Early diagnosis and intervention for gluteal compartment syndrome in the setting of acute pelvic trauma is critically important due to its potential for severe consequences, including death if left untreated
Dr. Jared B Hinton, Northeast Ohio Medical University, Ohio, USA. E-mail: jhinton@neomed.edu
Introduction: Compartment syndrome, an exceptionally rare condition, is a surgical emergency that can quickly escalate to limb ischemia and necrosis without treatment. Most cases occur post-trauma, typically affecting the anterior compartment of the leg. Patients present with pain out of proportion to their physical examination findings and often have an early hallmark discovery of pain with passive extension. Compartment syndrome of the buttock requires an even higher index of suspicion, as the condition is even more uncommon, and the diagnosis is complicated by it being difficult to palpate the affected area and passively extend the leg when the patient is supine.
Case Report: This case report presents an 83-year-old female with compartment syndrome of the left gluteal region, status post-fall 1 day earlier. She was admitted to the medical team for observation and failed to respond to narcotic pain medication. The physical examination revealed firm, tense, left gluteal compartments with buttock hematoma and surrounding muscle induration, significant pain, and extremity weakness in the sciatic nerve distribution. An emergent fasciotomy was performed to decompress the affected compartments.
Conclusion: All physicians must be mindful of gluteal compartment syndrome in patients complaining of buttock pain, especially after pelvic trauma, who present with buttock swelling, tense gluteal compartments, and severe gluteal pain. A delay in diagnosis or treatment can lead to severe consequences, including disability, irreversible gluteal muscle damage, sciatic nerve dysfunction, kidney failure, or death.
Keywords: Compartment syndrome, gluteal region, acute pelvic trauma.
Compartment syndrome is a medical emergency caused by increased intercompartmental pressures from extensive microvasculature damage within non-expandable musculoskeletal compartments. It is a surgical emergency that requires early intervention to prevent necrosis of the soft tissues, permanent disability, or death [1]. One study reported mortality rates as high as 47% following instances of acute compartment syndrome (ACS) in the thigh [2]. Typically, ACS occurs following fractures or crush injuries to the leg or forearm [3,4]. ACS is a rare condition with an incidence rate of 7.3/100,000 males and 0.7/100,000 females [3]. Compartment syndrome of the gluteal region is particularly rare and is classically associated with prolonged immobilization [5]. This case report presents an unusual instance involving an 83-year-old female who developed compartment syndrome in the left gluteal region following a fall. The report highlights the importance of recognizing gluteal compartment syndrome as a potential consequence of acute pelvic trauma and the critical need for the early diagnosis and intervention to prevent severe complications.
An 83-year-old Caucasian female with no history of bleeding disorders but with a history of eliquis use (5 mg 2× per day) and pertinent medical conditions including acute diastolic heart failure, hypertension, sideroblastic anemia, and paroxysmal atrial fibrillation, presented with left hip pain and a large, expanding hematoma after sustaining a fall the day prior. The patient was admitted to the medical team and given pain medication; however, she did not show any improvement over the next 24 h. Therefore, the orthopedics department was consulted, leading to the diagnosis of gluteal compartment syndrome. The operating room team was immediately notified, and the patient underwent emergent fasciotomy. The patient stated that her pain was a 10 on a scale of 1–10, with notable weakness and increased pain in the leg on passive extension when the nurses would roll her. The patient had to be rolled onto her non-affected side for the physical examination. The patient had a large hematoma on her left gluteal region with tense gluteal compartments, surrounding muscle induration, and pain out of proportion for the narcotics received. Most significantly, the patient exhibited weakness of dorsiflexion and plantarflexion of the ankle with numbness in the sciatic nerve distribution. The patient’s left buttock was approximately 3 times the size of her right. Computed tomography scan confirmed an enlarged expanding hematoma, 8 × 8 cm, and showed surrounding muscle hemorrhage and edema (Fig. 1). The patient’s hemoglobin was 7.6 g/dL. The clinical diagnosis was compartment syndrome of the left gluteal region and subsequent sciatic neuropraxia.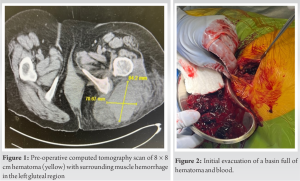
The patient underwent an emergent fasciotomy of the three gluteal compartments with evacuation of the hematoma at the time of surgery. Kcentra was given to reverse the effects of her eliquis before surgery. The muscle fibers of the gluteus maximus were dark and devoid of blood supply, consistent with necrosis, which underwent debridement. Several basins of hematoma and blood were evacuated (Fig. 2).A drain was not placed, as there was concern for further damage to the sciatic nerve if the patient was to lay supine on the drain. Postoperatively, the wound healed by secondary intention with no signs of infection. The patient had a return of sciatic nerve function and returned to her normal, active level of function 3 months post-operative. 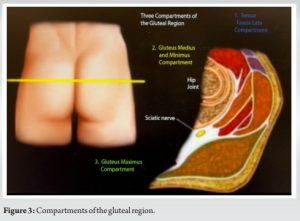
Compartment syndrome is considered a surgical emergency, and the importance of early diagnosis and treatment cannot be overstated. Compartment syndrome results from microvascular changes that increase interstitial pressures within non-expandable musculoskeletal compartments, compressing the associated vasculature and neurovasculature. Eventually, this compression results in ischemia, cellular hypoxia, and tissue death. 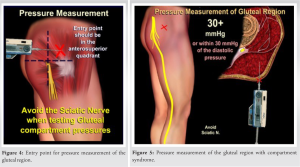 Irreversible rhabdomyolysis can manifest in as little as a few hours, while neurovasculature can be compromised in just 33 min [6]. Therefore, the management of compartment syndrome relies on early identification and treatment. In this case, the operating room team was promptly alerted when compartment syndrome was suspected, avoiding any delay in treatment after the patient presented with the left hip pain secondary to a large, firm intramuscular hematoma with progressive expansion, and extreme pain on passive extension. Trauma is the primary cause of compartment syndrome in various body regions, but gluteal compartment syndrome typically arises from extended periods of immobilization. Recent literature links gluteal compartment syndrome to substance abuse or incorrect surgical positioning, resulting in prolonged immobilization [3]. However, ACS of the gluteal region precipitated by trauma is not as well reported. In addition, a few cases of compartment syndrome have followed chronic anticoagulant use. Spontaneous muscle hematomas can be a serious complication of anticoagulant treatment [7]. Anticoagulant use can also exacerbate bleeding in the setting of minor traumas. The incidence of anticoagulant-associated bleeding has increased with the growing number of patients receiving these drugs. In this particular case, the patient was on eliquis (5 mg 2× per day) for the management of her paroxysmal atrial fibrillation and had a chronic history of sideroblastic anemia. She had been under the care of hematology specialists for several years. She underwent a comprehensive hematological evaluation, which revealed normal results for prothrombin time (PT), partial thromboplastin time (PTT), international normalized ratio (INR), and platelet count at the time of her admission. Therefore, aside from the traumatic injury, there were no other underlying causes identified for the patient’s bleeding issues.
Irreversible rhabdomyolysis can manifest in as little as a few hours, while neurovasculature can be compromised in just 33 min [6]. Therefore, the management of compartment syndrome relies on early identification and treatment. In this case, the operating room team was promptly alerted when compartment syndrome was suspected, avoiding any delay in treatment after the patient presented with the left hip pain secondary to a large, firm intramuscular hematoma with progressive expansion, and extreme pain on passive extension. Trauma is the primary cause of compartment syndrome in various body regions, but gluteal compartment syndrome typically arises from extended periods of immobilization. Recent literature links gluteal compartment syndrome to substance abuse or incorrect surgical positioning, resulting in prolonged immobilization [3]. However, ACS of the gluteal region precipitated by trauma is not as well reported. In addition, a few cases of compartment syndrome have followed chronic anticoagulant use. Spontaneous muscle hematomas can be a serious complication of anticoagulant treatment [7]. Anticoagulant use can also exacerbate bleeding in the setting of minor traumas. The incidence of anticoagulant-associated bleeding has increased with the growing number of patients receiving these drugs. In this particular case, the patient was on eliquis (5 mg 2× per day) for the management of her paroxysmal atrial fibrillation and had a chronic history of sideroblastic anemia. She had been under the care of hematology specialists for several years. She underwent a comprehensive hematological evaluation, which revealed normal results for prothrombin time (PT), partial thromboplastin time (PTT), international normalized ratio (INR), and platelet count at the time of her admission. Therefore, aside from the traumatic injury, there were no other underlying causes identified for the patient’s bleeding issues.
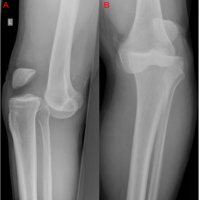
The gluteal region contains three compartments: the tensor fascia lata, the gluteus medius and minimus, and the gluteus maximus (Fig. 3) [8]. Each is enclosed by gluteal fascia, limiting their space, and predisposing them to high pressures if microvasculature is compromised [6,9]. When measuring pressure in the gluteal region, the sciatic nerve should be avoided by obtaining pressure readings from the superior anterior quadrant of the buttock (Fig. 4) [8]. In each compartment, the pressure should be <10 mmHg. Pressures above 30 mmHg or within 30 mmHg of diastolic pressure are considered diagnostic of compartment syndrome; however, it is essential not to rule out compartment syndrome or delay treatment based on a single normal pressure value (Fig. 5) [8]. If compartment syndrome is suspected, surgical intervention should be performed without hesitation [3,8,10]. Early treatment with fasciotomy improves the chances of preserved muscle function and full recovery. In advanced stages of gluteal compartment syndrome, neurovasculature and musculature are particularly susceptible to ischemic changes. The sciatic nerve’s location between the gluteus maximus and the external rotator complex makes it vulnerable to gluteal swelling, leading to compression-induced neuropathy [6,10]. In addition to neuropathy, gluteal compartment syndrome can result in severe rhabdomyolysis, characterized by systemic manifestations of muscle tissue necrosis. Rhabdomyolysis exhibits elevated creatinine, urea, potassium, and myoglobin levels in the urine [6]. Without aggressive intervention, organ dysfunction, acute kidney injury, and even death can ensue [11].
This case report highlights the importance of early diagnosis and treatment of gluteal compartment syndrome. This rare surgical emergency can lead to severe consequences, including disability, irreversible muscle damage, sciatic nerve dysfunction, kidney failure, or even death if left untreated. The presented case involving an 83-year-old female patient post-fall is a reminder of the need for vigilance in recognizing the potential for gluteal compartment syndrome, particularly in patients with acute pelvic trauma presenting with characteristic symptoms. Early fasciotomy is the key to successful management to relieve pressure, preserve muscle, and improve patient outcomes.
This article underscores the critical importance of early diagnosis and intervention in cases of gluteal compartment syndrome following acute pelvic trauma, as delayed treatment can lead to severe consequences, including death, highlighting the need for heightened clinical awareness in such scenarios.
References
- 1.Via AG, Oliva F, Spoliti M, Maffulli N. Acute compartment syndrome. Muscles Ligaments Tendons J 2015;5:18-22. [Google Scholar | PubMed]
- 2.Schwartz JT Jr., Brumback RJ, Lakatos R, Poka A, Bathon GH, Burgess AR. Acute compartment syndrome of the thigh-a spectrum of injury. J Bone Joint Surg Am 1989;71:392-400. [Google Scholar | PubMed]
- 3.Torlincasi AM, Lopez RA, Waseem M. Acute compartment syndrome. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. [Google Scholar | PubMed]
- 4.Elsorafy KR, Jm Stone A, Nicol SG. Acute compartment syndrome of the thigh 10 days following an elective primary total hip replacement. Ortop Traumatol Rehabil 2013;5:269-71. [Google Scholar | PubMed]
- 5.Villalba J, Solernou X. Gluteal compartment syndrome after total hip replacement. A presentation of two cases. Rev Esp Cir Ortop Traumatol 2013;57:296-9. [Google Scholar | PubMed]
- 6.Diaz Dilernia F, Zaidenberg EE, Gamsie S, Taype Zamboni DE, Carabelli GS, Barla JD, et al. Gluteal compartment syndrome secondary to pelvic trauma. Case Rep Orthop 2016;2016:2780295. [Google Scholar | PubMed]
- 7.Dohan A, Darnige L, Sapoval M, Pellerin O. Spontaneous soft tissue hematomas. Diagn Interv Imaging 2015;96:789-96. [Google Scholar | PubMed]
- 8.Abdelgawad A, Ebraheim N. Compartment Syndrome: Everything You Need to Know about Compartment Syndrome of the Upper and Lower Extremities; 2023. [Google Scholar | PubMed]
- 9.Iizuka S, Miura N, Fukushima T, Seki T, Sugimoto K, Inokuchi S. Gluteal compartment syndrome due to prolonged immobilization after alcohol intoxication: A case report. Tokai J Exp Clin Med 2011;36:25-8. [Google Scholar | PubMed]
- 10.Liu HL, Wong DS. Gluteal compartment syndrome after prolonged immobilisation. Asian J Surg 2009;32:123-6. [Google Scholar | PubMed]
- 11.Asmara IG, Pebruanto H, Winatha IM. Rhabdomyolysis with compartment syndrome-induced acute kidney injury in resource-limited settings: A case report. Caspian J Intern Med 2022;13:810-4. [Google Scholar | PubMed]