Dematiaceous fungi are a very rare cause of olecranon bursitis and a high index of suspicion is required for its diagnosis and timely management.
Dr. Sandeep Mohan, Department of Orthopaedics, St Joseph Hospital, Kannur, Kerala, India. E-mail: sandeepmohan123@gmail.com
Introduction: Dematiaceous fungi are a group of fungi characterized by the presence of melanin in their cell walls. These fungi are known to cause a wide range of infections in humans, including skin and soft-tissue infections, sinusitis, and meningitis. Infections caused by dematiaceous fungi are typically seen in immunocompromised hosts and manifest most commonly as cutaneous or subcutaneous disease. Systemic infections are exceedingly rare and associated with significant morbidity and mortality.
Case Report: Here is a case study of a 75-year-old diabetic male with a rare case of dematiaceous fungal infection in the olecranon bursa. The patient presented with a painless swelling of 3-year duration over the right elbow which started draining pus for 1 month. Surgical excision of the bursa was performed, and histopathological examination and culture confirmed the diagnosis of dematiaceous fungal infection. We discuss the diagnosis, treatment, and management of this rare fungal infection.
Conclusion: Although dematiaceous fungal infections are a rare cause of olecranon bursitis, the clinician must send a fungal culture in every case for prompt diagnosis and treatment.
Keywords: Dematiaceous fungi, olecranon bursitis, Exophiala, diabetes, immune compromised.
Dematiaceous fungi are ubiquitous saprophytic filamentous molds characterized by dark structures due to melanin deposition in their cell wall [1]. The 3 clinical syndromes resulting from dematiaceous fungal infection of the skin are eumycetoma, chromoblastomycosis, and phaeohyphomycosis [1]. Dematiaceous fungal infections of the olecranon bursa are extremely rare. Here, we present a case study of a 75-year-old diabetic male with a dematiaceous fungal infection in the olecranon bursa.
A 75-year-old male with a history of type 2 diabetes and treatment completed tuberculosis presented in outpatient department for evaluation of right olecranon bursitis. The patient has had a painless swelling over his right elbow for 3 years with no associated history of trauma. Swelling started to drain purulent pus for the past 1 month which was when the patient had sought medical attention. The patient was then treated with multiple antibiotics but with no relief. On examination, the patient had an enlarged, thickened, and fluctuant right olecranon bursa of 5 cm diameter with copious purulent pus drainage. There was no overlying cellulitis or lymphadenopathy. Range of movements of right elbow was full and painless. Radiographic evaluation showed a soft-tissue swelling over the olecranon without any osseous involvement or joint space reduction. Blood leukocyte count was within limits. A bacterial culture was sent which came back negative. Surgical excision of the bursa was performed under brachial plexus block. Intraoperative examination revealed a thick-walled bursa filled with purulent material. The bursa was excised and sent for histopathological examination (Fig. 1 and 2).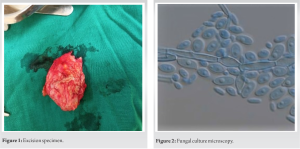 Histopathological analysis revealed the phaeohyphomycosis associated granulomatous inflammatory lesion with the presence of dematiaceous fungi, identified as Exophiala spp. on culture (Fig. 3, 4, 5). Since there was a significant clinical improvement by the time the histopathology and fungal culture report arrived, the patient was not started on antifungals. Serial reviews were done and no recurrence was observed.
Histopathological analysis revealed the phaeohyphomycosis associated granulomatous inflammatory lesion with the presence of dematiaceous fungi, identified as Exophiala spp. on culture (Fig. 3, 4, 5). Since there was a significant clinical improvement by the time the histopathology and fungal culture report arrived, the patient was not started on antifungals. Serial reviews were done and no recurrence was observed.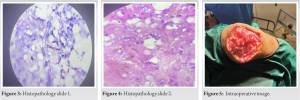
The dematiaceous (brown-pigmented) fungi are a large and heterogenous group of molds that cause a wide range of diseases including phaeohyphomycosis, chromoblastomycosis, and eumycotic mycetoma. Among the more important human pathogens are Alternaria species, Bipolaris species, Cladophialophora bantiana, Curvularia species, Exophiala species, Fonsecaea pedrosoi, Madurella species, Phialophora species, Scedosporium prolificans, Scytalidium dimidiatum, and Wangiella dermatitidis. These organisms are widespread in the environment, being found in soil, wood, and decomposing plant debris. Cutaneous, subcutaneous, and corneal infections with dematiaceous fungi occur worldwide but are more common in tropical and subtropical climates. Infection results from traumatic implantation. Most cases occur in immunocompetent individuals. Dematiaceous molds are also important causes of invasive sinusitis and allergic fungal sinusitis. Infection is thought to follow inhalation. Although cerebral infection is the most common form of systemic phaeohyphomycosis, other localized deep forms of the disease, such as arthritis and endocarditis, have been reported [2]. The majority of cases of septic bursitis are due to bacterial pathogens, particularly Gram-positive organisms (Staphylococcus aureus and Streptococcal species). More recently, reports have appeared in the literature of chronic infectious bursitis caused by fungi and occurring in both immunocompromised and healthy immunocompetent individuals [3,4]. Although the prevalence of bursitis, in total, was equal in olecranon as well as patellar bursa, fungal bursitis was found to be more prevalent in the olecranon bursa [5]. This was mentioned in one study [6,7] that due to its superficial location, swelling of the olecranon bursa is easy to detect by both the patient and the examiner. Other less common sites of involvement in fungal bursitis were patella and ankle (retrocalcaneal). Direct inoculation of deep bursa is uncommon, but iatrogenic infection resulting from bursal injections of glucocorticoids (e.g., subacromial, iliopsoas, or trochanteric bursae) may rarely occur [8]. In the absence of a known inoculation, infection of deep bursae is presumed to be due to hematogenous seeding or spread from an adjacent septic site such as contiguous septic arthritis [9]. Most reports of curative therapy describe the use of surgical debridement and long-term antifungal medication and illustrate the difficulty in treating these types of fungal infections. Long-term therapy that is interrupted or prematurely terminated raises the concern for developing antifungal resistance [10]. In our case, the patient had a rare dematiaceous fungal infection in the olecranon bursa. Surgical excision of the infected bursa is the treatment of choice for olecranon bursitis and is generally curative. In most cases, antifungal therapy may be necessary to prevent recurrence.
Dematiaceous fungal infections are a rare but important cause of infections in humans. In our case, we report a rare case of dematiaceous fungal infection in the olecranon bursa of a diabetic male. Timely diagnosis and appropriate treatment with surgical excision of the infected bursa led to a full recovery of the patient.
Due to rarity of the dematiaceous fungal cause of olecranon bursitis, we have to keep a high index of suspicion in all cases of olecranon bursitis, especially in immune compromised individuals and a fungal culture must be performed in all and every case.
References
- 1.Sutton DA, Rinaldi MG, Sanche SE. Dematacious fungi. In: Anaissie EJ, McGinnis MR, Pfaller MA, editors. Clinical Mycology. 2nd ed. Edinburgh, Scotland: Churchill Livingstone; 2009. p. 329-354. [Google Scholar | PubMed]
- 2.Brandt ME, Warnock DW. Epidemiology, clinical manifestations, and therapy of infections caused by dematiaceous fungi. J Chemother 2003;15 Suppl 2:36-47. [Google Scholar | PubMed]
- 3.Gertner E. Chronic septic bursitis caused by dematiaceous fungi. Am J Orthop (Belle Mead NJ) 2007;36:E10-1. [Google Scholar | PubMed]
- 4.Rakita U, Wallis LS, Grushchak S, Veselinovic M, Liu W, Krunic AL. Phaeohyphomycotic pseudotumor of the right elbow caused by Trematosphaeria grisea. JAAD Case Rep 2021;13:1-4. [Google Scholar | PubMed]
- 5.Kannadas S, Nisha TR. Clinicopathological study of fungal bursitis. J Evolution Med Dent Sci 2017;6:3629-2. [Google Scholar | PubMed]
- 6.Enzenauer RJ, Pluss JL. Septic olecranon bursitis in patients with chronic obstructive pulmonary disease. Am J Med 1996;100:479-80. [Google Scholar | PubMed]
- 7.Rubayi S, Montgomerie JZ. Septic ischial bursitis in patients with spinal cord injury. Paraplegia 1992;30:200-3. [Google Scholar | PubMed]
- 8.Drezner JA, Sennett BJ. Subacromial/subdeltoid septic bursitis associated with isotretinoin therapy and corticosteroid injection. J Am Board Fam Pract 2004;17:299-302. [Google Scholar | PubMed]
- 9.Small LN, Ross JJ. Suppurative tenosynovitis and septic bursitis. Infect Dis Clin North Am 2005;19:991-1005, xi. [Google Scholar | PubMed]
- 10.Bossler AD, Richter SS, Chavez AJ, Vogelgesang SA, Sutton DA, Grooters AM, et al. Exophiala oligosperma causing olecranon bursitis. J Clin Microbiol 2003;41:4779-82. [Google Scholar | PubMed]