Rare presentation and correction of scoliosis in ankylosing spondylitis.
Dr. Bhushan Balvantrao Patil, Department of Spine Surgery, Sancheti Institute for Orthopedics and Rehabilitation, Pune, Maharashtra, India. E-mail: bhushancric@gmail.com
Introduction: Ankylosing spondylitis is a spondyloarthropathy that commonly involves the axial skeleton with predilection to the sacro-iliac joints and spine. The disease frequently results in a smooth globular kyphotic deformity of the spine; however, a coronal plane scoliotic deformity is extremely rare. We present a unique case of scoliotic deformity in a patient diagnosed with ankylosing spondylitis. To the best of our knowledge, following a review of the literature, this appears to be the first report of this kind.
Case Report: A 23-year-old male patient presented with chronic back pain, stiffness, and a truncal shift of the body. He had a rigid left-sided thoracolumbar curve measuring 41° with a coronal imbalance of 3.6 cm. We present a case report on scoliosis deformity correction performed with a four-level asymmetric pontes osteotomy using a bone scalpel with excellent correction of the scoliotic deformity that was well maintained at 2-year follow-up.
Conclusion: Scoliosis in ankylosing spondylitis has not been documented in literature. We report the complete correction of the deformity, which is well maintained at the 2-year follow-up.
Keywords: Ankylosing spondylitis, scoliosis, deformity, osteotomy, spine.
The term “ankylosing” is an amalgamation of two words: “ankylos,” which means stiffening of a joint, and “spondylos”, which means vertebra. It primarily affects the axial skeleton [1]. The most common terminal presentation is bony ankylosis of the sacro-iliac joints and facet joints of the spine, with a resultant bamboo spine [2]. This bamboo spine may be associated with a smooth globular kyphotic deformity that has a sagittal plane deformity with global imbalance. Isolated coronal plane deformity, i.e., scoliosis, in ankylosing spondylitis has not previously been reported, making it a unique clinical presentation [3]. We would like to share a case report on a multilevel asymmetric pontes osteotomy performed using a bone scalpel for the deformity correction.
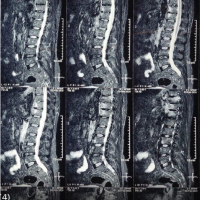
A 23-year-old male patient presented with chronic inflammatory back pain, which was associated with morning stiffness. He was diagnosed with seronegative axial spondyloarthropathy on the basis of magnetic resonance imaging (MRI) findings and a positive human leukocyte antigen B27 report [4]. He presented with deformity over the lower back, which was insidious in onset, gradually progressing, and was first noticed by the patient 5 years ago. Examination revealed rigid left-sided thoracolumbar scoliosis (Fig. 1). The left shoulder was at a higher level. The right side trunk-to-arm distance was increased. His chest expansion was 2.6 cm, and his lumbar Schober’s test was 1 cm. The lumbar range of motion was restricted. Sacroiliac joint stress tests were positive on both sides. Neurology was normal. A radiograph showed thoracolumbar scoliosis with convexity to the left side and a cobbs angle measuring 41°. (Fig. 1c and d).

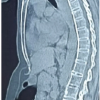
The curve was rigid, with the cobbs angle on bending films correcting to 36°. He had a coronal imbalance of 3.6 cm with an apex at the L1-L2 disc space. The X-ray showed ossification of the posterior interspinous ligament with fusion of the lumbar facet joints, showing clear characteristics of an ankylosing spondylitis appearance. (Fig. 2), a computed tomography (CT) scan of the thoracolumbar spine revealed fusion of the posterior facet joints; however, the discs were not completely ossified (Fig. 2).
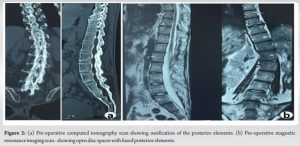
MRI showed features of sacroiliac joint fusion with no evidence of fusion at the disco-vertebral junction of the thoraco-lumbar spine. We planned a D9–L4 posterior instrumented stabilization with deformity correction. It was a rigid thoraco-lumbar curve with an apex in L1–L2 disc space. Deformity correction was done with an asymmetric pontes osteotomy at four levels, from L1 to L4 vertebra. A multilevel asymmetric pontes osteotomy was planned in view of the coronal plane deformity and flexibility of the anterior column (disc space was not ossified). After general anesthesia, the patient was positioned in a prone position. A posterior midline incision was taken, subperiosteal exposure of posterior elements was done from the upper instrumented vertebra to the lower instrumented vertebra. Bilateral pedicle screws were then placed. An asymmetric Pontes osteotomy was performed where the resection of the posterior elements on the convex side was wider than that on the concave side of the curve. (Fig. 3a) The osteotomy was done first at the apex of the curve and then at two levels below and one level above. The osteotomy was done with the aid of a bone scalpel. The bone scalpel was used to perform the osteotomy because the posterior elements of the thoracolumbar spine were completely ossified. (Fig. 3c).

The bone scalpel ensured precise bone cuts with a reduced risk of thermal and mechanical injury to dural structures. It also led to reduced osseous bleeding intraoperatively. The asymmetric pontes’ osteotomy resulted in a non-parallel resection gap, being wider on the convex side. Compression applied to the convex side resulted in a reduction of the coronal plane deformity. Two pre-contoured rods were placed, and conventional techniques of compression and distraction were applied. A reasonable on-table correction of the deformity was achieved. Decortication of the posterior elements and a bridging autograft were used to achieve posterolateral fusion. Neuromonitoring was used during the entire procedure. Drain was used post-operatively and kept for 48 h. The patient was mobilized full-weight bearing with walker support on the second post-operative day. Follow-up radiographs and clinical photos are shown in Fig. 4. The Cobb angle of the curve improved from 41° to <10° (Fig. 4c and d). The 2-year follow-up radiograph showed good maintenance of correction, which was assessed by measurement of the cobbs angle of the curve, which was maintained at 10°.

Untreated rigid scoliosis can lead to pain, truncal imbalance, progression of deformity, and daily living disability. Unlike patients with idiopathic scoliosis, patients with ankylosing spondylitis have a stiffer spine due to bony ankylosis, making the deformity correction more complicated. The most common deformity observed in ankylosing spondylitis is kyphosis. Wilkinson and Bywaters published a 15-year follow-up of 212 patients, analyzing the clinical features and deformities manifested in ankylosing spondylitis. The most common spinal deformity observed by them was thoracic and cervical kyphosis [5]. Similarly, Carette et al. published a 30-year follow-up of 51 patients studying the natural history of ankylosing spondylitis. The most common spinal deformity observed was thoracic kyphosis [2]. Thus, the scoliotic nature of this deformity makes this case report unique. The pontes osteotomy was originally described for the correction of thoracic kyphosis by a single-stage posterior column shortening for Scheuermann’s kyphosis [6]. Ponte et al. published their experience of 78 patients with thoracic hyper kyphosis [7]. Although a single-segment pontes osteotomy provides limited correction, its use at multiple segments can lead to a significant amount of deformity correction. The asymmetric pontes osteotomy results in a non-parallel resection gap with a wider gap at the convex side of the curve. Compression at the convex side of the curve leads to the closure of the osteotomy as well as the correction of the deformity [8]. The flexibility of the anterior column is a prerequisite in order for the asymmetric pontes osteotomy to work. Dynamic radiographs and CT scans can help determine the flexibility of the anterior column of the spine [7]. To minimize the risk of neurological complications, the width of the asymmetric Pontes osteotomy and the angle of the osteotomy are kept at <10 mm and 10°, respectively. There have been numerous papers describing the pontes osteotomy for the correction of sagittal imbalance. However, only a few papers have commented on the correction of the coronal balance with an asymmetric pontes osteotomy [9]. Zhang et al. evaluated the efficacy of a multi-level asymmetric pontes osteotomy for rigid adult idiopathic scoliosis. They observed significant correction in sagittal and coronal parameters with a very low complication rate [6]. Bone removal (osteotomy, facetectomy, or laminectomy) is an essential step in the Pontes osteotomy. Traditional instruments like burrs and high-speed drills produce significant vibration and torque intra-operatively. Similarly, manual osteotomies also require malletting, which increases the risk of injury to the soft tissue and neural structures. The ultrasonic scalpel allows narrow and precise bone cuts with minimum bone destruction and debris. The soft tissues have greater elastic properties than bone and can thus withstand the high amount of energy. It has a self-irrigation system, which provides lavage to wash away debris and reduces the risk of mechanical and thermal injury. Hu et al. published an initial experience of 128 patients with the use of an ultrasonic scalpel and reported that precision of bone cuts and ease of control improved the efficiency of surgery [10]. Bartley et al. used the bone scalpel for deformity correction in adolescent idiopathic scoliosis by pontes osteotomy without any anterior release. The use of a bone scalpel resulted in a significant reduction in intraoperative bleeding, with a reduction in overall blood loss of 30–40% [11].
The scoliotic nature of deformity in ankylosing spondylitis with the use of a single-stage multilevel asymmetric pontes osteotomy with an ultrasonic bone scalpel for deformity correction makes our case report unique. Such a case of scoliotic deformity correction in ankylosing spondylitis has not been documented in the literature.
Scoliosis in ankylosing spondylitis is a very rare presentation. The asymmetric pontes osteotomy can be used to treat this coronal plane deformity. The bone scalpel can be used in conditions to perform the pontes osteotomy where the posterior elements have fused due to ankylosing spondylitis. The use of an asymmetric multilevel pontes osteotomy with a bone scalpel for the correction of scoliosis in ankylosing spondylitis is reported for the 1st time through this case report.
References
- 1.Braun J, Bollow M, Remlinger G, Eggens U, Rudwaleit M, Distler A, et al. Prevalence of spondylarthropathies in HLA-B27 positive and negative blood donors. Arth Rheumatism 1998;41:58-67. [Google Scholar | PubMed]
- 2.Carette S, Graham D, Little H, Rubenstein J, Rosen P. The natural disease course of ankylosing spondylitis. Arthritis Rheum 1983;26:186-90. [Google Scholar | PubMed]
- 3.Mundwiler ML, Siddique K, Dym JM, Perri B, Johnson JP, Weisman MH. Complications of the spine in ankylosing spondylitis with a focus on deformity correction. Neurosurg Focus 2008;24:E6. [Google Scholar | PubMed]
- 4.Van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis. Arthritis Rheum 1984;27:361-8. [Google Scholar | PubMed]
- 5.Wilkinson M, Bywaters EG. Clinical features and course of ankylosing spondylitis; As seen in a follow-up of 222 hospital referred cases. Ann Rheum Dis 1958;17:209-28. [Google Scholar | PubMed]
- 6.Zhang Y, Hai Y, Tao L, Yang J, Zhou L, Yin P, et al. Posterior multiple-level asymmetrical ponte osteotomies for rigid adult idiopathic scoliosis. World Neurosurg 2019;127:e467-73. [Google Scholar | PubMed]
- 7.Ponte A, Orlando G, Siccardi GL. The true ponte osteotomy: By the one who developed it. Spine Deform 2018;6:2-11. [Google Scholar | PubMed]
- 8.Pizones J, Izquierdo E, Sánchez-Mariscal F, Álvarez P, Zúñiga L, Gómez A. Does wide posterior multiple level release improve the correction of adolescent idiopathic scoliosis curves? J Spinal Disord Tech 2010;23:e24-30. [Google Scholar | PubMed]
- 9.Halanski MA, Cassidy JA. Do multilevel ponte osteotomies in thoracic idiopathic scoliosis surgery improve curve correction and restore thoracic kyphosis? J Spinal Disord Tech 2013;26:252-5. [Google Scholar | PubMed]
- 10.Hu X, Ohnmeiss DD, Lieberman IH. Use of an ultrasonic osteotome device in spine surgery: Experience from the first 128 patients. Eur Spine J 2013;22:2845-9. [Google Scholar | PubMed]
- 11.Bartley CE, Bastrom TP, Newton PO. Blood loss reduction during surgical correction of adolescent idiopathic scoliosis utilizing an ultrasonic bone scalpel. Spine Deform 2014;2:285-90. [Google Scholar | PubMed]