Bilateral femur fractures are a rare injury pattern in nonambulatory children that strongly suggest nonaccidental trauma; patients greater than 6 months of age with significant comorbidities may be successfully treated with a Pavlik harness.
Dr. Anthony M Padgett, Department of Orthopaedic Surgery, University of Alabama Birmingham Heersink School of Medicine, 1600 7th Avenue South, Lowder Suite 316, Birmingham 35233, Alabama. E-mail: a.m.padgett2@gmail.com
Introduction: Bilateral femoral diaphyseal fractures in children due to nonaccidental trauma (NAT) are a rare occurrence, with no reported cases currently published in the literature. The authors present a case of an 8-month-old male who presented with bilateral femoral shaft fractures. History, physical examination, and radiographic findings support NAT as the cause of his injuries. Due to the patient’s size and associated comorbidities, he was initially treated with Pavlik harness placement, rather than spica casting. The patient demonstrated appropriate radiographic evidence of fracture healing on follow-up.
Case Report: An 8-month-old male with a complex past medical history presents to the emergency department. Per the patient’s mother, he has been demonstrating a progressive loss of movement and refusal to bear weight in his bilateral lower extremities over the preceding 1–2 weeks. Other injuries include facial bruising and lesions indicative of subconjunctival hemorrhages. After orthopedics was consulted, the decision was made to treat the patient’s bilateral femoral shaft fractures with a Pavlik harness, rather than spica casting, due to his small size and associated past medical history. The patient was subsequently discharged under foster care. Follow-up visit demonstrates appropriate fracture healing in the bilateral femoral diaphyses.
Conclusion: Many cases of NAT in the pediatric population are initially missed. Orthopedic providers must maintain a high index of suspicion for NAT as many of these patients will present with musculoskeletal injuries. The authors report a rare case of NAT in a male child resulting in bilateral femoral diaphyseal fractures. The patient was successfully treated through Pavlik harness placement. Orthopedic providers should consider Pavlik harness placement as a viable option even for young children >6 months of age presenting with femoral shaft fractures if spica casting or open reduction internal fixation is not appropriate.
Keywords: Femoral fracture, nonaccidental trauma, pediatric.
Pediatric femoral fractures are relatively common injuries with an annual incidence of approximately 19/100,000 [1]. Bilateral femoral fractures, however, are much less common injuries with an unknown incidence. Femoral fractures are present in a bimodal fashion, and the etiology is age-dependent. Early femoral fractures occur between 2 and 3 years when the child starts walking; however, the femoral cortex is thin. Falls remain the major cause up to age 6, at which point pedestrians hit by vehicles becomes the major cause. For ages 13–15, fractures occur as passengers are involved in road traffic accidents [2]. Low-energy fractures are rare and are usually due to genetic, metabolic, or endocrine disorders [3]. Nonaccidental trauma (NAT) was registered in 7% of the femoral fractures in children < 3 years, a percentage at variance with earlier reports [4,5]. Young age is a strong predictor of nonaccidental pediatric femoral fractures [6], with up to 60% of femoral fractures in infants < 1 year old due to suspected or confirmed child abuse [7,8]. NAT should be suspected in children younger than walking age, and a detailed history, physical examination, fracture characterization, and injury scene investigation should be conducted for a thorough assessment of the cause of injury [9]. From previous studies, non-surgical treatment is the most common treatment in younger age groups, and surgical treatment increased with age [10]. Infantile femoral diaphyseal fractures are usually immediately treated with a simple splint to provide stability and reduce pain [11], followed by the application of a Pavlik harness to immobilize the injured femur while maintaining an optimal position for the reduction of the femur [12]. Immobilization with a Pavlik harness serves as an excellent standard for the management of femoral shaft fractures in neonates [12,13], as it allows rapid callus formation with minimal complications [14]. The current literature is limited on bilateral femoral fractures in the pediatric population. A comprehensive literature search was performed to identify all reported cases of bilateral femoral fractures resulting from NAT in the pediatric population. To the authors’ knowledge, there are no reports to date of bilateral femoral fractures due to NAT. All relevant studies in Cochrane Library, Medline/PubMed, and EMBASE (Elsevier) were searched from inception to April 21, 2022, using medical subject headings and text words without limitations on language or study type. The authors present the unique case of an 8-month-old with bilateral femoral shaft fractures resulting from NAT who demonstrated appropriate fracture healing following Pavlik harness placement.
The patient was an 8-month-old male with a past medical history of premature birth at 26 weeks, bilateral grade III intraventricular hemorrhage leading to hydrocephalus status post shunt placement, oropharyngeal dysphagia, and hypertension, who initially presented to the emergency department for poor feeding and was subsequently found to have VP shunt malfunction and several injuries concerning for NAT. These injuries included bilateral femoral fractures, facial bruising, and subconjunctival hemorrhages. The patient has a history of recurrent hospitalizations and has been following up with multiple different specialties, most notably neurosurgery and gastrointestinal. The patient’s mother reported that 1–2 weeks before presenting to the emergency department, she noticed the patient came home from day care 1 day not moving his legs as much and refusing to bear weight on his legs when she would lift him up. She denied any known injuries at the time or increased fussiness. The mother also noticed around that time that he had a dark brown mark on the left side of his face, as well as a red spot on his eye. Due to poor oral intake, she decided to go to the emergency department. Of note, the patient’s mother denies knowledge of any recent injuries, including accidental falls, motor vehicle accidents, or previous problems with bleeding. On physical examination, the patient was noted to be cachectic-appearing, and the admission weight was 5.7 kg. He was also noted to have a hyperpigmented area on the side of his face concerning bruising and subconjunctival hemorrhages. On musculoskeletal examination, the patient had bilateral legs flexed outward at the hips and knees. The patient cried with movements of the legs. The dorsalis pedis pulses were 2+ bilaterally. The skeletal survey obtained showed fractures in the proximal diaphysis of the right femur and proximal diaphysis of the left femur (Fig. 1 and 2).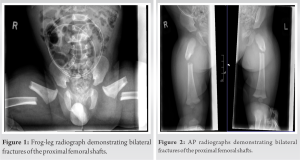 Both fractures had angular deformities with apices pointing anteriorly and laterally. There was soft tissue swelling in the right and left thigh. The fractures appear to have happened simultaneously. No osteopenia or Wormian bones was detected. After orthopedics was consulted, the plan was to initiate a large Pavlik harness. The lower extremities were wrapped in a frog-leg position. The size was based on the manufacturer’s sizing chart. Specific recommendations included non-weight bearing of bilateral lower extremities, genetics consultation, and obtaining a full metabolic workup for possible metabolic bone disorders. We did not restrict the patient’s positioning following Pavlik harness placement. Physical therapy and occupational therapy were consulted to expedite the patient’s recovery process during his stay. After initiating the harness, a repeat skeletal survey was obtained 8 days after the initial presentation, which showed callus formation on the left femur fracture indicative of a partial healing process. There was also a progressive callus seen about the proximal right femur fracture that was compatible with healing. 2 weeks after the initial presentation, a right and left femur X-ray with a two-sided view of anterior–posterior and lateral obtained revealed a left femur fracture with about one shaft width dorsal displacement distal fracture fragment and lateral angulation of the distal fracture fragment (Fig. 3 and 4).
Both fractures had angular deformities with apices pointing anteriorly and laterally. There was soft tissue swelling in the right and left thigh. The fractures appear to have happened simultaneously. No osteopenia or Wormian bones was detected. After orthopedics was consulted, the plan was to initiate a large Pavlik harness. The lower extremities were wrapped in a frog-leg position. The size was based on the manufacturer’s sizing chart. Specific recommendations included non-weight bearing of bilateral lower extremities, genetics consultation, and obtaining a full metabolic workup for possible metabolic bone disorders. We did not restrict the patient’s positioning following Pavlik harness placement. Physical therapy and occupational therapy were consulted to expedite the patient’s recovery process during his stay. After initiating the harness, a repeat skeletal survey was obtained 8 days after the initial presentation, which showed callus formation on the left femur fracture indicative of a partial healing process. There was also a progressive callus seen about the proximal right femur fracture that was compatible with healing. 2 weeks after the initial presentation, a right and left femur X-ray with a two-sided view of anterior–posterior and lateral obtained revealed a left femur fracture with about one shaft width dorsal displacement distal fracture fragment and lateral angulation of the distal fracture fragment (Fig. 3 and 4).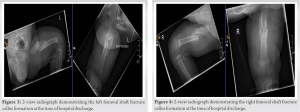 Subtotal callus about the fracture site was compatible with partial healing. On the day of discharge, the patient went home with a spica harness, and his foster mother was educated on using the harness, as well as patient handling in supine, sitting, and held positions. A follow-up appointment was scheduled for 1 month after discharge. Two-view radiographs obtained at that visit demonstrated evidence of healing of his bilateral femoral shaft fractures with good bony callus and bridging bone formation between the two fractures (Fig. 5 and 6). Some amount of remodeling had already occurred.
Subtotal callus about the fracture site was compatible with partial healing. On the day of discharge, the patient went home with a spica harness, and his foster mother was educated on using the harness, as well as patient handling in supine, sitting, and held positions. A follow-up appointment was scheduled for 1 month after discharge. Two-view radiographs obtained at that visit demonstrated evidence of healing of his bilateral femoral shaft fractures with good bony callus and bridging bone formation between the two fractures (Fig. 5 and 6). Some amount of remodeling had already occurred.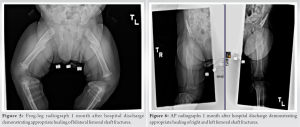
The incidence of bilateral femoral fractures due to NAT is a rare phenomenon in the pediatric population, with no cases currently published in the literature. Our patient’s bilateral femoral shaft fractures and associated physical examination and radiographic findings strongly support NAT as the cause of his injuries. Musculoskeletal injuries are the second-most common injuries seen in children with NAT, after soft-tissue injuries. As a result, 30%-50% of these children are seen by orthopedic surgeons [15]. It is important to maintain a high index of suspicion for NAT as the diagnosis is missed in up to 20% of children at the initial presentation [15,16]. Physical examination and radiographic findings in children with NAT include subdural hematomas, conjunctival hemorrhages, posterior rib fractures, fractures in different stages of healing, long bone fractures in young or nonambulatory patients, and metaphyseal corner fractures. Social factors such as parental drug abuse, lower socioeconomic status, and single-parent households have also been shown to correlate with a higher incidence of NAT [15]. Treatment of pediatric diaphyseal femoral fractures varies depending on age [17]. Initial treatment with a Pavlik harness, rather than spica casting, was used in this case due to the patient’s small size and history of failure to thrive. The complication rates associated with Pavlik harness placement are minimal, but providers should thoroughly consider parental reliability and follow-up when utilizing this treatment option [13,14]. Throughout the course of our patient’s hospitalization, we consulted the expertise of multiple specialties to address the patient’s nonorthopedic ailments. This multidisciplinary approach will hopefully decrease the morbidity associated with the patient’s NAT and increase his long-term quality of life.
Providers must maintain a high index of suspicion for NAT in pediatric patients. Long bone fractures in nonambulatory children should raise a strong suspicion for NAT. Prompt diagnosis and treatment of these fractures are essential. It is important to address both the orthopedic injuries and other physical and social needs of the patient through a multidisciplinary approach.
Lower extremity fractures are a common injury seen in children as a result of NAT. However, bilateral lower extremity fractures are a much less common presentation. This report documents a case in which an 8-month-old male presented with bilateral femoral diaphyseal fractures. There are currently no reported cases in the literature of this phenomenon. The patient demonstrated appropriate fracture healing following the placement of a Pavlik harness.
References
- 1.Hinton RY, Lincoln A, Crockett MM, Sponseller P, Smith G. Fractures of the femoral shaft in children. Incidence, mechanisms, and sociodemographic risk factors. J Bone Joint Surg Am 1999;81:500-9. [Google Scholar | PubMed]
- 2.Lindisfarne EA, Ayodele O. Non-accidental injury, femoral shaft and neck fractures in children. Surgery (Oxford) 2020;38:568-80. [Google Scholar | PubMed]
- 3.Ju DG, Mogayzel PJ, Sponseller PD, Familiari F, McFarland EG. Bilateral midshaft femoral fractures in an adolescent baseball player. J Cyst Fibros 2016;15:e41-3. [Google Scholar | PubMed]
- 4.von Heideken J, Svensson T, Blomqvist P, Haglund-Åkerlind Y, Janarv PM. Incidence and trends in femur shaft fractures in Swedish children between 1987 and 2005. J Pediatr Orthop 2011;31:512-9. [Google Scholar | PubMed]
- 5.Loder RT, O’Donnell PW, Feinberg JR. Epidemiology and mechanisms of femur fractures in children. J Pediatr Orthop 2006;26:561-6. [Google Scholar | PubMed]
- 6.Schwend RM, Werth C, Johnston A. Femur shaft fractures in toddlers and young children: Rarely from child abuse. J Pediatr Orthop 2000;20:475-81. [Google Scholar | PubMed]
- 7.Thomas SA, Rosenfield NS, Leventhal JM, Markowitz RI. Long-bone fractures in young children: Distinguishing accidental injuries from child abuse. Pediatrics 1991;88:471-6. [Google Scholar | PubMed]
- 8.Gross RH, Stranger M. Causative factors responsible for femoral fractures in infants and young children. J Pediatr Orthop 1983;3:341-3. [Google Scholar | PubMed]
- 9.Pierce MC, Bertocci GE, Janosky JE, Aguel F, Deemer E, Moreland M, et al. Femur fractures resulting from stair falls among children: An injury plausibility model. Pediatrics 2005;115:1712-22. [Google Scholar | PubMed]
- 10.Hunter JB. Femoral shaft fractures in children. Injury 2005;36:S86-93. [Google Scholar | PubMed]
- 11.Schenk R. In: Weber BG, Brunner Ch, Frueler F, editors. Treatment of Fractures in Children and Adolescents. Berlin, Heidelberg: Springer; 1980. [Google Scholar | PubMed]
- 12.Stannard JP, Christensen KP, Wilkins KE. Femur fractures in infants: A new therapeutic approach. J Pediatr Orthop 1995;15:461-6. [Google Scholar | PubMed]
- 13.Rush JK, Kelly DM, Sawyer JR, Beaty JH, Warner WC. Treatment of pediatric femur fractures with the Pavlik harness: Multiyear clinical and radiographic outcomes. J Pediatr Orthop 2013;33:614-7. [Google Scholar | PubMed]
- 14.Podeszwa DA, Mooney JF, Cramer KE, Mendelow MJ. Comparison of Pavlik harness application and immediate spica casting for femur fractures in infants. J Pediatr Orthop 2004;24:460-2. [Google Scholar | PubMed]
- 15.Azar FM, Beaty JH, Daugherty K, Jones L, Campbell WC, Sawyer JR, et al. Fractures and dislocations in children. In: Campbell’s Operative Orthopaedics. Netherlands: Elsevier; 14th ed. 2021. p. 1492-639. [Google Scholar | PubMed]
- 16.Grossman J, Giliberti B, Dolitsky R, Parker G, Kim B, Kutzarov K, et al. Pediatric orthopedic trauma. Pediatr Clin North Am 2020;67:101-18. [Google Scholar | PubMed]
- 17.Kocher MS, Sink EL, Blasier RD, Luhmann SJ, Mehlman CT, Scher DM, et al. American Academy of Orthopaedic Surgeons Clinical Practice guideline on treatment of pediatric diaphyseal femur fracture. J Bone Joint Surg Am 2010;92:1790-2. [Google Scholar | PubMed]








