Unusual presentation of giant cell tumor of the proximal phalanx of the hand managed surgically without loss of function and donor-site morbidity.
Dr. Ashish Garg, Department of Orthopaedics, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India. E-mail: ashishgarg30011993@gmail.com
Introduction: The prevalence of giant cell tumor (GCT) of bone is approximately 5% of all primary osseous tumors. It accounts for <2% of the total cases as far as the involvement of the hand is concerned. Numerous studies stated that <1% of cases have phalangeal involvement of the thumb.
Case Report: This case is delineated for its unusual location (thumb proximal phalanx) in a 42-year-old male patient managed by single-stage en-bloc excision, arthrodesis, and web-space deepening procedure without donor-site morbidity. It is known for its notorious nature for reoccurrence (10–50%) and transformation into malignancy (10%); therefore, meticulous dissection is a prerequisite.
Conclusion: GCT of the thumb proximal phalanx is quite an unusual presentation. Although very rare, it is thought to be one of the most aggressive varieties of benign bone tumor observed to date. Amid a high rate of recurrence, careful preoperative planning is pivotal for fruitful outcome both anatomically and functionally.
Keywords: Giant cell tumor, proximal phalanx, extended curettage.
World became introduced to the terminology “giant cell tumor” (GCT) when Joseph Bloodgood coined this term for the 1st time in 1912 [1]. The distal femur and proximal tibia are the most common sites of involvement (55%); the prevalence of GCT in the hand accounts for only 2% of all the manifestations [2]. Patel et al., in their cohort of 2400 cases, found only 2% of cases that were diagnosed with GCT of the hand [3]. It is even rarer when we talk about the involvement of phalanges of the thumb recording 0.11% prevalence [4]. Even though GCT of the thumb shares <1% involvement, it is supposed to be much more aggressive in nature and has a higher rate of recurrence, that is, 30.7% [4,5,6], compared to other giant cell-rich lesions observed at the index location. Only five cases have been published worldwide to date in the best of our search.
A 42-year-old male patient presented to the tertiary care center outpatient department with complaints of pain and swelling of the left thumb for 1 year. Physical examination revealed globular swelling of about 6×4×5 cm with a firm consistency at the proximal phalanx region and interphalangeal joint of the thumb in such a way that bony palpation of the phalanx and joint range of motion cannot be appreciated (Fig. 1). 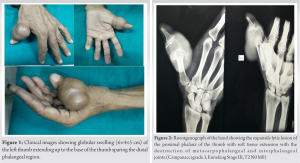 It was gradually progressive in nature and associated with tenderness over the whole of the thumb. The overlying skin was stretched without any adherence to the underlying mass. There was a limitation of the metacarpophalangeal and interphalangeal joint range of motion. The patient gave no history of any constitutional symptoms such as an evening rise in temperature, significant weight loss, and loss of appetite. Radiographs of the left hand with the wrist joint were suggestive of the expansile lytic lesion with a “soap bubble” appearance involving the whole of the proximal phalanx with soft tissue extension and destruction of metacarpophalangeal and interphalangeal joints suggestive of Campanacci grade 3 GCT (Fig. 2). A routine blood workup revealed hemoglobin 8.7 mg/dL, total leukocyte counts 6,800 cells/mm3, erythrocyte sedimentation rate 27 mm/1st h, and highly sensitive C-reactive protein 9 mg/L. Rest other blood investigations were unremarkable. On open biopsy, grossly there was a gray-brown mass with a lobulated appearance following which provisional diagnosis of GCT was made. Histopathology examination revealed multinucleated scattered osteoclastic giant cells interposed between numerous ovoid mononuclear clusters of stromal cells with pale cytoplasm suggestive of GCT (Fig. 3).
It was gradually progressive in nature and associated with tenderness over the whole of the thumb. The overlying skin was stretched without any adherence to the underlying mass. There was a limitation of the metacarpophalangeal and interphalangeal joint range of motion. The patient gave no history of any constitutional symptoms such as an evening rise in temperature, significant weight loss, and loss of appetite. Radiographs of the left hand with the wrist joint were suggestive of the expansile lytic lesion with a “soap bubble” appearance involving the whole of the proximal phalanx with soft tissue extension and destruction of metacarpophalangeal and interphalangeal joints suggestive of Campanacci grade 3 GCT (Fig. 2). A routine blood workup revealed hemoglobin 8.7 mg/dL, total leukocyte counts 6,800 cells/mm3, erythrocyte sedimentation rate 27 mm/1st h, and highly sensitive C-reactive protein 9 mg/L. Rest other blood investigations were unremarkable. On open biopsy, grossly there was a gray-brown mass with a lobulated appearance following which provisional diagnosis of GCT was made. Histopathology examination revealed multinucleated scattered osteoclastic giant cells interposed between numerous ovoid mononuclear clusters of stromal cells with pale cytoplasm suggestive of GCT (Fig. 3). 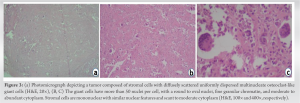 Report did not reveal any evidence suggestive of malignancy. Metabolic workup rules out other differentials which counterfeit GCT, such as aneurysmal bone cyst (ABC), benign chondroblastoma, non-ossifying fibroma (NOF), simple bone cyst (SBC), enchondroma, spina ventosa, and metastasis, and some primary osseous tumors such as chondrosarcoma, osteosarcoma, brown tumor of hyperparathyroidism, and giant cell reparative granuloma (GCRG); the final diagnosis of GCT of the left thumb proximal phalanx was made. On exploration of the swelling, the tumor was found to extend into surrounding soft tissue with involvement of the entire proximal phalanx with metacarpophalangeal and interphalangeal joint (Fig. 4).
Report did not reveal any evidence suggestive of malignancy. Metabolic workup rules out other differentials which counterfeit GCT, such as aneurysmal bone cyst (ABC), benign chondroblastoma, non-ossifying fibroma (NOF), simple bone cyst (SBC), enchondroma, spina ventosa, and metastasis, and some primary osseous tumors such as chondrosarcoma, osteosarcoma, brown tumor of hyperparathyroidism, and giant cell reparative granuloma (GCRG); the final diagnosis of GCT of the left thumb proximal phalanx was made. On exploration of the swelling, the tumor was found to extend into surrounding soft tissue with involvement of the entire proximal phalanx with metacarpophalangeal and interphalangeal joint (Fig. 4). 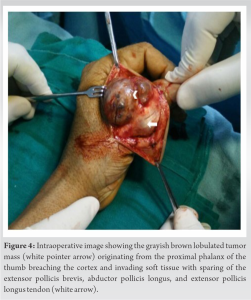 Decision of en-bloc tumor excision was made instead of standard curettage to ensure there was no residual tumor left behind which was confirmed intraoperatively by histopathological assessment of the frozen sections of tissue at both the ends of the void created. It was coming out to be negative (Fig. 5 and 6).
Decision of en-bloc tumor excision was made instead of standard curettage to ensure there was no residual tumor left behind which was confirmed intraoperatively by histopathological assessment of the frozen sections of tissue at both the ends of the void created. It was coming out to be negative (Fig. 5 and 6).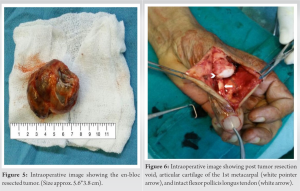 The resulting bone defect was rectified by the fusion of distal phalanx and metacarpal bone with k-wire fixation and application of thumb spica (Fig. 7).
The resulting bone defect was rectified by the fusion of distal phalanx and metacarpal bone with k-wire fixation and application of thumb spica (Fig. 7). The first web-space deepening procedure was also performed to preserve the functionality of the thumb postoperatively. Subsequently, the k-wire was removed 6 weeks postoperatively. Clinically, the wound was healthy. Although there was shortening of the thumb amid arthrodesis of the metacarpophalangeal joint (between the 1st metacarpal and distal phalanx), the patient was able to hold objects and make a fist (Fig. 8). Thus, there occurs no functional morbidity to the patient, which is also explained by the Disabilities of the Arm, Shoulder, and Hand (Quick DASH) score of 17% and Musculoskeletal Tumor Society functional score of 25.
The first web-space deepening procedure was also performed to preserve the functionality of the thumb postoperatively. Subsequently, the k-wire was removed 6 weeks postoperatively. Clinically, the wound was healthy. Although there was shortening of the thumb amid arthrodesis of the metacarpophalangeal joint (between the 1st metacarpal and distal phalanx), the patient was able to hold objects and make a fist (Fig. 8). Thus, there occurs no functional morbidity to the patient, which is also explained by the Disabilities of the Arm, Shoulder, and Hand (Quick DASH) score of 17% and Musculoskeletal Tumor Society functional score of 25.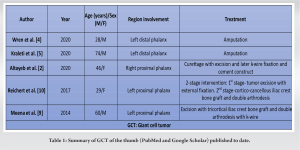
Coopers and Travers described the “GCT” of bone for the 1st time in 1818 [7]. Accounting for 3-5% of all primary benign bone tumors, it mainly originates at epiphysio-metaphyseal region [4].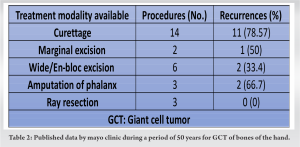 The prevalence of GCT in the thumb is even rarer, accounting for <1% [4,5,6]. According to Wren et al., the prevalence of GCT in the phalanx of the thumb is 0.11% [4]. The majority of the sufferers are skeletally mature females (54%) [8]. In a cohort of 900 GCTs, gender distribution showed that 51.5% of females suffered compared to 48.5% of males [6]. Biscaglia et al. [6], in their study, showed that the average size of the lesions was 5.7*3.1*2.1 cm compared to our case, where the size of the lesion is 6*4*5 cm. Biscaglia et al. [6] conducted a study over eight cases of GCT hand delineated that the majority of the lesions involved epiphysio-metaphyseal region with extension into diaphysis of metacarpal bones compared to our case where the lesion is predominantly of the diaphyseal origin in the proximal phalanx of the thumb. One of the peculiarities GCT of the thumb shares is that it occupies the central diaphyseal region instead of the usual eccentric epiphyseal location in long bones [9]. The rarity of the location could be understood by the fact that no phalangeal lesions were found in the cohort of Biscaglia et al. [6]. Only five cases have been reported worldwide to date summarized in Table 1. To obtain a tumor-free functional hand, one needs to be very vigilant while making the diagnosis and management. The dilemma of multiple lesions mimicking GCT on roentgenography often creates a problem to proceed toward the right path. Radiological differentials such as ABC, GCRG, NOF, SBC, chondroblastoma, brown tumor of hyperparathyroidism, and malignancy [10] should always rule out by histopathological analysis of the lesion by biopsy. However, Biscaglia et al. [6] stated that even if the radiological presentation is nonspecific, it is assumed that a giant cell-rich lesion in the skeletally mature long bone epiphyseal region favored the diagnosis as GCT. On the contrary, similar lesions at the meta-diaphyseal region of a skeletally immature patient go toward GCRG or ABC [6]. It is of immense importance to consider the “diagnostic areas” characterized by “round-oval cells” together making giant cells when seeing slides under a microscope [6]. Areas having spindle-shaped cells in the stroma signify GCRG and solid ABC [6]. In the present case also, few spindle-shaped cells were found; however, the recognition of the diagnostic area allowed to make an appropriate diagnosis. Although not new, as this overlapping phenomenon was observed in 13.7% of the cases in a cohort of 29 GCT, its identification is pivotal to avoid confusion [6]. GCT of phalanges of the hand originates from diaphysis but frequently invades nearby soft tissue after penetrating the cortex which appeared like “paper thin” and having a “ballooned appearance” on roentgenograph, making it less suitable for simple curettage procedure [10]. A similar finding was there in our patient also. GCT of phalanx usually presents with high Campanacci grading [2]. Ropares, in his cohort of 214 GCTs, found only three GCTs of the phalanx; everyone presented with the Campanacci grade 3 [2] similar to what our patient presented with. There is no standardization for the management of phalangeal GCT [2,5]. The methodology to adopt depends on several factors such as the location of the tumor (bone), extent of involvement (zone) to the joint and soft tissue, grade of tumor, and functional requirements of the patient, which are to be negotiated with high risk of recurrence (risk–benefit ratio). Discussing various treatment modalities and the associated rate of recurrence becomes a game changer in the long-term outcome as shown in Table 2 [11]. Since curettage of phalangeal GCT recorded a 79% chance of recurrence [11], there are certain tools which were used to augment the curettage, such as phenol, argon beam, liquid nitrogen, and polymethyl methacrylate cement [2]. However, studies showed that curettage and bone grafting are not effective to cater GCT of the thumb, which is known to have a very high recurrence rate [9]. Since our patient had Campanacci grade 3 thumb proximal phalanx GCT with soft tissue involvement, we do not have the option of curettage and bone grafting. Performing wide/en-bloc excision of the tumor with arthrodesis of the distal phalanx with the head of the 1st metacarpal and 1st web-space deepening [4] not only removes the tumor (intra-op frozen section were negative) but at the same time saves the thumb and functionality of the hand without adding any donor-site morbidity of bone graft.
The prevalence of GCT in the thumb is even rarer, accounting for <1% [4,5,6]. According to Wren et al., the prevalence of GCT in the phalanx of the thumb is 0.11% [4]. The majority of the sufferers are skeletally mature females (54%) [8]. In a cohort of 900 GCTs, gender distribution showed that 51.5% of females suffered compared to 48.5% of males [6]. Biscaglia et al. [6], in their study, showed that the average size of the lesions was 5.7*3.1*2.1 cm compared to our case, where the size of the lesion is 6*4*5 cm. Biscaglia et al. [6] conducted a study over eight cases of GCT hand delineated that the majority of the lesions involved epiphysio-metaphyseal region with extension into diaphysis of metacarpal bones compared to our case where the lesion is predominantly of the diaphyseal origin in the proximal phalanx of the thumb. One of the peculiarities GCT of the thumb shares is that it occupies the central diaphyseal region instead of the usual eccentric epiphyseal location in long bones [9]. The rarity of the location could be understood by the fact that no phalangeal lesions were found in the cohort of Biscaglia et al. [6]. Only five cases have been reported worldwide to date summarized in Table 1. To obtain a tumor-free functional hand, one needs to be very vigilant while making the diagnosis and management. The dilemma of multiple lesions mimicking GCT on roentgenography often creates a problem to proceed toward the right path. Radiological differentials such as ABC, GCRG, NOF, SBC, chondroblastoma, brown tumor of hyperparathyroidism, and malignancy [10] should always rule out by histopathological analysis of the lesion by biopsy. However, Biscaglia et al. [6] stated that even if the radiological presentation is nonspecific, it is assumed that a giant cell-rich lesion in the skeletally mature long bone epiphyseal region favored the diagnosis as GCT. On the contrary, similar lesions at the meta-diaphyseal region of a skeletally immature patient go toward GCRG or ABC [6]. It is of immense importance to consider the “diagnostic areas” characterized by “round-oval cells” together making giant cells when seeing slides under a microscope [6]. Areas having spindle-shaped cells in the stroma signify GCRG and solid ABC [6]. In the present case also, few spindle-shaped cells were found; however, the recognition of the diagnostic area allowed to make an appropriate diagnosis. Although not new, as this overlapping phenomenon was observed in 13.7% of the cases in a cohort of 29 GCT, its identification is pivotal to avoid confusion [6]. GCT of phalanges of the hand originates from diaphysis but frequently invades nearby soft tissue after penetrating the cortex which appeared like “paper thin” and having a “ballooned appearance” on roentgenograph, making it less suitable for simple curettage procedure [10]. A similar finding was there in our patient also. GCT of phalanx usually presents with high Campanacci grading [2]. Ropares, in his cohort of 214 GCTs, found only three GCTs of the phalanx; everyone presented with the Campanacci grade 3 [2] similar to what our patient presented with. There is no standardization for the management of phalangeal GCT [2,5]. The methodology to adopt depends on several factors such as the location of the tumor (bone), extent of involvement (zone) to the joint and soft tissue, grade of tumor, and functional requirements of the patient, which are to be negotiated with high risk of recurrence (risk–benefit ratio). Discussing various treatment modalities and the associated rate of recurrence becomes a game changer in the long-term outcome as shown in Table 2 [11]. Since curettage of phalangeal GCT recorded a 79% chance of recurrence [11], there are certain tools which were used to augment the curettage, such as phenol, argon beam, liquid nitrogen, and polymethyl methacrylate cement [2]. However, studies showed that curettage and bone grafting are not effective to cater GCT of the thumb, which is known to have a very high recurrence rate [9]. Since our patient had Campanacci grade 3 thumb proximal phalanx GCT with soft tissue involvement, we do not have the option of curettage and bone grafting. Performing wide/en-bloc excision of the tumor with arthrodesis of the distal phalanx with the head of the 1st metacarpal and 1st web-space deepening [4] not only removes the tumor (intra-op frozen section were negative) but at the same time saves the thumb and functionality of the hand without adding any donor-site morbidity of bone graft.
GCT of the proximal phalanx of the thumb is quite a rare tumor encountered to date. Meticulous en-bloc resection with the fusion of distal phalanx and 1st metacarpal bone without violating the extensor and flexor tendons could result in functional sparing postoperatively and negates the donor-site morbidity of the bone grafting. Web-space deepening not only compensates for anatomical shortening of the thumb but also provides an additional lever arm necessary for holding the objects.
GCT of proximal phalanx although very rare, thought to be one of the most aggressive varieties of benign bone tumor observed with an estimated rate of reoccurrence (10–50%) and transforms into malignancy (10%). Extended curettage and reconstruction with autograft or allograft remain the mainstay treatment modality resulting in a prolonged rehabilitation period and donor-site morbidity. In this case, soft tissue procedure (web-space deepening) behaves as an alternative to bone grafting to obtain the lever arm necessary to maintain the functionality of the thumb.
References
- 1.McCarthy EF. Giant-cell tumor of bone: An historical perspective. Clin Orthop Relat Res 1980;153:14-25. [Google Scholar | PubMed]
- 2.Altayeb M, Shaheen M, Abduljawad S, Pant R. Giant cell tumor in the proximal phalanges of the hand: A report of two cases treated with a nonbiological construct. J Musculoskelet Surg Res 2021;5:62. [Google Scholar | PubMed]
- 3.Patel MR, Desai SS, Gordon SL, Nimberg GA, Sclafani SJ, Vigorita VJ, et al. Management of skeletal giant cell tumors of the phalanges of the hand. J Hand Surg Am 1987;12:70-7. [Google Scholar | PubMed]
- 4.Wren E, Goodwin TM, Brazier BG, Marinas E, Katranji A. A case report of giant cell tumor in the thumb distal phalanx. J Orthop Case Rep 2020;10:84-7. [Google Scholar | PubMed]
- 5.Kraleti S, Manyam S, Dawson K. Giant cell tumor of the bone presenting as swelling of the thumb. Proc (Bayl Univ Med Cent) 2021;34:307-8. [Google Scholar | PubMed]
- 6.Biscaglia R, Bacchini P, Bertoni F. Giant cell tumor of the bones of the hand and foot. Cancer 2000;88:2022-32. [Google Scholar | PubMed]
- 7.Jogani A, Rathod T, Sujith BS, Mohanty SS, Panchal S, Rathod R. Bicentric synchronous giant cell tumor: A rare managed case report of bilateral fibula neck tumor. J Orthop Case Rep 2020;10:22-4. [Google Scholar | PubMed]
- 8.Werner M. Giant cell tumour of bone: Morphological, biological and histogenetical aspects. Int Orthop 2006;30:484-9. [Google Scholar | PubMed]
- 9.Meena U, Sharma Y, Saini N, Meena D, Gahlot N. Giant cell tumours of hand bones: A report of two cases. J Hand Microsurg 2016;7:177-81. [Google Scholar | PubMed]
- 10.Reichert P, Kowalski P, Gosk J. The giant cell tumour of the proximal phalanx of the thumb treated by a 2-stage operation. Acta Orthop Traumatol Turc 2017;51:425-8. [Google Scholar | PubMed]
- 11.Athanasian EA, Wold LE, Amadio PC. Giant cell tumors of the bones of the hand. J Hand Surg Am 1997;22:91-8. [Google Scholar | PubMed]







