Practitioners should be mindful of the potential post-reduction complications with prompt consultation of vascular and orthopedic surgery services after prolonged vascular ischemia.
Dr. Zachary Donato, Department of Orthopaedic Surgery, University of Miami Miller School of Medicine, 1600 NW 10th Ave, Miami, Florida 33136, United States. E-mail: z.donato@med.miami.edu
Introduction: While commonly caused by traumatic injury and fracture, compartment syndrome can also result from reperfusion injury. Very few cases of prophylactic fasciotomy are mentioned when considering time to revascularization after prolonged vascular ischemia. We present a case of a patient who underwent multiple compartment prophylactic fasciotomies following reperfusion injury in the upper extremity.
Case Report: We report a 72-year-old male that suffered from an anterior shoulder dislocation after a ground-level fall. After reduction, pulses were not measurable, and angiography indicated an axillary artery occlusion. Immediately after operative reperfusion, compartments became tense. Orthopedic surgeons subsequently performed arm anterior, posterior, and forearm volar and mobile wad compartment fasciotomies, after 13 h of ischemia. The patient tolerated the procedure, and at the latest follow-up, was working to improve strength in the extremity.
Conclusion: Even when the circumstances of injury seem to be less traumatic as in this case of a ground-level fall, we document the importance of prompt recognition and intervention of suspected compartment syndrome following prolonged ischemia and revascularization of the upper extremity.
Keywords: Compartment syndrome, reperfusion injury, shoulder dislocation, axillary artery occlusion, fasciotomy.
Compartment syndrome is a surgical emergency that occurs when the pressure within a muscular compartment rises higher than the perfusion pressure. While commonly caused by traumatic injury and fracture, it can also result from reperfusion injury, which occurs secondary to inflammation that develops after blood supply is returned following prolonged ischemia [1]. His phenomenon is well documented in the lower extremity, with some indications for the consideration of prophylactic fasciotomy [2-4]. Very few cases of prophylactic fasciotomy are mentioned when considering the time to revascularization after prolonged ischemia due to arterial injury in the upper extremity [5-8]. This highlights the need for further evaluation of reperfusion injury and the indications for fasciotomy in the upper extremity. Herein, we present a case report on a patient who underwent multiple compartment fasciotomies following an axillary artery occlusion following shoulder dislocation and perform a review of the current literature on prophylactic fasciotomy for reperfusion injuries in the upper extremity.
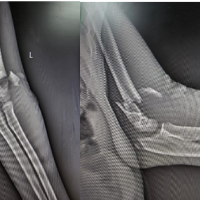
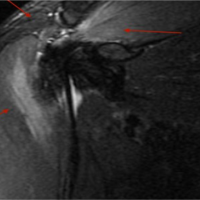
A 72-year-old man with a past medical history of hypertension and morbid obesity presented to the emergency department immediately after sustaining a ground-level fall complaining of left shoulder pain and complete loss of sensation in his left hand. The patient had sluggish capillary refill of his left hand as well as palpable but weak radial pulse. His left shoulder and upper arm were edematous but soft with ecchymosis about the axilla. At this point, the patient was able to actively move his left arm at the elbow and wrist. Plain radiographs of the shoulder showed a left anterior shoulder dislocation with no fractures. Within 1 h of presentation, a left shoulder reduction was attempted by an emergency medicine physician under conscious sedation, but this was aborted when the patient became apneic. Immediately after this attempt, there were no palpable radial, ulnar, or brachial pulses. Both vascular surgery and orthopedic surgery were then consulted. The patient was immediately intubated and emergently taken to perform a computed tomography angiography (CTA) of the chest and left upper extremity and then to the operating room for a closed reduction. Exam under anesthesia demonstrated that the patient had full unrestricted passive shoulder range of motion, and the fluoroscopic view of the humeral head was stable to external rotation in both neutral and 90° abduction. Post-operatively, upon evaluation by vascular surgery, the left upper extremity was cool to touch and no brachial, radial, or ulnar pulses or signals could be obtained with Doppler ultrasound. The finalized interpretation of the CTA indicated left axillary and subclavian artery occlusion (Fig. 1). The vascular surgery service then emergently transferred the patient to the partnering institution for operative management. Upon arrival at the Level I trauma center, 7 h after initial presentation, the left shoulder had a large hematoma in the left axillary artery region. The shoulder compartments were full but compressible, and the forearm and hand compartments were soft and compressible. At this time, the vascular surgeons performed a left upper extremity angiogram demonstrating extravasation of contrast at the level of the axillary artery, with patent brachial, ulnar, and radial arteries. They subsequently performed the placement of two left stents across the area of axillary artery injury. Soon after, brisk blood flow was noted through the entire extremity. The orthopedic surgery service was consulted intraoperatively by the vascular surgeons to assess the need for fasciotomy. Intraoperatively after revascularization, at 14 h after original presentation, the patient was noted to have tense upper arm compartments. The orthopedic surgeons proceeded with left upper arm anterior and posterior compartment fasciotomies. During the case, the forearm became significantly more swollen and tense. Due to this change in examination, the surgeons proceeded with forearm volar compartment fasciotomy through a volar approach. This included all volar compartments and the mobile wad compartment. The dorsal compartment was not released as it appeared soft and compressible. The radial artery was then identified and noted to have a strong pulse. Post-operatively the patient continued to have a strong radial pulse and Doppler signal. The elbow was held in extension to facilitate adequate blood flow. The patient returned to the operating room 4 days later for irrigation and debridement of the fasciotomy sites. The patient subsequently returned to the operating room 3 days later for a repeat irrigation and debridement followed by closure of the fasciotomies. The patient was discharged home 10 days after his arrival, with his left upper extremity adequately perfused, motor and sensation grossly intact, and palpable distal pulses. At the latest follow-up 13 months post-operatively, imaging was performed and demonstrated no acute fracture, dislocation, or osteonecrosis (Fig. 2).
The vascular surgery service then emergently transferred the patient to the partnering institution for operative management. Upon arrival at the Level I trauma center, 7 h after initial presentation, the left shoulder had a large hematoma in the left axillary artery region. The shoulder compartments were full but compressible, and the forearm and hand compartments were soft and compressible. At this time, the vascular surgeons performed a left upper extremity angiogram demonstrating extravasation of contrast at the level of the axillary artery, with patent brachial, ulnar, and radial arteries. They subsequently performed the placement of two left stents across the area of axillary artery injury. Soon after, brisk blood flow was noted through the entire extremity. The orthopedic surgery service was consulted intraoperatively by the vascular surgeons to assess the need for fasciotomy. Intraoperatively after revascularization, at 14 h after original presentation, the patient was noted to have tense upper arm compartments. The orthopedic surgeons proceeded with left upper arm anterior and posterior compartment fasciotomies. During the case, the forearm became significantly more swollen and tense. Due to this change in examination, the surgeons proceeded with forearm volar compartment fasciotomy through a volar approach. This included all volar compartments and the mobile wad compartment. The dorsal compartment was not released as it appeared soft and compressible. The radial artery was then identified and noted to have a strong pulse. Post-operatively the patient continued to have a strong radial pulse and Doppler signal. The elbow was held in extension to facilitate adequate blood flow. The patient returned to the operating room 4 days later for irrigation and debridement of the fasciotomy sites. The patient subsequently returned to the operating room 3 days later for a repeat irrigation and debridement followed by closure of the fasciotomies. The patient was discharged home 10 days after his arrival, with his left upper extremity adequately perfused, motor and sensation grossly intact, and palpable distal pulses. At the latest follow-up 13 months post-operatively, imaging was performed and demonstrated no acute fracture, dislocation, or osteonecrosis (Fig. 2).  All incisions were healed. The patient demonstrated the ability to perform all activities of daily living with no complaints and could perform flexion of the left shoulder to 80° abduction of the left shoulder to sixty degrees, external rotation to ten degrees, and internal rotation to the lumbar spine. He continues to perform physical therapy to improve his range of motion and strength.
All incisions were healed. The patient demonstrated the ability to perform all activities of daily living with no complaints and could perform flexion of the left shoulder to 80° abduction of the left shoulder to sixty degrees, external rotation to ten degrees, and internal rotation to the lumbar spine. He continues to perform physical therapy to improve his range of motion and strength.
Compartment syndrome is a surgical emergency that requires immediate recognition and repair with a decompressive fasciotomy. While diagnosis is clinically based, measurement of compartment pressures is a useful adjunct in equivocal cases or in those with a sedated patient. A delta pressure (diastolic-compartment pressure) <30 mmHg is highly specific for compartment syndrome. Arterial ischemia as a cause of compartment syndrome is well documented in the lower extremity; however, there are not many studies discussing its prevalence in the upper extremity. Numerous occluded arteries in the upper extremity have been documented as causes of reperfusion injury and subsequent compartment syndrome. Injury to the brachial artery specifically is a more common cause of compartment syndrome. Zellweger et al. studied 124 cases of surgically managed brachial artery injuries, and Ekim and Tuncer studied 49 patients also treated with surgical repair of brachial artery injuries [6,7]. The rate of fasciotomy for impending or established compartment syndrome in these studies was about 12%. Other studies demonstrate ranges of compartment syndrome due to reperfusion injury in the upper extremity from 6.7% to 29.3% with multiple varying arteries occluded (Table 1) [6, 7, 9-13].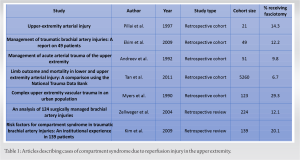 In a prospective study by Dragas et al. dealing with cases of traumatic arterial damage of the upper extremity, the brachial artery was the artery damaged in 55% of cases, followed by the axillary artery in 21.7% [8]. There were 9.6% of patients who demonstrated impending or established compartment syndrome and were treated with fasciotomy. In our case, the axillary artery was occluded due to contusion, secondary to an anterior shoulder dislocation. Similar axillary artery injury following closed reduction of an anterior shoulder dislocation was described in a 2018 case report by Magister et al. [14] Just as in our case, during attempts at closed reduction, the patient became apneic, was intubated, and transferred to the nearest level I trauma center. Upon transfer, distal pulses were still present while CT angiography demonstrated an axillary artery occlusion. Vascular surgeons performed a common carotid artery to mid-brachial artery bypass allograft and orthopedic surgeons performed prophylactic arm and forearm fasciotomies and carpal tunnel release due to swelling noted more distally in the hand. In our case, the forearm and the upper arm compartments were treated with fasciotomy with satisfactory outcome upon discharge. This multicompartmental compartment syndrome is likely an effect of the location of the injury on the axillary artery, as it is more proximal to the occlusions of the brachial artery noted in other cases that required only a forearm fasciotomy. Bekmez et al. describe another case of a newborn born at 37 weeks, in which the axillary artery was spontaneously occluded [15]. Doppler ultrasound demonstrated thrombosis of the axillary artery which was subsequently treated with thrombolytic agents. After 24 h, the finger, hand, and forearm compartments became edematous and tight. Volar forearm and hand compartment fasciotomies were performed, and soon after, perfusion of the tissues improved significantly. Six months later, the patient had no neurological or vascular impairment. In addition to the location of injury, the duration of ischemia is a major contributing factor for the development of compartment syndrome. The time from reduction in the emergency department to fasciotomy in this patient was >13 h. The prolonged ischemia in the extremity likely contributed to the subsequent complications and need for recurrent incision and drainage. There is existing evidence regarding the increased risk of complications following acute limb ischemia within the first few hours [16,17]. Ben Hammamia et al. found a significant risk of neurological sequelae with revascularization delays >12 h for acute upper-limb ischemia [16]. Another study by Rothenberg et al. demonstrated that delays to prophylactic fasciotomy >6 h result in a significantly increased risk of amputation at the 30-day mark [17]. Although this patient recovered uneventfully after fasciotomy, there is clear evidence that prolonged limb ischemia puts patients at risk for preventable complications and further procedures. While reduction of anterior shoulder dislocations seldom results in vascular compromise, this case shows the necessity for post-reduction vascular examination as well as prompt diagnosis and treatment of upper extremity compartment syndrome. Practitioners should be mindful of the potential post-reduction complications with prompt consultation of vascular and orthopedic surgery services should this rare complication be encountered.
In a prospective study by Dragas et al. dealing with cases of traumatic arterial damage of the upper extremity, the brachial artery was the artery damaged in 55% of cases, followed by the axillary artery in 21.7% [8]. There were 9.6% of patients who demonstrated impending or established compartment syndrome and were treated with fasciotomy. In our case, the axillary artery was occluded due to contusion, secondary to an anterior shoulder dislocation. Similar axillary artery injury following closed reduction of an anterior shoulder dislocation was described in a 2018 case report by Magister et al. [14] Just as in our case, during attempts at closed reduction, the patient became apneic, was intubated, and transferred to the nearest level I trauma center. Upon transfer, distal pulses were still present while CT angiography demonstrated an axillary artery occlusion. Vascular surgeons performed a common carotid artery to mid-brachial artery bypass allograft and orthopedic surgeons performed prophylactic arm and forearm fasciotomies and carpal tunnel release due to swelling noted more distally in the hand. In our case, the forearm and the upper arm compartments were treated with fasciotomy with satisfactory outcome upon discharge. This multicompartmental compartment syndrome is likely an effect of the location of the injury on the axillary artery, as it is more proximal to the occlusions of the brachial artery noted in other cases that required only a forearm fasciotomy. Bekmez et al. describe another case of a newborn born at 37 weeks, in which the axillary artery was spontaneously occluded [15]. Doppler ultrasound demonstrated thrombosis of the axillary artery which was subsequently treated with thrombolytic agents. After 24 h, the finger, hand, and forearm compartments became edematous and tight. Volar forearm and hand compartment fasciotomies were performed, and soon after, perfusion of the tissues improved significantly. Six months later, the patient had no neurological or vascular impairment. In addition to the location of injury, the duration of ischemia is a major contributing factor for the development of compartment syndrome. The time from reduction in the emergency department to fasciotomy in this patient was >13 h. The prolonged ischemia in the extremity likely contributed to the subsequent complications and need for recurrent incision and drainage. There is existing evidence regarding the increased risk of complications following acute limb ischemia within the first few hours [16,17]. Ben Hammamia et al. found a significant risk of neurological sequelae with revascularization delays >12 h for acute upper-limb ischemia [16]. Another study by Rothenberg et al. demonstrated that delays to prophylactic fasciotomy >6 h result in a significantly increased risk of amputation at the 30-day mark [17]. Although this patient recovered uneventfully after fasciotomy, there is clear evidence that prolonged limb ischemia puts patients at risk for preventable complications and further procedures. While reduction of anterior shoulder dislocations seldom results in vascular compromise, this case shows the necessity for post-reduction vascular examination as well as prompt diagnosis and treatment of upper extremity compartment syndrome. Practitioners should be mindful of the potential post-reduction complications with prompt consultation of vascular and orthopedic surgery services should this rare complication be encountered.
Compartment syndrome has many etiologies. It can occur after prolonged ischemia in the setting of attempted shoulder reduction with vascular compromise and delayed revascularization. A fasciotomy should be considered when there is a high index of suspicion of a reperfusion injury in the upper extremity.
Compartment syndrome must be considered in the case of prolonged vascular compromise after shoulder reduction.
References
- 1.McNally MM, Univers J. Acute limb ischemia. Surg Clin North Am 2018;98:1081-96. [Google Scholar | PubMed]
- 2.Wesslen C, Wahlgren CM. Contemporary management and outcome after lower extremity fasciotomy in non-trauma-related vascular surgery. Vasc Endovascular Surg 2018;52:493-7. [Google Scholar | PubMed]
- 3.Kronja G, Misovic S, Tomic A. Indications and results of fasciotomy in vascular injuries of the lower extremities. Vojnosanit Pregl 2000;57:271-6. [Google Scholar | PubMed]
- 4.Hofmeister EP, Shin AY. The role of prophylactic fasciotomy and medical treatment in limb ischemia and revascularization. Hand Clin 1998;14:457-65, x. [Google Scholar | PubMed]
- 5.Sayar U, Ozer T, Mataraci I. Forearm compartment syndrome caused by reperfusion injury. Case Rep Vasc Med 2014;2014:931410. [Google Scholar | PubMed]
- 6.Zellweger R, Hess F, Nicol A, Omoshoro-Jones J, Kahn D, Navsaria P. An analysis of 124 surgically managed brachial artery injuries. Am J Surg 2004;188:240-5. [Google Scholar | PubMed]
- 7.Ekim H, Tuncer M. Management of traumatic brachial artery injuries: A report on 49 patients. Ann Saudi Med 2009;29:105-9. [Google Scholar | PubMed]
- 8.Dragas M, Davidovic L, Kostic D, Markovic M, Pejkic S, Ille T, et al. Upper extremity arterial injuries: Factors influencing treatment outcome. Injury 2009;40:815-9. [Google Scholar | PubMed]
- 9.Pillai L, Luchette FA, Romano KS, Ricotta JJ. Upper-extremity arterial injury. Am Surg 1997;63:224-7. [Google Scholar | PubMed]
- 10.Andreev A, Kavrakov T, Karakolev J, Penkov P. Management of acute arterial trauma of the upper extremity. Eur J Vasc Surg 1992;6:593-8. [Google Scholar | PubMed]
- 11.Tan TW, Joglar FL, Hamburg NM, Eberhardt RT, Shaw PM, Rybin D, et al. Limb outcome and mortality in lower and upper extremity arterial injury: A comparison using the National Trauma Data Bank. Vasc Endovascular Surg 2011;45:592-7. [Google Scholar | PubMed]
- 12.Myers SI, Harward TR, Maher DP, Melissinos EG, Lowry PA. Complex upper extremity vascular trauma in an urban population. J Vasc Surg 1990;12:305-9. [Google Scholar | PubMed]
- 13.Kim JY, Buck DW 2nd, Forte AJ, Subramanian VS, Birman MV, Schierle CF, et al. Risk factors for compartment syndrome in traumatic brachial artery injuries: An institutional experience in 139 patients. J Trauma 2009;67:1339-44. [Google Scholar | PubMed]
- 14.Magister S, Bridgforth A, Yarboro S. Axillary artery injury following closed reduction of an age-indeterminate anterior glenohumeral dislocation. J Orthop Case Rep 2018;8:53-6. [Google Scholar | PubMed]
- 15.Bekmez S, Beken S, Mermerkaya MU, Ozkan M, Okumus N. Acute forearm compartment syndrome in a newborn caused by reperfusion after spontaneous axillary artery thrombosis. J Pediatr Orthop B 2015;24:552-5. [Google Scholar | PubMed]
- 16.Ben Hammamia M, Ben Mrad M, Mleyhi S, Ziadi J, Ghedira F, Ben Omrane S, et al. Revascularization delay and complications in acute upper limb ischemia. J Med Vasc 2019;44:194-8. [Google Scholar | PubMed]
- 17.Rothenberg KA, George EL, Trickey AW, Chandra V, Stern JR. Delayed fasciotomy is associated with higher risk of major amputation in patients with acute limb ischemia. Ann Vasc Surg 2019;59:195-201. [Google Scholar | PubMed]