This case series provides a viable treatment option for patients with distal femur fracture and pre-existing knee arthritis in a single sitting.
Dr. Sujoy Bhattacharjee, Sarvodaya Hospital Research Centre Sector 8, Sarvodaya Hospital Sector 19, Faridabad - 121 006, Haryana, India. E-mail: sujoybhattacharjeetha@gmail.com
Introduction: Intra-articular and periarticular distal femur fractures with pre-existing osteoporosis (OP) and osteoarthritis (OA) pose a significant challenge to ambulatory patients because of the higher chances of implant failure and severe disability of OA. To reduce OA-related morbidity, we advocate simultaneous total knee arthroplasty (TKA) with fracture fixation instead of fracture fixation alone using computer-assisted navigation to achieve proper ligament balance, restoration of the mechanical axis, and component alignment.
Case Report: A case series of four patients (male – 2 and females – 2) with periarticular fractures of the distal femur with severe OA and OP were primarily fixed with different modalities such as distal femur locking plates, cannulated-cancellous screw, and Herbert screw followed by computer navigation-assisted cruciate retaining TKA. All patients had Kellgren Lawrence grade ≥3 OA and underwent bilateral TKA. All patients were aggressively treated for OP using pulsed PTH therapy. Patients were found to have a faster recovery with the initiation of early partial weight bearing with crutches postoperatively in all patients, followed by unassisted weight bearing once radiological union was seen.
Conclusion: Based on satisfactory quality evidence and navigation-assisted cruciate-retaining TKA appears to be a useful treatment option for distal femoral fractures with pre-existing OA and OP. This is cost-effective and is associated with the least morbidity and excellent patient satisfaction.
Keywords: Total knee arthroplasty, distal femur fracture, osteosynthesis.
Distal femur fractures (DFFs) are relatively common in the elderly, often after a low-energy fall in association with osteoarthritis (OA), osteoporosis (OP), or any other medical comorbidities [1]. In elderly osteoporotic patients, relatively poor outcomes have been reported with open reduction and internal fixation of complex DFF [2] which depicts prolonged immobilization leads to recumbent complications and, eventually, an increase in morbidity and mortality [3]. Primary TKA has been proposed as an attractive solution that allows early weight-bearing to limit decubitus complications, knee function, and patient autonomy [4]. Wolfgang first described a single case of TKA in a patient with R.A. having a DFF. Subsequently, many authors with small series had relatively good results with TKA in DFF[5]. In this case series, we performed computer navigation-assisted bilateral total knee replacement with unilateral osteosynthesis in a single sitting, and the results were evaluated using the OXFORD KNEE score, Western Ontario and McMaster University Arthritis Index (WOMAC) score, Barthel index, range of motion (ROM), surgical time, time of union, and weight bearing.
Case 1: 53-year-old male with a medial condyle stress fracture and OA of both knees (Fig. 1 and Tables 1, 2, 3)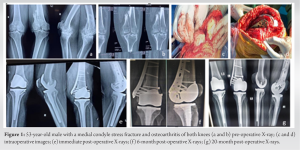
A 53-year-old male patient with a BMI of 38, obesity class 2 (WHO classification) presented with a left medial femoral condyle fracture (Orthopaedic Trauma Association [OTA] classification of 33B2). Radiography revealed Kellgren–Lawrence (KL) grade 4 OA of both knees with a pre-operative ROM of 10–70° on the right side. A standard dual X-ray absorptiometry (DEXA −2.9) scan was performed to assess bone quality. Computer navigation-assisted total knee arthroplasty (TKA) with left medial femoral condyle osteosynthesis was performed in a single sitting.
Surgical procedure
A trivector approach with curvilinear incision extension was used to expose DFF and knee without tourniquet. After exposure fracture fixation was done under C-ARM using a 4 mm distal femoral locking compression plate (DFLCP). After fracture fixation, computer navigation-assisted cruciate retaining TKA (CR-TKA) was performed followed by the opposite side. Under spinal anesthesia, the entire surgical operation took 120 min to complete. On the osteosynthesis side, a long knee brace was used following surgery. After the patient’s spinal anesthetic had worn off, isometric exercises were begun, and after 6 h, active knee movement started. With the aid of crutches, partial weight bearing was permitted after 48–72 h. Knee ROM was achieved at 90–95° after 6–10 weeks. After gaining union at 13 weeks, the patient was allowed full weight bearing on osteosynthesis side. The Barthel index showed an improvement in performance in daily living activities from 35 to 90 postoperatively. The Oxford Knee Score showed improvement from 12 preoperatively to 18 at 3 months, and 39 at 6 months follow-up. Significant improvement was evident in the range of daily activities using the WOMAC score, which was 70 preoperatively, 50 at 3 months, and 7.29 at 6 months.
Case 2: 73-year-old male with a history of falls from height (Fig. 2 and Tables 1, 2, 3)
The patient 73-year-old male with a BMI of 32, moderate obesity, class 1, presented with the right lateral femoral condyle fracture of 33B1 OTA classification. Radiological examination revealed grade 4 OA (KL Grading) with a left ROM of 90°.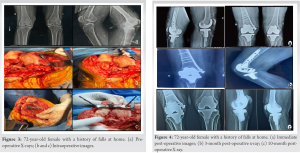
Surgical procedure
After a complete clinical assessment, the presence of any significant osteopenia or OP was assessed by DEXA scan (−2.8). DFLCP with three CC screws (4 mm) and two Herbert screws was performed under C-ARM. Total surgical time was 100 min. Subsequently, isometric exercises were initiated. Active knee movement was started within 6 h, and after 48–72 h, partial weight bearing was allowed with the help of crutches. The patient was allowed complete weight bearing at 12 weeks after achieving union. The Barthel Index score improved from 40 preoperatively to 90 at the Oxford Knee Score improved to 20 at 3 months and 38 at the 6 months follow-up. The WOMAC score analysis revealed an improvement from 92 preoperatively to 54 at 3 months and 30 at 6 months follow-up.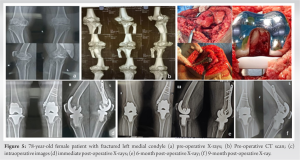
Case 3: 72-Year-Old Female with a History of Fall at Home. (Figs. 3 and 4; Tables 1, 2, 3)
A 72-year-old female with a BMI of 24 presented with the right medial femoral condyle fracture 33B2 of OTA classification. Radiological analysis revealed KL grade 4 OA on both knee joints with a ROM of 0–80° left side.
Surgical procedure
A complete clinical examination followed by a DEXA scan for any OP or osteopenia (DEXA − 3.4). The patient underwent CR-TKA with osteosynthesis of the right medial condyle fracture, with C-ARM and computer navigation assistance. The surgery time was 120 min, and the implant selected for this surgery was the proximal humerus internal locking (PHILOS) plate with CC screw. Early movement within 3–4 h, beginning with isometric exercises followed by active knee movement 6 h after recovery from spinal anesthesia. Knee flexion of 90–95° was achieved within 6–10 h postoperatively. Partial weight bearing was started within 48–72 h with the help of axillary crutches, leading to full weight bearing in 13 weeks, with a union time of 12 weeks. Postoperatively, the ROM increased from 80° to 90° at 6 weeks, 110 at 3 months, and 125° at 6 months follow-up. The score for daily activities indicated by the Barthel Index improved from 65 to 95 at 6-month follow-up. Oxford Knee score increased from 13 to 24 at 3 months and 39 at 6 months. WOMAC score was 70 preoperatively changed to 60 at 3 months and 17 at the 6 months follow-up.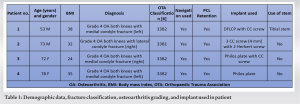
Case 4: 78-year-old female patient with a fractured left medial condyle (Fig. 5 and Tables 1-3)
The patient was a 78-year-old female with a BMI of 35, obese class 2, who presented with a left medial condyle fracture of OTA classification 33B2. Radiography revealed KL grade 4 OA in both knee joints with a ROM of 90° right side.
Surgical procedure
After a complete clinical assessment, a DEXA scan was performed to asses bone quality and which was OP (DEXA − 3.6). Following the assessment, CR-TKA with left medial condyle osteosynthesis was performed in a single sitting with navigation assistance. PHILOS plate was used as an implant without any tibial stem. The duration of surgery was 120 min. Postoperatively, early ambulatory movements with isometric exercises were performed, followed by active knee movements and partial weight bearing with axillary crutches allowed as early as 48–72 h. Full weight-bearing was allowed at 15 weeks, with a union time of 15 weeks. The improvement postoperatively was reflected by an increase in the ROM from 90° preoperatively to 100° at 3 months and 120° at 6 months follow-up. The Barthel Index at the final follow-up was 95. The Oxford Knee Score improved from 11 preoperatively to 18 at 3 months and 38 at 6 months. The WOMAC score was 100 preoperatively and 50 at 3rd month, followed by 32 at the end of the 6th month.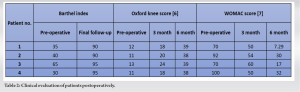
Conventionally, a patient with DFF undergoes osteosynthesis in the first sitting, followed by arthroplasty in the next sitting. A systemic review by Chen et al. states that extraarticular type-A fractures can be treated with long stem femoral components with limited need for internal fixation augmentation, but intra-articular type-B fractures may require modular or constrained prosthesis based on collateral ligament integrity and metaphyseal comminution [7]. However, in our study, we used screws (Herbert, cannulated cancellous screws) and locking plates for internal fixation without the need for a constrained TKA prosthesis [7]. Unconstrained prosthetic designs have a higher survival rate and lower rate of failure and aseptic loosening than modular and constrained prostheses in patients with distal femoral fractures and OA.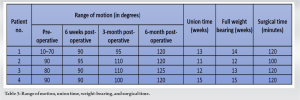
In this case series, we used an unconstrained cruciate-retaining TKA prosthesis as compared to Yoshino et al., who used posterior stabilized total knee replacement, as decreased bone cuts in CR-TKA increased stability and fixation, leading to increased survival and decreased chances of failure [8]. Choi et al. also stated in a study of eight patients that an appropriate amount of bone stock is a factor in the stability and survivorship of TKA with fixation in osteoarthritic patients with DFF [9]. The average surgical time for bilateral TKA in our study was 115 min. A computer navigation system has been used in TKA to improve the precision and accuracy of bone cuts and restoration of the mechanical axis without the need for intramedullary instrumentation [10]. Computer navigation is a beneficial technique for assisting complicated cases of TKA, such as extraarticular deformity of tibia/femur, obese patients, and patients with severe deformities, and gives excellent results in this study, as shown by improvement in Oxford Knee Score, WOMAC score, and union time. The mean range of knee flexion improvement in this study was 125 (120–130). During this case series, we inferred that a single sitting TKA with fracture fixation in elderly osteoarthritic patients who presented with a DFF is a better alternative in terms of cost, pain relief, and early ambulation [1].
Based on clinical and radiographic findings, TKA and osteosynthesis in a single sitting can be considered valid procedures for DFFs in osteoarthritic patients, as it relieve the pain and improve the patient’s functional results. Further follow-up and extensive studies should be undertaken to gain a better understanding of the procedure.
This case series demonstrates the potential benefits of utilizing computer navigation-assisted bilateral TKA with osteosynthesis in a single sitting for patients with both distal femur fracture and pre-existing knee arthritis. This approach offers a promising treatment option that can improve surgical outcomes and optimize patient recovery in complex cases.
References
- 1.Canton G, Giraldi G, Dussi M, Ratti C, Murena L. Osteoporotic distal femur fractures in the elderly: Peculiarities and treatment strategies. Acta Biomed 2019;90:25-32. [Google Scholar | PubMed]
- 2.Huang TL, Chiu FY, Chuang TY, Chen TH. The results of open reduction and internal fixation in elderly patients with severe fractures of the distal humerus: A critical analysis of the results. J Trauma 2005;58:62-9. [Google Scholar | PubMed]
- 3.Teasell R, Dittmer DK. Complications of immobilization and bed rest. Part 2: Other complications. Can Fam Physician 1993;39:1440-2, 1445-6. [Google Scholar | PubMed]
- 4.Parratte S, Ollivier M, Argenson JN. Primary total knee arthroplasty for acute fracture around the knee. Orthop Traumatol Surg Res 2018;104:S71-80. [Google Scholar | PubMed]
- 5.Wolfgang GL. Primary total knee arthroplasty for intercondylar fracture of the femur in a rheumatoid arthritic patient. A case report. Clin Orthop Relat Res 1982;171:80-2. [Google Scholar | PubMed]
- 6.Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and dislocation classification compendium-2018. J Orthop Trauma 2018;32:S1-170. [Google Scholar | PubMed]
- 7.Chen F, Li R, Lall A, Schwechter EM. Primary total knee arthroplasty for distal femur fractures: A systematic review of indications, implants, techniques, and results. Am J Orthop (Belle Mead NJ) 2017;46:E163-71. [Google Scholar | PubMed]
- 8.Yoshino N, Takai S, Watanabe Y, Fujiwara H, Ohshima Y, Hirasawa Y. Primary total knee arthroplasty for supracondylar/condylar femoral fracture in osteoarthritic knees. J Arthroplasty 2001;16:471-5. [Google Scholar | PubMed]
- 9.Choi NY, Sohn JM, Cho SG, Kim SC, In Y. Primary total knee arthroplasty for simple distal femoral fractures in elderly patients with knee osteoarthritis. Knee Surg Relat Res 2013;25:141-6. [Google Scholar | PubMed]
- 10.Bae DK, Song SJ. Computer assisted navigation in knee arthroplasty. Clin Orthop Surg 2011;3:259-67. [Google Scholar | PubMed]









