Radiological evaluation methods played a major role in the time to diagnosis of idiopathic transient osteoporosis of the hip, while evaluation with plain radiographs resulted in increased time to diagnosis (TTD), utilization of magnetic resonance imaging significantly reduced the TTD to institute appropriate management at the earliest.
Dr. Sathish Muthu, Orthopaedic Research Group, Coimbatore, Tamil Nadu, India. E-mail: drsathishmuthu@gmail.com
Introduction: Transient osteoporosis of the hip (TOH) is a poorly recognized self-limiting clinical entity. Due to a lack of awareness among the clinicians, the condition is often misdiagnosed leading to inappropriate treatment, thereby lengthening the time to diagnosis (TTD). In this study, we analyze the delay in TTD of TOH using plain radiographs and present the optimal management strategy.
Materials and Methods: We retrospectively collected the data of patients who were diagnosed with TOH from March 2017 to March 2022. A total of 10 patients with a mean age of 43.7 years (range 33–56 years) were included in the study. The mean time to presentation from the onset of symptoms was 4 weeks (range 2–8 weeks) Radiologic evaluation with radiographs was sensitive in only 8 patients with osteopenia, whereas magnetic resonance imaging (MRI) was sensitive in all the patients and aided in early diagnosis of TOH. Radiographic evaluation alone leads to a mean delay in TTD of 1.6 weeks (range 0–8 weeks) in our study. All the patients were treated conservatively without any major complications.
Conclusion: Plain radiographs were not sensitive in the early detection of TOH and increased the TTD by 1.6 weeks, however, MRI imaging was found to be highly sensitive and specific in diagnosing TOH.
Keywords: Avascular necrosis, reflex sympathetic dystrophy, transient osteoporosis of the hip, magnetic resonance imaging, X-ray.
Transient osteoporosis of the hip (TOH) is an idiopathic, self-limiting condition that clinically presents with unexplained hip pain and limping. It is often associated with painful range of motion at the hip joint and the laboratory and the radiological findings are non-specific [1-3]. Initial research regarding this condition dates back to 1959 when Curtiss and Kincaid [1] described three women in the past months of pregnancy who suffered from hip and thigh pain and tenderness, limping, and functional disability of the affected limb, which spontaneously resolved over a few months. Later Lequesne in 1968 coined the term transient osteoporosis of the hip [4]. As the research has progressed into this clinical entity, various other terms such as complex regional pain syndrome (CRPS) Type 1, bone marrow edema syndrome, transient demineralization, migratory osteolysis, and algodystrophy of the hip have been associated and used in synonym with TOH [4-6]. The diagnosis of TOH is often delayed or missed due to the paucity of literature regarding the disease hence leading to inappropriate management, thereby lengthening the time to diagnosis (TTD). Despite the myriad strategies available to evaluate this hip disease, radiographs remain the common and first-line method of evaluation. Although TOH presents with radiological features such as subchondral cortical loss and osteopenia involving the femoral head and neck in radiographs, the features are not always present in all the patients of TOH who present early. However, magnetic resonance imaging (MRI) helps in the early identification of the disease with features such as bone marrow edema involving the femoral head and neck, even extending to the intertrochanteric region without findings of osteonecrosis. Other signs such as subchondral fractures and sparing of the medial femoral head by bone marrow edema can be found in almost 90% of patients which disappears toward the later stages of the disease. MRI has been considered the modality of choice to investigate and diagnose TOH at the early stages before evident sign sets in the radiographs. However, the literature on the delay in the TTD with the use of radiographs as the first-line evaluation tool is limited. In this study, we analyze the time delay in diagnosing TOH using radiographs as the first-line evaluation tool.
This retrospective single institutional study was performed in a tertiary care hospital after obtaining institutional ethical committee approval. Ten (n = 10) patients who presented with complaints of hip pain from May 2017 to September 2022 and were diagnosed to have TOH clinically and radiologically were included in the study. A detailed history was collected from the case records of all these patients, including the history of trauma, steroid use (oral or topical) alcohol and smoking, and other endocrine disorders. Routine clinical examination and investigations including complete blood count, erythrocyte sedimentation rate, C-reactive protein, and the rheumatoid factor were retrieved and evaluated. The radiological investigations, including plain radiographs, MRI, and other relative investigations were also retrieved and studied. The mean age of the patients included in the analysis was 43.7 years (range 33–56 years). There were 8 (80%) male and 2 (20%) female patients. Presentation of pain was seen in the left hip in 4 (40%) patients and 6 (60%) patients presented with pain on the right side. The mean duration of the period from the onset of symptoms to the first consultation was 4 weeks (range 2–8 weeks). The demographic details for all the patients are shown in Table 1.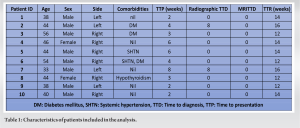 The chief complaint for the majority of the patients was sudden onset pain over the hip and the groin region. The pain which was sharp and pricking in nature was aggravated on prolonged walking or during exercise and was partially relieved on taking rest. Nocturnal pain was reported by 8 (80%) patients. There was no history of trauma, no history of steroid or regular alcohol intake in any of the study participants. Two (20%) patients had a history of diabetes mellitus, 1 (10%) patient had a history of systemic hypertension, 1 (10%) patient was hypothyroid on regular medications, and 1 (10%) patient had a history of both diabetes mellitus and systemic hypertension. On examination of the affected hip, no external skin changes were noted. Tenderness on deep palpation was present and there was a painful restriction of the movements of the hip joint. No proximal migration or thickening of the greater trochanter was seen and no limb length discrepancy was noted in either of the participants. All the patients were evaluated radiologically using radiographs as the first-line evaluation with a bilateral hip anteroposterior view. Radiographs demonstrated localized osteopenia, extending from the femoral head into the intertrochanteric region in 8 (80%) patients as shown in Fig. 1.
The chief complaint for the majority of the patients was sudden onset pain over the hip and the groin region. The pain which was sharp and pricking in nature was aggravated on prolonged walking or during exercise and was partially relieved on taking rest. Nocturnal pain was reported by 8 (80%) patients. There was no history of trauma, no history of steroid or regular alcohol intake in any of the study participants. Two (20%) patients had a history of diabetes mellitus, 1 (10%) patient had a history of systemic hypertension, 1 (10%) patient was hypothyroid on regular medications, and 1 (10%) patient had a history of both diabetes mellitus and systemic hypertension. On examination of the affected hip, no external skin changes were noted. Tenderness on deep palpation was present and there was a painful restriction of the movements of the hip joint. No proximal migration or thickening of the greater trochanter was seen and no limb length discrepancy was noted in either of the participants. All the patients were evaluated radiologically using radiographs as the first-line evaluation with a bilateral hip anteroposterior view. Radiographs demonstrated localized osteopenia, extending from the femoral head into the intertrochanteric region in 8 (80%) patients as shown in Fig. 1.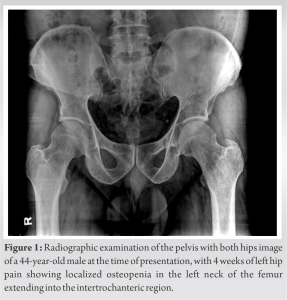 There were no features suggestive of a reduction of the joint space or any change in the sphericity of the femoral head. The other two patients demonstrated normal radiographs and were managed conservatively with analgesics. MRI was ordered to confirm the diagnosis in the eight cases with features suggestive of TOH, whereas the other two patients were ordered for MRI during their second visit 8 weeks following the primary visit. MRI showed features of low-signal intensity in T1 images and a high-signal intensity noted in T2 and STIR sequences extending from the femoral head into the intertrochanteric region, representing edema in the bone marrow as shown in Fig. 2.
There were no features suggestive of a reduction of the joint space or any change in the sphericity of the femoral head. The other two patients demonstrated normal radiographs and were managed conservatively with analgesics. MRI was ordered to confirm the diagnosis in the eight cases with features suggestive of TOH, whereas the other two patients were ordered for MRI during their second visit 8 weeks following the primary visit. MRI showed features of low-signal intensity in T1 images and a high-signal intensity noted in T2 and STIR sequences extending from the femoral head into the intertrochanteric region, representing edema in the bone marrow as shown in Fig. 2.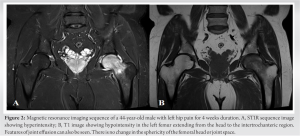 Joint effusion was seen in 7 (70%) patients. There was no obvious subchondral collapse or joint space reduction. Serial MRI scans showed the joint space was maintained and no changes were seen in the shape of the femoral head as shown in Fig. 2. Hence, we noted a mean delay of 1.6 weeks (range 0–8 weeks) in diagnosing TOH. After confirming the diagnosis clinically and radiologically, all patients had undergone conservative treatment. Partial weight-bearing mobilization with support was advised for 2 weeks, along with pain management through non-steroidal anti-inflammatory drugs (NSAIDs). Initially, low-dose aspirin (75 mg once a day) was started for all patients. Oral vitamin D3 calcium supplements and bisphosphonates were also given. All the patients were followed up initially for pain management for 2 weeks until 1 month, and then every 3-month interval for 1 year. During follow-up, patients underwent pelvic radiographs and screening MRI at 3 and 6 months as shown in Fig. 3.
Joint effusion was seen in 7 (70%) patients. There was no obvious subchondral collapse or joint space reduction. Serial MRI scans showed the joint space was maintained and no changes were seen in the shape of the femoral head as shown in Fig. 2. Hence, we noted a mean delay of 1.6 weeks (range 0–8 weeks) in diagnosing TOH. After confirming the diagnosis clinically and radiologically, all patients had undergone conservative treatment. Partial weight-bearing mobilization with support was advised for 2 weeks, along with pain management through non-steroidal anti-inflammatory drugs (NSAIDs). Initially, low-dose aspirin (75 mg once a day) was started for all patients. Oral vitamin D3 calcium supplements and bisphosphonates were also given. All the patients were followed up initially for pain management for 2 weeks until 1 month, and then every 3-month interval for 1 year. During follow-up, patients underwent pelvic radiographs and screening MRI at 3 and 6 months as shown in Fig. 3.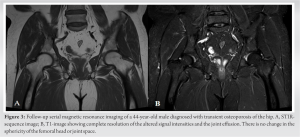
The diminution of pain and ability to get a full painless range of motion at the hip joint was considered the end point for the treatment and the patient was regarded as treated. The patients became symptom-free at a mean interval of 16 weeks after treatment (range 12–24 weeks). Nine patients reported complication-free recovery, whereas one patient presented with the complication of contralateral TOH and underwent the same treatment protocol. The patient reported complete resolution of the symptoms over the contralateral hip within 5 months of this treatment regimen.
TOH is an uncommon disorder of unknown etiology. It clinically presents as a sudden, dull aching pain over the hip and the thigh region. The pain often leads to abnormalities in gait and limping, which is often disproportionate to the symptoms. However, the range of motion at the hip joint is usually preserved [4]. Although first reported in pregnant females, TOH has been reported to have a male predilection and affects most commonly the age group of 40–50 years [7,8]. The disease usually manifests as unilateral involvement, however, bilateral involvement has been described in pregnant women in 25–30% of the cases [9]. Lequesne, in their case series in 1968, described phases of the disease activity. The first phase, which is seen during the 1st month is characterized by the rapid aggravation of pain and functional disability with normal radiographs. During the second phase, which goes on for around 1–2 months, the clinical signs and symptoms reach maximal intensity and radiological osteopenia appears. The final phase is the regression of the disease and gradual restitution of the bone mineralization, a phase which usually lasts up to 4 months [4]. In the present study, all the patients went through a similar progression of the disease, with spontaneous resolution of the symptoms.
The pathogenesis of TOH is complex and unclear. Multiple theories have been put forward explaining this condition, including microvascular injury, local hyperemia-impaired venous return with marrow edema, nontraumatic reflex sympathetic dystrophy, metabolic pathologies, viral infection, neurological, and endocrine factors [10]. Research on this entity has led to the theory that TOH may be a subtype of CRPS owing to the similarities in presentation as it has an unidentifiable cause and unknown precipitating event and pain which is out of proportion to the radiological and clinical findings [11]. However, the characteristic cutaneous changes seen in the case of CRPS are not seen in TOH.
Due to this non-specificity of presentation and radiographical features, the misdiagnosis of TOH is very common and needs to be addressed to differentiate it from other conditions that may require surgical intervention. Patients might initially present with normal radiographs, hence based on this study we noted a TTD delay of 1.6 weeks (range 0–8 weeks) using radiographs only as the initial line of management which is in line with the existing evidence [12]. Apart from the osteopenia in the head and neck region, the subchondral cortical loss seen on plain radiographs is said to be the pathognomonic feature of TOH, along with adjacent joint effusion and preserved joint space. Osseous erosion or subchondral collapse is usually not seen [11].
Misdiagnosis of TOH as avascular necrosis (AVN) is very common, due to the similar clinical presentation of sudden onset, and unexplained hip pain, and hence researchers have tried to differentiate between the two clinical entities. The osteopenia seen on plain radiographs is usually only seen after 4–8 weeks and hence lacks the sensitivity for the diagnosis. On MRI scans, the abnormalities may be reported within the first 48 h of the onset of the disease [12].
The characteristic changes that can be observed in TOH are a pattern of diffuse edema in the absence of any focal defects. The articular surface is intact and the characteristic double line sign seen in AVN is absent. The extent of the edema pattern in the case of TOH usually exceeds in amount expected in the case of AVN. The edema pattern can be identified by the homogeneously hypointense signal in T1 weighted images and a homogeneously hyperintense signal in T2 STIR images. The signal intensity change can be seen extending from the superior articular surface of the femoral head, extending into the neck and the intertrochanteric region [13,14]. This diffuse edema pattern seen in TOH is of low specificity, but as Vande Berg et al. noted in their prospective clinical case series, the absence of any subchondral lesions has a 100% positive predictive value for transient lesions [5]. Serial screening using MRI will be more helpful in differentiating the two as there are different distinct stages the two disease progress through.
Bone scans may be used to differentiate between TOH and AVN. In the case of TOH, there is a markedly increased homogeneous uptake, whereas, there is a cold spot in the case of AVN owing to vascular occlusion in an early stage of disease. The characteristic doughnut sign which can be appreciated in the case of AVN in the late stages is not seen in TOH [11]. However, the specificity of bone scans for TOH is low [15]. In addition to the differentiating features, radionuclide scanning can also serve as an effective screening tool as it helps in revealing the asymptomatic involvement of other body parts such as the contralateral hip [11]. Bone scans were not done in our case series, as the findings in MRI were specific to reach the diagnosis.
As TOH is a self-limiting disease, only symptomatic and supportive treatment is sufficient using NSAIDs, protected weight-bearing, and physiotherapy exercises [16,17]. Although in longer-duration cases, the non-weight-bearing is useful and efficient, it comes with the disadvantage of disuse mineralization on the affected joint. Few studies in the available literature show accelerated and effective treatment using bisphosphonate either orally or intravenously and the use of calcitonin with the dosage of 200 IU daily as a nasal spray for reduced bone loss during acute and early stages of disease [18,19]. In a few studies involving severe painful conditions, a prostacyclin analog like iloprost has proven effective as they cause vasodilation and decreased permeability of smaller capillaries [20]. Its effectiveness in TOH is still under consideration. In our series, we used a combination of oral NSAIDs and protected weight-bearing. In the present study, the average time for resolution of symptoms was 13.6 weeks as shown in Table 1. No long-term complications were noted in 9 out of the 10 study participants. However, one patient developed contralateral hip involvement and underwent the same treatment protocol. No major long-term complications were noted in literature on this condition [15,16,17,20].
Despite with available literature, knowledge the TOH is often still overlooked and misdiagnosed as other mimicking conditions like AVN. TOH is a distinct non-destructive and self-limiting condition of the hip that presents spontaneously with hip pain and is managed conservatively. Awareness of this entity is important to the clinicians for an early diagnosis and to avoid unnecessary surgical treatment, thereby providing appropriate treatment. Plain radiographs were not sensitive in the early detection of TOH and resulted in a diagnostic delay of 1.6 weeks. However, MRI particularly as a serial screening tool was found to be highly sensitive and specific in diagnosing and managing TOH.
- TOH is a distinct non-destructive and self-limiting condition of the hip that presents spontaneously with hip pain and is managed conservatively.
- Awareness of this entity is important to the clinicians for an early diagnosis and to avoid unnecessary surgical treatment, thereby providing appropriate treatment.
- Plain radiographs were not sensitive in the early detection of TOH and resulted in a diagnostic delay of 1.6 weeks.
- MRI particularly as a serial screening tool was found to be highly sensitive and specific in diagnosing and managing TOH.
References
- 1.Curtiss PH Jr., Kincaid WE. Transitory demineralization of the hip in pregnancy. A report of three cases. J Bone Joint Surg Am 1959;41-A:1327-33. [Google Scholar | PubMed]
- 2.Shifrin LZ, Reis ND, Zinman H, Besser MI. Idiopathic transient osteoporosis of the hip. J Bone Joint Surg Br 1987;69:769-73. [Google Scholar | PubMed]
- 3.Rocchietti March M, Tovaglia V, Meo A, Pisani D, Tovaglia P, Aliberti G. Transient osteoporosis of the hip. Hip Int 2010;20:297-300. [Google Scholar | PubMed]
- 4.Lequesne M. Transient osteoporosis of the hip. A nontraumatic variety of Südeck’s atrophy. Ann Rheum Dis 1968;27:463-71. [Google Scholar | PubMed]
- 5.Vande Berg BC, Lecouvet FE, Koutaissoff S, Simoni P, Malghem J. Bone marrow edema of the femoral head and transient osteoporosis of the hip. Eur J Radiol 2008;67:68-77. [Google Scholar | PubMed]
- 6.Wilson AJ, Murphy WA, Hardy DC, Totty WG. Transient osteoporosis: Transient bone marrow edema? Radiology 1988;167:757-60. [Google Scholar | PubMed]
- 7.Hadidy AM, Al Ryalat NT, Hadidi ST, Tarawneh ES, Hadidi MT, Samara OA, et al. Male transient hip osteoporosis: Are physicians at a higher risk? Arch Osteoporos 2009;4:41-5. [Google Scholar | PubMed]
- 8.Niimi R, Sudo A, Hasegawa M, Fukuda A, Uchida A. Changes in bone mineral density in transient osteoporosis of the hip. J Bone Joint Surg Br 2006;88:1438-40. [Google Scholar | PubMed]
- 9.Escolà A, Pons M, Pasarin A, Majó J. Idiopathic transient osteoporosis of the pelvis in a non-pregnant young woman: A case study. Hip Int 2009;19:71-4. [Google Scholar | PubMed]
- 10.Harrington S. Idiopathic TOH. Phys Sportsmed 2000;28:34. [Google Scholar | PubMed]
- 11.Vaishya R, Agarwal AK, Kumar V, Vijay V, Vaish A. Transient osteoporosis of the hip: A mysterious cause of hip pain in adults. Indian J Orthop 2017;51:455-60. [Google Scholar | PubMed]
- 12.Daniel WW, Sanders PC, Alarcón GS. The early diagnosis of transient osteoporosis by magnetic resonance imaging. A case report. J Bone Joint Surg Am 1992;74:1262-4. [Google Scholar | PubMed]
- 13.Bloem JL. Transient osteoporosis of the hip: MR imaging. Radiology 1988;167:753-5. [Google Scholar | PubMed]
- 14.Balakrishnan A, Schemitsch EH, Pearce D, McKee MD. Distinguishing transient osteoporosis of the hip from avascular necrosis. Can J Surg 2003;46:187-92. [Google Scholar | PubMed]
- 15.Bramlett KW, Killian JT, Nasca RJ, Daniel WW. Transient osteoporosis. Clin Orthop Relat Res 1987;222:197-202. [Google Scholar | PubMed]
- 16.Bruinsma BJ, LaBan MM. The ghost joint: Transient osteoporosis of the hip. Arch Phys Med Rehabil 1990;71:295-8. [Google Scholar | PubMed]
- 17.Crespo E, Sala D, Crespo R, Silvestre A. Transient osteoporosis. Acta Orthop Belg 2001;67:330-7. [Google Scholar | PubMed]
- 18.Kibbi L, Touma Z, Khoury N, Arayssi T. Oral bisphosphonates in treatment of transient osteoporosis. Clin Rheumatol 2008;27:529-32. [Google Scholar | PubMed]
- 19.Mitchell DG, Rao VM, Dalinka MK, Spritzer CE, Alavi A, Steinberg ME, et al. Femoral head avascular necrosis: Correlation of MR imaging, radiographic staging, radionuclide imaging, and clinical findings. Radiology 1987;162:709-15. [Google Scholar | PubMed]
- 20.Nicol RO, Williams PF, Hill DJ. Transient osteopaenia of the hip in children. J Pediatr Orthop 1984;4:590-2. [Google Scholar | PubMed]










