Operative treatment of patients with an unstable pathological femur fracture through a large benign tumor is indicated, and it allows for early mobilization, likely tumor resolution, and fracture healing.
Mr. Nathan Cai, Department of Education, The University of Miami Leonard M. Miller School of Medicine, 1600 NW 10th Ave #1140, Miami 33136, Florida. E-mail: nac157@miami.edu
Introduction: Non-ossifying fibroma (NOF) is a common benign fibrogenic bone lesion commonly found in the metaphysis of long bones. While small NOFs are typically asymptomatic and left untreated, large NOFs are often associated with pathologic fractures that can be treated conservatively or operatively. To our knowledge, the NOF presented in this case report is one of the largest reported in the literature.
Case Report: We present a case of a 12-year-old Hispanic female who presented to our institution after falling off a horse and landing on her right leg and wrist. Radiographs revealed a right distal femur fracture through an unusually large lytic bone lesion. The patient was treated with curettage, grafting, open reduction, and internal fixation, given the unstable and pathological nature of the fracture.
Conclusion: This case substantiates the literature that large fractures through a NOF can be appropriately managed operatively. However, orthopedic surgeons should be aware of the risks of surgery, including infection, when considering operative management of patients who present with large unstable pathologic fractures through a NOF.
Keywords: Non-ossifying fibroma, pediatrics, open reduction, and internal fixation.
Non-ossifying fibroma (NOF) is a common benign fibrogenic bone lesion with an estimated incidence of 30–40% in children and adolescents [1,2]. NOFs are most commonly found in the metaphysis of long bones, particularly the distal femur, proximal and distal tibia, and fibula [3,4]. They are characterized by a well-defined, radiolucent lesion in the cortical bone and can be staged by their radiomorphologic features [2,5]. The average length of NOFs can range from 21 to 47 mm based on their stage [3]. Most NOFs are small, asymptomatic, and left untreated [2,6]. On the other hand, larger NOFs can cause pathologic fractures which are typically treated with adequate immobilization [7-9]. Prophylactic curettage and bone grafting can be considered in NOFs larger than 50% of the bone’s diameter or >33 mm in length because large NOFs are more prone to pathologic fracture [3,9,10]. Unstable fractures or those that cannot be acceptably reduced by closed methods should be considered for internal fixation [9]. To the best of our knowledge, there are a limited number of reported cases of pathologic fractures through NOFs that require open reduction and internal fixation (ORIF) [6,11]. Moreover, there are few reported cases of NOFs larger than 5 cm [3,10]. Here, we present a case of a pathologic fracture through an unusually large NOF in the distal femur that was treated with ORIF.
A 12-year-old Hispanic female initially presented to an outside emergency department after falling off a horse and landing on her right wrist and leg. Whole-body scans were conducted. The only positive finding was a right distal femur fracture concerning for a lytic bone lesion, for which she was recommended to transfer to our emergency department. Her mother and father both endorsed that the patient experienced right knee pain for the past 3–6 months, causing her to quit volleyball. They report that the patient’s primary care physician was unable to provide a diagnosis for the knee pain. She had no other previous significant history. Clinically, the right lower extremity was tender, demonstrated moderate swelling with intact skin, and showed no ecchymosis. The compartments were soft and the distal neurovascular examination was intact. A plain film radiograph of the right femur demonstrated a large lytic lesion with well-defined borders measuring up to 17 cm at the distal diaphysis and an oblique comminuted fracture without articular involvement (Fig. 1 and 2).
Given the unstable and pathological nature of the fracture, a decision was made to subsequently perform a curettage, grafting, open biopsy, and ORIF of the right distal femur (Fig. 3 and 4). The procedure was performed through the standard lateral approach to the distal femur coupled with the subvastus approach. Once we were satisfied with our exposure, we then preceded to curette the cyst in a circumferential manner, ensuring all of the cyst and lesion were removed. Afterward, a mixture of mineralized cortical bone and Osteocrete was inserted into the canal of the femur to fill the entire site of the previous cyst. Next, we appropriately reduced the fracture and fixed an appropriately sized and contoured plate to the distal femur. After the incision was closed, the patient was placed in a long leg splint and instructed to be non-weight-bearing for 2 weeks. She was discharged on post-operative day 4 without complications.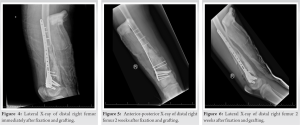
At her 2-week follow-up in the clinic, the patient had appropriate post-operative pain. Radiographs showed an excellent position of the fracture (Fig. 5 and 6). Stitches were removed and a cylinder cast was applied. Histopathology reported NOF.
One month after her initial operation, the patient reported a significant amount of thick, brown drainage from the proximal aspect of her long-leg cast. She denied any recent fevers, interval trauma, or drainage before this instance. On evaluation in the emergency department, the patient underwent a computed tomography scan with contrast of her right femur which demonstrated a deep rim-enhancing abscess with air and fluid in the canal suggestive of an intramedullary abscess. The patient subsequently underwent an incision and drainage of her right distal femur. After opening the previous scar, there was a significant amount of pus, necrotic tissue, and subcutaneous fat necrosis. We then opened the iliotibial band layer and discovered more pus and an old hematoma that was evacuated. Approximately 600 mL of necrotic tissue and old blood products were evacuated. We further discovered an abscess within the femoral canal. The hardware appeared to be moderately intact, and the tissue was debrided thoroughly until the patient became hypotensive and subsequently decompensated. Fortunately, she was successfully resuscitated by the anesthesia team. After resuscitation, the procedure was aborted. The patient was transferred to the intensive care unit (ICU) for stabilization, monitoring, and administration of vancomycin, cefepime, and metronidazole.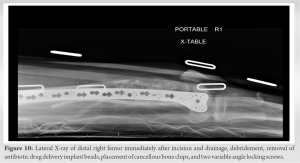
After 4 days in the ICU, the patient was brought back to the operating suite for further irrigation and debridement, removal of hardware, revision ORIF, and application of antibiotic drug delivery implant beads of the right distal femur (Fig. 7 and 8). The procedure was performed using the prior subvastus approach and the tissue was debrided of necrotic and loose tissues. The plate, screws, and Osteocrete were easily removed. Once we were satisfied with our exposure and appropriately reduced the fracture, we fixed an appropriately sized and contoured plate to the distal femur. We then mixed 40 mg PMMA simplex cement with 1 g vancomycin and 2.4 g tobramycin, forming an antibiotic bead chain of 43 balls. We placed the chain within the defect and then closed the incision. Cultures taken during the operation grew back Clostridium species. As a result, her antibiotic regimen was changed to vancomycin, cefepime, and clindamycin to reflect her culture results. She was discharged on post-operative day 5 without complication and scheduled to return in 1 week for an outpatient procedure. After 1 week, the patient underwent incision and drainage, debridement, removal of antibiotic drug delivery implant beads, placement of cancellous bone chips, and two variable angle locking screws of the right distal femur without complication (Fig. 9 and 10). Cultures taken during this operation showed no growth. The patient was discharged on penicillin and metronidazole. Follow-up appointments in the clinic showed the patient progressing with physical therapy, weight-bearing as tolerated on her right leg, and continuing long-term antibiotics and analgesia. Radiographs after 4 months showed good plate position, bone graft in situ, and progressive healing of the pathological fracture (Fig. 11 and 12).
At approximately 6 months after her last operation, the patient presented to the emergency department after a 1-week history of erythema and sinus tract drainage from her right thigh incision. The patient received an incision and drainage of her right femur abscess and application of antibiotic drug delivery implant beads (Fig. 13 and 14). The operation was uncomplicated and the patient was discharged after 1 day. Cultures taken during the operation showed no growth. At her 2-month follow-up (9 months after her initial injury), the patient was doing well, continuing long-term antibiotics managed by infectious disease, working with physical therapy, and weight bearing as tolerated on her right leg (Fig. 15 and 16).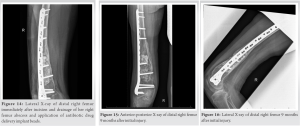
NOF is a common benign fibrogenic bone lesion that typically occurs in the 1st or 2nd decade of life affecting males more frequently than females [9,12]. The diagnosis of NOF is routinely made based on the history, physical examination, and radiographic appearance [2]. Radiographic features of NOF include distinct, sclerotic margins with an internal “bubbly” appearance [2]. Ritschl et al. classified NOFs based on their radiomorphologic features into four stages: lesions that are small, smooth, and oval without a sclerotic border (type A), polycyclic sclerotic borders (type B), partially calcified lesion with increased sclerosis (type C), and completely sclerotic lesion (type D) [5]. In a case series of 87 patients, Herget et al. reported that patients with a type A lesion had a mean age of 13 with a mean length of 21 mm [3]. Furthermore, the largest lesion reported with a pathological fracture was a 52 mm NOF, making the 17 cm lesion presented here extremely unusual [3]. NOFs are typically asymptomatic and found accidentally by radiographs for unrelated issues [8]. These lesions typically present in the lower extremities, especially around the knee [9,10,13]. Asymptomatic NOFs are followed with serial radiographs annually and they often self-resolve with increasing age [2,14]. Symptomatic NOFs typically present as pain on exertion, limping, and/or pathologic fracture [9,13]. In 23 cases of pathological fractures caused by NOFs, Arata et al. present only one fracture that occurred in a location other than the lower extremities, which substantiates the reported predisposition of NOFs for the lower extremities [9]. They concluded that lesions that exceed 50% of the bone’s transverse diameter and have a vertical length >33 mm should be monitored closely for pathologic fracture [9]. However, there is no validated method or model proven accurate enough to assess the risk of pathologic fracture for clinical use. In our case here, we present a pathologic fracture occurring in a lesion of 17 cm in size, greatly exceeding the threshold. Treatment of NOFs remains largely conservative as many have been shown to self-resolve [2,14]. Lesions that cause pain or limps have been shown to improve with curettage and the application of calcium sulfate pellets [13]. Pathologic fractures through NOFs are typically treated nonoperatively with closed reduction and cast immobilization [2,7,8]. Fractures that cannot be sufficiently reduced by closed methods can be treated with internal fixation as in this case [6,9,11]. In the reported cases of these pathologic fractures, the prognosis is good with normal fracture healing in cases treated with either non-operative or operative measures [2,9]. Reported complications after treatment include refracture, continued growth of the lesion causing pain, and physeal arrest [9].
To the best of our knowledge, this is one of the largest NOFs with a pathologic fracture reported in the literature to date. We demonstrate in this case that, even though a large NOF, the pathologic fracture can be appropriately treated with the operative methods suggested in literature – curettage, grafting, and ORIF. This case substantiates the literature that large fractures through a NOF can be appropriately managed operatively. However, orthopedic surgeons should be aware of the risks of surgery, including infection, when considering operative management of patients who present with large unstable pathologic fractures through a NOF.
A pathologic fracture through a NOF of this size is rarely reported, and this case demonstrates that operative management is a viable and appropriate method for reduction and stabilization of the fracture and opportunity for resolution of the tumor defect compared to non-operative management. The risks of surgery with large exposure should be considered.
References
- 1.Caffey J. On fibrous defects in cortical walls of growing tubular bones: Their radiologic appearance, structure, prevalence, natural course, and diagnostic significance. Adv Pediatr 1955;7:13-51. [Google Scholar | PubMed]
- 2.Betsy M, Kupersmith LM, Springfield DS. Metaphyseal fibrous defects. J Am Acad Orthop Surg 2004;12:89-95. [Google Scholar | PubMed]
- 3.Herget GW, Mauer D, Krauss T, El Tayeh A, Uhl M, Sudkamp NP, et al. Non-ossifying fibroma: Natural history with an emphasis on a stage-related growth, fracture risk and the need for follow-up. BMC Musculoskelet Disord 2016;17:147. [Google Scholar | PubMed]
- 4.Jaffe HL, Lichtenstein L. Non-osteogenic fibroma of bone. Am J Pathol 1942;18:205-21. [Google Scholar | PubMed]
- 5.Ritschl P, Karnel F, Hajek P. Fibrous metaphyseal defects--determination of their origin and natural history using a radiomorphological study. Skeletal Radiol 1988;17:8-15. [Google Scholar | PubMed]
- 6.Alshehri K, Fadil AA. Non-ossifying fibroma pathological fracture in a patient with lactose intolerance. Cureus 2021;13:e17225. [Google Scholar | PubMed]
- 7.7. Ortiz EJ, Isler MH, Navia JE, Canosa R. Pathologic fractures in children. Clin Orthop Relat Res 2005;432:116-26. [Google Scholar | PubMed]
- 8.Mankin HJ, Trahan CA, Fondren G, Mankin CJ. Non-ossifying fibroma, fibrous cortical defect and jaffe-campanacci syndrome: A biologic and clinical review. Chir Organi Mov 2009;93:1-7. [Google Scholar | PubMed]
- 9.Arata MA, Peterson HA, Dahlin DC. Pathological fractures through non-ossifying fibromas. Review of the mayo clinic experience. J Bone Joint Surg Am 1981;63:980-8. [Google Scholar | PubMed]
- 10.Sakamoto A, Arai R, Okamoto T, Matsuda S. Non-ossifying fibromas: Case series, including in uncommon upper extremity sites. World J Orthop 2017;8:561-6. [Google Scholar | PubMed]
- 11.Canavese F, Samba A, Rousset M. Pathological fractures in children: Diagnosis and treatment options. Orthop Traumatol Surg Res 2016;102:S149-59. [Google Scholar | PubMed]
- 12.Lin AJ, Siddiqui AA, Fan B, Bennett JT, Illingworth KD, Andras LM, et al. Treatments and sequelae of pediatric pathologic proximal femur fractures due to benign bone cyst. J Pediatr Orthop 2022;42:e661-6. [Google Scholar | PubMed]
- 13.Andreacchio A, Alberghina F, Testa G, Canavese F. Surgical treatment for symptomatic non-ossifying fibromas of the lower extremity with calcium sulfate grafts in skeletally immature patients. Eur J Orthop Surg Traumatol 2018;28:291-7. [Google Scholar | PubMed]
- 14.Biermann JS. Common benign lesions of bone in children and adolescents. J Pediatr Orthop 2002;22:268-73. [Google Scholar | PubMed]