This case series underscores the importance of including primary hyperparathyroidism in the differential diagnosis of multiple osteolytic bone lesions to prevent unnecessary surgical interventions.
Dr. Nagashree Vasudeva, Department of Orthopaedics and Trauma, Ganga Medical Centre and Hospitals Private Limited, 313, Mettupalayam Road, Coimbatore, Tamil Nadu, India. E-mail: drnagashreev@gmail.com
Introduction: Primary hyperparathyroidism (PHPT) is an intrinsic abnormality of the parathyroid glands in which there is an inappropriate secretion of parathormone (PTH), resulting in skeletal resorption and bone loss. The characteristic bony changes of fibrotic cystic lesions are called Brown’s tumors. Clinical dilemmas exist due to the varied clinical presentation of hypercalcemia with multiple lytic lesions mimicking metastatic bone disease. 99 mTc sestamibi scanning is the imaging modality of choice used for the preoperative localization of parathyroid adenomas. Surgery provides a definitive treatment, and the bony lesions resolve completely over a period of time.
Case Report: We present four cases of PHPT where they presented with multiple lytic lesions and were evaluated for metastatic deposits. The diagnosis was confirmed with a biopsy. They were successfully treated by excision of the parathyroid gland. A high index of suspicion will avoid misdiagnosis and inappropriate treatment.
Conclusion: PHPT must be considered as a differential diagnosis for multiple osteolytic bone lesions. Diagnosis can be aided by a thorough clinical examination, including an assessment for neck swelling and laboratory testing of serum calcium levels and PTH levels. Surgical excision of the hyperactive gland serves as the definitive treatment for this condition, with bony lesions regressing gradually over time.
Keywords: Brown tumors, bone scan, hyperparathyroidism, primary, osteitis fibrosa cystica.
Primary hyperparathyroidism (PHPT) is a condition characterized by excessive secretion of parathyroid hormone (PTH), resulting in excessive bone resorption due to increased osteoclastic activity. This leads to multiple lytic lesions in the skeletal system, and a microscopic examination of these would reveal circumscribed brown-colored areas of bony resorption, typically referred to as “brown tumors” [1]. Skeletal manifestations of hyperparathyroidism occur in <2% of patients. Such multiple lytic lesions often look similar to secondary metastatic deposits in bone and pose a real challenge for the clinician in the differential diagnosis. However, they are benign and often regress spontaneously after treating the primary cause. We present four such cases that presented with multiple lytic lesions and were thought to be secondary metastases. The management and the outcomes have been discussed here.
Case 1
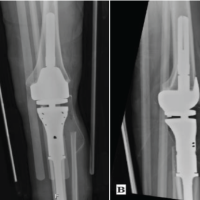
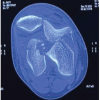
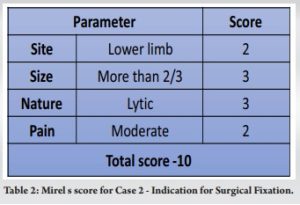
A 53-year-old female presented to the orthopedic outpatient with pain over both hips and difficulty walking for the past 1 month. The pain was dull and aching, aggravated by activity, relieved by rest, associated with backache, and had a history of significant weight loss. On physical examination of the patient, she had tenderness over the left trochanter and low back. A swelling of 4×3 cm was noticed in the anterior aspect of the neck, which moves with deglutition. On laboratory analysis, serum calcium level was 15.2 mg/dL (normal 8.4–10.7 mg/dL), serum albumin level was 4.3 g/dL (normal 3.4–4.8 g/dL), serum PTH level was 2233 pg/mL (normal 7–53 pg/mL), and vitamin D3 was 32 pg/mL (normal 25–45 pg/mL). Radiological evaluation of the pelvis revealed multiple lytic expansile lesions involving the pelvis (left ischial tuberosity, bilateral iliac bone, and both iliac crests), neck and intertrochanteric region of the left femur, head of the right femur, and right pedicle of T11 and L3. There was a cortical breach with significant thickening of the cortex noted involving the left femoral neck. Further evaluation of the chest and abdomen showed multiple enhanced, well-defined lytic expansile lesions involving the left glenoid and posterior aspects of the right 9th and 12th ribs. The radiograph of the skull was found to be normal. An ultrasound scan of the neck showed a well-defined homogenous hypoechoic solid soft tissue lesion in relation to the posterior aspect of the inferior pole of the left lobe of the thyroid, and a bone scan provided enhanced activity at the same site. A Tc99 scan was done, which showed enhanced activity in the parathyroid gland.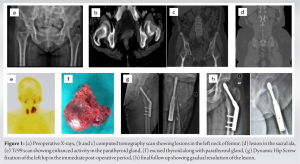 To arrive at a conclusive diagnosis, pathological analysis of the thyroid and bony lesion was essential. After a mandatory indirect laryngoscope to visualize the vocal cords, the patient underwent a left hemithyroidectomy and a left-sided parathyroidectomy, along with an intraoperative assessment of PTH (half-life of 5 min), where it had decreased from the pre-operative levels of 1869 pg/mL to 228 pg/mL, and hence, a complete excision of the adenoma was confirmed. Pathological analysis revealed the presence of hypercellular nodules with chief cell hyperplasia, surrounded by a capsule, which confirmed the diagnosis of a brown tumor. Since Mirel’s score was 9 (Table 2), it was followed by internal fixation of the left neck of the femur with a dynamic hip screw, after which the patient was able to ambulate with walking frame support. The patient was closely monitored for serial serum calcium levels in the post-operative period and was treated appropriately. Two weeks postoperatively, the serum levels of calcium and PTH had declined to a level within their respective normal limits. The follow-up visits were unremarkable, and by the end of 6 months the lesion had completely resolved, and the patient was able to walk without support along with resuming her normal activities.
To arrive at a conclusive diagnosis, pathological analysis of the thyroid and bony lesion was essential. After a mandatory indirect laryngoscope to visualize the vocal cords, the patient underwent a left hemithyroidectomy and a left-sided parathyroidectomy, along with an intraoperative assessment of PTH (half-life of 5 min), where it had decreased from the pre-operative levels of 1869 pg/mL to 228 pg/mL, and hence, a complete excision of the adenoma was confirmed. Pathological analysis revealed the presence of hypercellular nodules with chief cell hyperplasia, surrounded by a capsule, which confirmed the diagnosis of a brown tumor. Since Mirel’s score was 9 (Table 2), it was followed by internal fixation of the left neck of the femur with a dynamic hip screw, after which the patient was able to ambulate with walking frame support. The patient was closely monitored for serial serum calcium levels in the post-operative period and was treated appropriately. Two weeks postoperatively, the serum levels of calcium and PTH had declined to a level within their respective normal limits. The follow-up visits were unremarkable, and by the end of 6 months the lesion had completely resolved, and the patient was able to walk without support along with resuming her normal activities.
Case 2
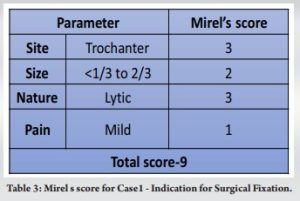
An 80-year-old female presented with a history of gradually increasing swelling in the left leg for the past 2 months and insidious onset pain of 1 week duration. There was no significant history of trauma. On examination, there was minimal tenderness over the middle third of the anterior aspect of the leg. Blood investigations showed an increased serum calcium level of 14 mg/dL (normal 8.4–10.7 mg/dL), a serum albumin level of 4.3 g/dL (normal 3.4–4.8 g/dL), a serum PTH level of 1380 pg/mL (normal 7–53 pg/mL), and a vitamin D3 level of 28 pg/mL (normal 25–45 pg/mL). Radiological examination showed multiple lytic areas of destruction in the entire length of the left tibia, distal femur, and tarsal bones. A nuclear scan revealed enhanced activity in the right parathyroid gland, and a diagnosis of PHPT was made. She underwent a biopsy of the bony lesion, which was followed by a hemithyroidectomy. A prophylactic nailing of the left tibia was done since the scoring as per Mirel’s criteria was 10 (Table 3).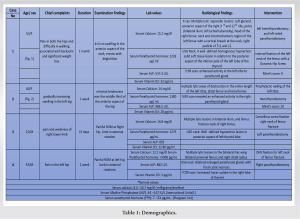 Histopathological findings were consistent with Brown’s tumor. Serial calcium monitoring was done to monitor for hypocalcemic episodes and was treated with intravenous calcium therapy. The post-operative care included static quadriceps exercises and was initiated along with walking frame-assisted non-weight-bearing mobilization. After 6 weeks, blood parameters were repeated and were found to be normal. The patient was kept non-weight-bearing for 12 weeks, followed by gradual partial-weight-bearing with walker assistance. She was asymptomatic at 6 months of follow-up with near-normal serum parameters and was permitted to walk with a stick support. At 1 year, the fracture healed completely, and she was painless. The case details of the demographics, clinical presentation, laboratory and radiological signs, and treatment given to each of the 4 patients are summarized in Table 1.
Histopathological findings were consistent with Brown’s tumor. Serial calcium monitoring was done to monitor for hypocalcemic episodes and was treated with intravenous calcium therapy. The post-operative care included static quadriceps exercises and was initiated along with walking frame-assisted non-weight-bearing mobilization. After 6 weeks, blood parameters were repeated and were found to be normal. The patient was kept non-weight-bearing for 12 weeks, followed by gradual partial-weight-bearing with walker assistance. She was asymptomatic at 6 months of follow-up with near-normal serum parameters and was permitted to walk with a stick support. At 1 year, the fracture healed completely, and she was painless. The case details of the demographics, clinical presentation, laboratory and radiological signs, and treatment given to each of the 4 patients are summarized in Table 1.
PHPT is characterized by the hyperactivity of parathyroid glands, often due to a solitary benign adenoma (80–85%) [1]. The bony manifestations of this condition are called “brown tumors,” although the word tumor is a misnomer. These bony lesions manifest in approximately only 2% of the PHPT patients [2]. They represent a terminal stage of hyperparathyroidism-dependent bone pathology. The classical bony manifestation of PHPT is osteitis fibrosa cystica, which is characterized clinically by bone pain and radiographically by subperiosteal bone resorption on the radial aspect of the middle phalanges, tapering of the distal clavicles, a “salt and pepper” appearance of the skull, bone cysts, and brown tumors of the long bones. Brown tumors result from excess osteoclast activity and consist of collections of osteoclasts intermixed with fibrous tissue and poorly mineralized woven bone. The brown coloration is due to hemosiderin deposition. The clinical presentation of bone pain, multiple lytic lesions in X-rays, and hypercalcemia presents a diagnostic dilemma of the two most common conditions, i.e., metastatic tumors and hyperparathyroidism [3,4]. The definitive treatment for hyperparathyroidism is a parathyroidectomy. In the postoperative period, associated vitamin D deficiency makes the patients more prone to hungry bone disease, i.e., after a successful parathyroidectomy, patients have shown normalization of bone turnover markers and increases in bone mineral density with a gradual disappearance of the skeletal lesions over a period of time [5,6]. Bones that were barely visible due to severe osteopenia became easily appreciable. Most noticeable was a dramatic “brightening” of the brown tumors, as if they were filled up with bone minerals. Joyce et al. reported about this condition first in a middle-aged female, and since then, many cases have been reported [7]. We describe here four cases of PHPT where bone pain or fracture was the first clinical manifestation of the disease. In none of the cases, symptoms of hypercalcemia were present. In the presence of multiple large osteolytic lesions, primary or metastatic cancer is frequently considered a differential. Many a times, elevated calcium and ALP are considered manifestation of the malignancy itself [8]. Also, due to the rarity of the disease, it is not included in the radiological differential diagnosis of such skeletal lesions. To avoid misdiagnosis and unnecessary or harmful interventions, a high index of suspicion is necessary in the presence of hypercalcemia and elevated PTH levels. A 99 mTc sestamibi scan is useful to locate the adenoma and localization. The mainstay of treatment was the surgical removal of the hyperfunctioning parathyroid gland. The intervention for the bony issues was considered based on the Mirel scoring for estimating the pathologic fracture [9]. Postoperatively, the patients recovered well, and the lesions disappeared gradually [10].
This case series emphasizes the need to include PHPT as a differential diagnosis for multiple osteolytic bone lesions to avoid unnecessary surgical interventions. Surgical excision of the hyperactive gland is a definitive treatment of the condition, and the bony lesion regresses gradually over a period of time.
• The value of accurate diagnosis in cases with osteolytic lesions is emphasized in this report, where such lesions can lead to various possible diagnoses, including metastatic bone involvement, multiple myeloma, and metabolic bone diseases like hyperparathyroidism due to adenoma
• It’s important to note that these conditions require significantly different treatment approaches, ranging from chemotherapy to surgical removal of the adenoma
• We present a case series that initially appeared to resemble metastatic bone involvement but, upon careful examination, was determined to have a rather benign cause
• Therefore, it is crucial to consider brown tumors as a potential differential diagnosis for osteolytic bone lesions to avoid unnecessary interventions.
References
- 1.Grulois V, Buysschaert I, Schoenaers J, Debruyne F, Delaere P, Vander Poorten V. Brown tumour: Presenting symptom of primary hyperparathyroidism. B ENT 2005;1:191-5. [Google Scholar | PubMed]
- 2.Kaplan EL, Yashiro T, Salti G. Primary hyperparathyroidism in the 1990s: Choice of surgical procedures for this disease. Ann Surg 1992;215:300-17. [Google Scholar | PubMed]
- 3.Priya G, Jyotsna VP, Gupta N, Chumber S, Bal CS, Karak AK, et al. Clinical and laboratory profile of primary hyperparathyroidism in India. Postgrad Med J 2008;84:34-9. [Google Scholar | PubMed]
- 4.Gopal RA, Acharya SV, Bandgar T, Menon PS, Dalvi AN, Shah NS. Clinical profile of primary hyperparathyroidism from western India: A single center experience. J Postgrad Med 2010;56:79-84. [Google Scholar | PubMed]
- 5.Mishra SK, Agarwal G, Kar DK, Gupta SK, Mithal A, Rastad J. Unique clinical characteristics of primary hyperparathyroidism in India. Br J Surg 2002;88:708-14. [Google Scholar | PubMed]
- 6.Silverberg SJ, Clarke BL, Peacock M, Bandeira F, Boutroy S, Cusano NE, et al. Current issues in the presentation of asymptomatic primary hyperparathyroidism: Proceedings of the fourth international workshop. J Clin Endocrinol Metab 2014;99:3580-94. [Google Scholar | PubMed]
- 7.Joyce JM, Idea RJ, Grossman SJ, Liss RG, Lyons JB. Multiple brown tumors in unsuspected primary hyperparathyroidism mimicking metastatic disease on radiograph and bone scan. Clin Nucl Med 1994;19:630-5. [Google Scholar | PubMed]
- 8.Misiorowski W, Czajka-Oraniec I, Kochman M, Zgliczyński W, Bilezikian JP. Osteitis fibrosa cystica-a forgotten radiological feature of primary hyperparathyroidism. Endocrine 2017;58:380-5. [Google Scholar | PubMed]
- 9.Mirels H. Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures. Clin Orthop Relat Res 1989;249:256-64. [Google Scholar | PubMed]
- 10.Rubin MR, Bilezikian JP, McMahon DJ, Jacobs T, Shane E, Siris E, et al. The natural history of primary hyperparathyroidism with or without parathyroid surgery after 15 years. J Clin Endocrinol Metab 2008;93:3462-70. [Google Scholar | PubMed]