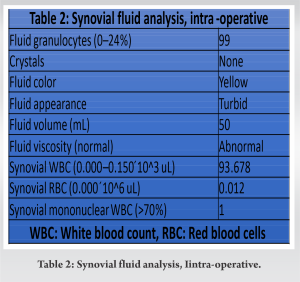
SA following a urologic procedure has never been described. Recent years have seen a rise in MIST for the treatment of BPH, and further research is needed on the post-operative complications of these procedures. This case emphasizes the need for frontline clinicians to consider SA in patients presenting with joint pain following a surgical procedure.
SA is often caused by bacteremia and can lead to significant morbidity and mortality. Bacteremia has been described after surgical instrumentation of the prostate. As minimally invasive surgical therapies are increasingly used in the treatment of BPH, this case emphasizes the need for clinicians to consider the diagnosis of SA in a patient presenting with joint pain following a urologic procedure
References
- 1.Mathews CJ, Weston VC, Jones A, Field M, Coakley G. Bacterial septic arthritis in adults. Lancet 2010;375:846-55. [Google Scholar | PubMed]
- 2.Singh JA, Yu S. Septic arthritis in emergency departments in the US: A national study of health care utilization and time trends. Arthritis Care Res (Hoboken) 2018;70:320-6. [Google Scholar | PubMed]
- 3.Roerdink RL, Huijbregts HJ, van Lieshout AW, Dietvorst M, van der Zwaard BC. The difference between native septic arthritis and prosthetic joint infections: A review of literature. J Orthop Surg (Hong Kong) 2019;27:2309499019860468. [Google Scholar | PubMed]
- 4.Parvizi J, Kim GK. Septic arthritis. In: Parvizi J, Kim GK, editors. High Yield Orthopaedics. United States: W.B. Saunders; 2010. p. 421-2. [Google Scholar | PubMed]
- 5.Long B, Koyfman A, Gottlieb M. Evaluation and management of septic arthritis and its mimics in the emergency department. West J Emerg Med 2019;20:331-41. [Google Scholar | PubMed]
- 6.Denisenko A, Somani B, Agrawal V. Recent advances in UroLift: A comprehensive overview. Turk J Urol 2022;48:11-6. [Google Scholar | PubMed]
- 7.Gao B, Lu S, Bhojani N, Zorn K, Chughtai B, Elterman D. Office-based procedures for BPH. Curr Urol Rep 2021;22:63. [Google Scholar | PubMed]
- 8.Bozkurt A, Karabakan M, Keskin E, Hirik E, Can Balci MB, Nuhoglu B. Prostatic urethral lift: A new minimally invasive treatment for lower urinary tract symptoms secondary to benign prostatic hyperplasia. Urol Int 2016;96:202-6. [Google Scholar | PubMed]
- 9.Shore N, Freedman S, Gange S, Moseley W, Heron S, Tutrone R, et al. Prospective multi-center study elucidating patient experience after prostatic urethral lift. Can J Urol 2014;21:7094-101. [Google Scholar | PubMed]
- 10.Tokunaga S, Ohkawa M, Oshinoya Y, Nakashima T, Hisazumi H, Nishikawa T, et al. Bacteremia from transurethral prostatic resection under prophylactic use of antibiotics. Kansenshogaku Zasshi 1991;65:698-702. [Google Scholar | PubMed]
- 11.Mathews CJ, Coakley G. Septic arthritis: Current diagnostic and therapeutic algorithm. Curr Opin Rheumatol 2008;20:457-62. [Google Scholar | PubMed]
- 12.Horowitz DL, Katzap E, Horowitz S, Barilla-LaBarca ML. Approach to septic arthritis. Am Fam Physician 2011;84:653-60. [Google Scholar | PubMed]
- 13.Chong HH. Bilateral knee septic arthritis: Was it from sternal wound? Clin Case Rep 2018;6:1765-8. [Google Scholar | PubMed]
- 14.Whitehead-Clarke TI, Singavarapu R, Gulihar A, Chettiar K. Bilateral, simultaneous pneumococcal septic arthritis of the knees: A normal immune system, an unknown source. BMJ Case Rep 2016;2016:bcr2016214980. [Google Scholar | PubMed]








