This case report highlights the diagnostic challenges posed by this condition, emphasizes the importance of considering it in the differential diagnosis, and underscores the need for timely surgical intervention
Dr. Mainak Roy, Department of Orthopaedics, All India Institute of Medical Sciences, Nagpur, Maharashtra, India. E-mail: mainakroy30@gmail.com
Introduction: Periosteal chondromas are rare, slow-growing, benign cartilaginous tumors arising from the cortical surface of the bone, beneath the periosteal membrane. Typically affect young males, the most common site being the proximal humerus. There have been no reported cases of periosteal chondroma of the talus in the literature.
Case Report: A 9-year-old Indian boy presented with a 1.5-year history of atraumatic right ankle pain and swelling, exacerbated by walking, with limited dorsiflexion. Physical examination revealed a firm, painless swelling on the anterior ankle’s talar region, accompanied by equinus deformity. Radiography displayed osseous masses on the anterior talus. Magnetic resonance imaging indicated well-defined osseous growths originating from the talus’s anterior aspect, likely osteochondromas, with adjacent osseous fragments in the tibiotalar joint, suggestive of loose bodies, supporting a clinical diagnosis of synovial chondromatosis. Surgical excision revealed whitish, hard, irregular tissue, confirmed as periosteal chondroma on histopathology. After 6 months, the patient is pain-free with unrestricted movement and no clinical or radiological signs of recurrence.
Conclusion: This case report presents a unique instance of previously unreported talus periosteal chondroma, adding novelty to medical literature. It details the diagnostic challenges and its intricacies. It provides a comprehensive overview of clinical presentation, imaging and histopathological findings, differentials and provisional diagnosis, surgical approach, and post-operative outcomes. The successful surgical management, along with the specific details of the surgical procedure (anteromedial approach, excision, and curettage), adds practical insights for orthopedic surgeons and contributes to the existing knowledge on treatment strategies for talus periosteal chondroma. This report will serve as an excellent educational resource.
Keywords: Periosteal chondroma, talus, pediatric patient, surgical management, rare case report.
Periosteal chondromas are uncommon, benign cartilaginous tumors originating in the periosteum, typically manifesting as gradually progressive pain and swelling [1]. Radiographically, they are characterized by saucerization of the adjacent cortex and a well-formed sclerotic periosteal reaction [1], inducing erosion and sclerosis of the neighboring bone cortex [2]. Histopathologically, periosteal chondromas display hypercellularity, nuclear pleomorphism, and binucleation. Diagnosing them is challenging due to similarities with other periosteal-origin tumors [3]. Surgical excision with underlying bone curettage remains the preferred treatment [3,4]. The rarity of periosteal chondroma of the talus adds to the diagnostic and therapeutic complexities. This report details the successful surgical management of a pediatric talus periosteal chondroma case, contributing insights to this unusual condition.
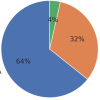
A 9-year-old Indian boy without any prior trauma presented with a 1.5-year history of pain and swelling in his right ankle, which had emerged subtly and gradually progressed. His gait had also changed. There were no significant medical or family history factors. Notably, the pain and swelling had intensified in the past 6 months. On physical examination, antalgic gait with restricted dorsiflexion of the affected ankle was noted. Local examination revealed a firm and non-tender swelling located in the anterior aspect of the ankle. In addition, there was a 20-degree equinus deformity. Examination of other systems was unremarkable. Routine blood investigations, immune and infection markers, were all within the normal range. Plain X-ray showed osseous masses over the anterior talus with loose bodies (Fig. 1). Magnetic resonance imaging (MRI) revealed a well-defined osseous projection arising from the anterior aspect of the talar neck with MRI reporting suggestive of osteochondroma (Fig. 2). No evidence of significant thickened cartilage was seen. Two well-defined osseous fragments seen adjacent to the above lesion in the tibiotalar joint suggestive of loose bodies were also seen.
Provisional diagnosis
Based on clinical and imaging findings, a provisional clinical diagnosis of ankle synovial chondramatosis was made and surgical excision was planned.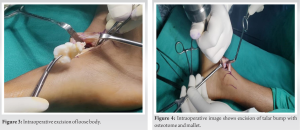
Treatment
Surgical excision of the lesion: An anteromedial approach to the talus was done which exposed two hard, whitish, irregular masses (loose bodies) on the anterosuperior aspect of the talus of sizes 3 × 2 × 1 cm and 2 × 2 × 1 cm (Fig. 3). They were removed and excision of mass over the anterosuperior aspect of the talus was done with osteotome and mallet with curettage (Fig. 4). Excised masses (Fig. 5) were sent for histopathological examination. Intraoperative dorsiflexion of ankle was restored to 10 degrees. Post-operative radiographs showed normal contour of the talus with complete resection of the talar bump with no loose bodies. Histopathological examination revealed hyaline cartilage enveloped by fibrocollagenous (periosteal) tissue forming reactive bone (Fig. 6) with a single pyknotic nucleus, confirming periosteal chondroma.
Postoperatively, course was uneventful. On 6-month follow-up, the patient was pain-free, had improved ankle range of motion and normal gait. Active and passive ankle dorsiflexion was possible up to 10 degrees and 20 degrees, respectively, with 30 degrees of plantarflexion (Fig. 7). No residual deformity was observed. No clinical as well as radiological signs (Fig. 8) of recurrence were noted.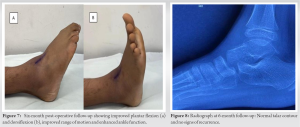
Periosteal chondromas are rare, benign cartilaginous tumors arising in the periosteum, primarily affecting children and young adults, commonly affecting the tubular bones of the hands, feet, and long bones of the extremities [3,4], constituting only 2% of all primary bone neoplasms [5]. Usual symptoms include insidious pain and swelling [1]. Diagnosis is challenging due to similarities with other periosteal-origin tumors, such as periosteal osteosarcoma, osteochondromas, fibrous cortical defects, cortical desmoids, chondrosarcomas, and synovial sarcomas [3]. An infrequent possibility is synovial osteochondromatosis, which may present with loose bodies [6]. Radiographically, periosteal chondromas display a distinctive appearance, characterized by saucerization of the adjacent cortex and a well-formed sclerotic periosteal reaction [1]. They induce erosion and sclerosis of the neighboring bone cortex, distinguishing them from osteochondromas and solitary enchondromas [2]. MRI shows soft-tissue masses on the bone surface, exerting pressure on the adjacent cortical bone and forming a hypointense rim, often with a lobulated appearance. The tumor tissue typically appears hypo- or isointense relative to muscle on T1-weighted MRI images and hyperintense relative to fat on T2-weighted images, sometimes with significant calcifications within the tumor [7]. Histology exhibits hypercellularity, nuclear pleomorphism, and binucleation, potentially leading to a misdiagnosis of chondrosarcoma. [8]. The preferred treatment is surgical excision with underlying bone curettage [3,4]. The pathogenesis remains unclear, with potential associations with trauma [9]. Congenital cases have also been reported [10]. Genetic mutations in isocitrate dehydrogenase 1 and isocitrate dehydrogenase 2 are also a potential association [11]. Our patient had no significant history of trauma. The absence of chondrocytes (cartilage cells) at the tumor site suggests that the tumor may arise from a unique cell in the periosteum, which is believed to be a totipotent primitive cell in the periosteum [12]. Distinguishing periosteal chondroma from other conditions can be challenging. Histopathological patterns can aid in differentiation of these lesions. Our patient had a high suspicion of osteochondroma. Osteochondromas develop on the bone’s surface, while periosteal chondromas likely form through subperiosteal cartilage formation, unrelated to metaphyseal plates [13]. Periosteal osteosarcoma presents with irregular lobules of chondroblastic tissue and areas of osteoid formation [14]. Enchondromas contain mature hyaline cartilage with a lobular pattern and small chondrocytes in lacunar spaces [15]. Chondrosarcomas, a major differential diagnosis [16], tend to be larger (1) and can extend into soft tissue, typically occurring in older individuals [13]. As periosteal chondroma is a benign tumor, there are usually no mitotic figures, atypia, or necrosis found on histology [17]. Our case involved an extremely rare periosteal chondroma of the talus. The diagnostic process was complex, initially leaning toward osteochondromas, but intraoperative findings suggested synovial chondromatosis. The definitive diagnosis was confirmed through histopathological examination, confirming periosteal chondroma. Post-surgery, the patient experienced pain relief, improved range of motion, and no signs of recurrence. As shown in previous literature, chondromas, being benign lesions, rarely recur [18]. This case highlights the rarity, diagnostic challenges, and successful surgical management of talus periosteal chondroma, contributing to our understanding of this rare condition in the field of orthopedics.
To the best of our knowledge, no prior case of talus periosteal chondroma has been documented. Diagnosis can be intricate due to the absence of specific markers, necessitating differentiation from similar conditions. Surgical intervention, specifically en bloc resection and bone curettage, is the preferred treatment, yielding favorable post-operative outcomes with pain relief and improved function. This report underscores the rarity, diagnostic intricacies, distinctive features, and treatment strategies associated with talus periosteal chondroma, making it a noteworthy case in the realm of foot and ankle surgery.
This case report enriches our understanding of periosteal chondromas, underscoring their infrequency, diagnostic complexities, and the significance of timely surgical management. It provides a valuable reference for orthopedic practitioners, emphasizing the unique attributes and treatment considerations of talus periosteal chondroma in pediatric patients.
References
- 1.Robinson P, White LM, Sundaram M, Kandel R, Wunder J, McDonald DJ, et al. Periosteal chondroid tumors: Radiologic evaluation with pathologic correlation. AJR Am J Roentgenol 2001;177:1183-8. [Google Scholar | PubMed]
- 2.Lichtenstein L, Hall JE. Periosteal chondroma; a distinctive benign cartilage tumor. J Bone Joint Surg 1952;34:691-7. [Google Scholar | PubMed]
- 3.Kirchner SG, Pavlov H, Heller RM, Kaye JJ. Periosteal chondromas of the anterior tibial tubercle: Two cases. AJR Am J Roentgenol 1978;131:1088-9. [Google Scholar | PubMed]
- 4.Nojima T, Unni KK, McLeod RA, Pritchard DJ. Periosteal chondroma and periosteal chondrosarcoma. Am J Surg Pathol 1985;9:666-77. [Google Scholar | PubMed]
- 5.Miller SF. Imaging features of juxtacortical chondroma in children. Pediatr Radiol 2014;44:56-63. [Google Scholar | PubMed]
- 6.Milgram JW. Synovial osteochondromatosis: A histopathological study of thirty cases. J Bone Joint Surg Am 1977;59:792-801. [Google Scholar | PubMed]
- 7.Woertler K, Blasius S, Brinkschmidt C, Hillmann A, Link TM, Heindel W. Periosteal chondroma: MR characteristics. J Comput Assist Tomogr 2001;25:425-30. [Google Scholar | PubMed]
- 8.Nishio J, Arashiro Y, Mori S, Iwasaki H, Naito M. Periosteal chondroma of the distal tibia: Computed tomography and magnetic resonance imaging characteristics and correlation with histological findings. Mol Clin Oncol 2015;3:677-81. [Google Scholar | PubMed]
- 9.Morisaki Y, Takagi K, Ishii Y, Furuya T, Ishikawa M, Tanaka S. Periosteal chondroma developing in a rib at the side of a chest wall wound from a previous thoracotomy: Report of a case. Surg Today 1996;26:57-9. [Google Scholar | PubMed]
- 10.Domson GF, Bush CH, Reith JR, Rajaram A, Scarborough MT, Gibbs CP. Periosteal chondroma at birth. Skeletal Radiol 2008;37:559-62. [Google Scholar | PubMed]
- 11.Amary MF, Bacsi K, Maggiani F, Damato S, Halai D, Berisha F, et al. IDH1 and IDH2 mutations are frequent events in central chondrosarcoma and central and periosteal chondromas but not in other mesenchymal tumours. J Pathol 2011;224:334-43. [Google Scholar | PubMed]
- 12.Gao Y, Wang JG, Liu H, Gao CP. Periosteal chondroma of the rib: A case report. World J Clin Cases 2022;10:8330-5. [Google Scholar | PubMed]
- 13.Motififard M, Hatami S, Jamalipour Soufi G. Periosteal chondroma of pelvis-an unusual location. Int J Burns Trauma 2020;10:174-80. [Google Scholar | PubMed]
- 14.Cesari M, Alberghini M, Vanel D, Palmerini E, Staals EL, Longhi A, et al. Periosteal osteosarcoma: A single-institution experience. Cancer 2011;117:1731-5. [Google Scholar | PubMed]
- 15.Torbaghan SS, Ashouri M, Naderi NJ, Baherini N. Histopathologic differentiation between enchondroma and well-differentiated chondrosarcoma: Evaluating the efficacy of diagnostic histologic structures. J Dent Res Dent Clin Dent Prospects 2011;5:98-101. [Google Scholar | PubMed]
- 16.Al-Qudah AS, Abu-Ali HM, Al-Hussaini MA, Massad IM. Periosteal chondroma of the clavicle: Case report and review of the literature. Int J Surg 2009;7:140-1. [Google Scholar | PubMed]
- 17.Prabhakar G, Dev A, Ghazanfari Amlashi F, Rajani R. Periosteal chondroma of the pelvis: An uncommon tumor in an unusual location. Cureus 2021;13:e17163. [Google Scholar | PubMed]
- 18.Khadka R, Pachhai P, Gurung A, Shrestha DK, Shilpakar SK. Intraspinal periosteal chondroma in upper thoracic spine causing cord compression and myelopathy: A case report. Int J Surg Case Rep 2022;93:106964. [Google Scholar | PubMed]