In resource-limited environments, wide-awake local anesthesia surgery is a viable option for treating peri-implant humerus fractures.
Dr. Samuel Shepard, Kettering Health Grandview Medical Center, Orthopaedic Surgery Residency, Dayton, Ohio. E-mail: Samuelshepard93@gmail.com
Introduction: Over the past two decades, wide-awake local anesthesia no-tourniquet (WALANT) surgery has gained substantial popularity, challenging conventional assumptions regarding the safety of epinephrine. This report investigates the unprecedented expansion of the wide-awake local anesthesia technique beyond hand surgeries. It meticulously documents its successful application in a peri-implant proximal humerus fracture, presenting a fresh perspective on its safety and viability for managing intricate orthopedic injuries.
Case Report: The subject of this study is a 61-year-old HIV-positive male with a history of recurrent falls, seeking treatment for a peri-implant proximal humerus fracture. Electing the wide-awake local anesthesia option due to financial constraints, the patient underwent a successful surgery. The technique employed involved precise administration of local anesthetic, facilitating fracture reduction, and plate replacement. Notably, the emphasis was placed on active patient participation during intraoperative assessment.
Conclusion: This report extends the recognized utility of WALANT surgery beyond hand surgeries, demonstrating its versatility and potential transformative impact on health-care delivery. The study underscores the pivotal role played by wide-awake local anesthesia surgery in addressing challenges related to health-care accessibility. It presents a promising avenue for future orthopedic interventions and positions itself as a safe and viable option for patients in underserved areas globally.
Keywords: Humerus, open reduction internal fixation, Wide-awake local anesthesia no tourniquet
Wide-awake local anesthesia no-tourniquet (WALANT) surgery has been increasingly popular over the last two decades. The rise in popularity coincided with a publication [1] that failed to corroborate the long-standing dogma that epinephrine, when used in fingers and toes, would result in digital necrosis. A 2005 multicenter prospective study demonstrated the safety of epinephrine after presenting more than 3000 elective hand cases with no reported vasoconstriction complications [2]. Most published literature on WALANT concerns elective hand and upper extremity surgery. In a prospective study [3], over 1500 carpal tunnels were performed under WALANT using minimal sterility or field sterility across multiple centers, and only six superficial infections were reported that resolved with oral antibiotics. A randomized control trial assessing patient discomfort in WALANT carpal tunnel surgery versus local anesthetic with a tourniquet (LAWT) demonstrated patients experienced significantly more discomfort with a tourniquet than without [4]. In Addition, Gunasagaran et al. [5] reported patients treated with WALANT experienced less discomfort than those treated with LAWT. Post-operative pain control after WALANT versus other anesthetic approaches has also been widely researched in hand and upper extremity surgery. A growing body of literature has shown patients experience similar or even less post-operative pain after WALANT surgery compared to general anesthesia (GA) or LAWT with or without sedation [6-8]. For hand and upper extremity operations, WALANT surgery is a viable and safe option for eliminating unnecessary sedation, no longer subjugating patients to the pain and discomfort of a tourniquet, and is found to be equivalent in post-operative narcotic consumption. The potential to expand the scope of WALANT surgery beyond minor hand procedures holds significant promise for enhancing access to healthcare, particularly in underdeveloped countries, more so than in developed ones. A 2022, publication reiterated this, highlighting the need for more access in Brazil for elective procedures due to overall cost and lack of staff, specifically anesthetists [9]. Due to the widespread adoption of WALANT surgery in Brazil, patients can now receive treatment for a wide range of conditions, from minor hand procedures to olecranon fractures. Non-elective procedures such as distal radius fractures [10] and spaghetti wrist [11] have been performed under WALANT with similar success. Moreover, WALANT surgery for lower extremity operations such as foot and ankle injuries has been successfully reported [12-15]. Multiple publications have demonstrated wide-awake local anesthesia as a safe option for open reduction and internal fixation (ORIF) of clavicle fractures [16-18]. However, no reports have reported its use in proximal humerus surgery. Therefore, we present this report to demonstrate the usefulness and effectiveness of this technique for treating a peri-implant proximal humerus fracture.
A 61-year-old male with a history of recurrent falls and a previous left proximal humerus ORIF procedure in January 2022 following a fall on December 26, 2021, presented to an external hospital in June 2023 after experiencing a ground-level fall. On arrival, the patient was unable to raise his left arm due to severe pain. He was promptly splinted and referred for a higher level of care. The patient underwent an evaluation 3 days later, and radiographs were taken, revealing a peri-implant fracture located below the previously implanted plate at the level of the proximal humerus (Fig. 1).

On clinical examination, the patient remained incapable of actively using his arm. However, he exhibited intact neurovascular function, showed no signs of infection, and displayed well-healed wound sites from the previous ORIF procedure. The patient’s pertinent medical history includes being HIV-positive, actively receiving antiretroviral therapy, former tobacco use, and reportedly abstaining from alcohol consumption for the past 2 years. The patient was thoroughly informed about the available treatment options, associated risks, and benefits. He expressed a preference for wide-awake local anesthesia surgery over non-operative management and GA. The patient desired surgery but wished to avoid hospital admission, thus opting for wide-awake local anesthesia to prevent the need for GA. The patient admittedly also wanted a more affordable surgery. The patient was consented and booked for surgery. Wide Awake Local Anesthesia Humerus Technique. The patient was positioned supine with their arm well-supported, and manipulation was avoided until the patient received adequate anesthetic. First, to manage pain, 15 mg of ketorolac was initially administered intramuscularly. Next, the surgical assistant prepared the local anesthetic solution by combining 25 mL of lidocaine with adrenaline and 10 ml of bicarbonate, diluting the mixture to 200 mL with normal saline. The solution was then gently administered systematically, with an initial entry point in the upper arm anteriorly, followed by circumferential injections around the upper arm, along the planned anterolateral incision line (taking into account any previous scars), and into deep subcutaneous tissues approximately 8–10 cm above and below the fracture site. The periosteum and bone around the fracture site and incision line were also adequately anesthetized. The surgeon waited for 20 min between the initial injection and the first incision to allow the local anesthetic sufficient time to take effect. During the initial incision, the patient was monitored by asking for feedback, and they reported not feeling the incision. The patient’s comfort and anesthesia adequacy were actively monitored throughout the procedure, with additional local anesthetic administered as needed. An incision was made through the patient’s previous scar. Meticulously, the soft-tissue envelope was exposed and retracted until the plate and fracture were adequately visualized. The previous plate and hardware were then removed, and the fracture was reduced using a new plate and screws. Since no intraoperative imaging is presently available at the hospital, the reduction and internal fixation were carried out solely under direct visualization, depending on the expertise of the surgeon. The incision was then closed, and the patient’s neurovascular status was assessed by having the patient flex and extend his elbow as well as his wrist and digits. The total duration of the procedure was 85 min though from incision to close was only 65 min accounting for the 20-min window for the anesthetic to take effect. The patient received appropriate care and instructions postoperatively, ensuring a successful and pain-free surgical experience. The patient followed up in the clinic 4 weeks later, having no issues with a well-healed wound (Fig. 2).

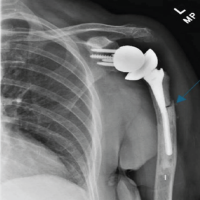
Radiographs were also obtained at that time (Fig. 3). The patient was instructed to begin physical therapy at that time. The patient was seen in the clinic at 8 weeks and 12 weeks postoperatively and was once again found to have no issues, he was progressing appropriately with his physical therapy.

The main finding from our case is the successful implantation of the wide-awake local anesthesia surgical technique for proximal humerus fracture or, more specifically, a peri-implant proximal humerus fracture. Far and away, hand surgeons have mostly implemented and accepted the WALANT surgical technique over the last decade. The benefits of the technique for standard hand procedures are well-defined. First, it allows patients to participate in intraoperative assessment, for example, during flexor tendon repairs or transfers, thus allowing physicians to assess the tension on the tendon [2]. Second, patients can avoid the risks and costs of pre-operative testing associated with undergoing GA [19]. In addition, local anesthesia administration does not require the expertise of an anesthesiologist, unlike the administration of a well-placed regional block. The WALANT technique, though mainly incorporated for typical hand procedures, has been described for distal radius fractures [10], ankle fractures [13], and clavicle fractures [17]. However, the use of WALANT in a peri-implant proximal humerus fracture has yet to be documented in the literature. In our case, the patient admittedly wanted his arm surgically fixed while incurring the least expenses. The charges for undergoing surgery with GA, plus a hospital stay, without any additional medications, is 10 times the cost of a WALANT or a wide-awake local anesthesia-only procedure in this facility. Being able to accommodate patients who are financially unable to afford GA is just one advantage of wide-awake local anesthesia surgery compared to standard GA, the most significant advantage of this technique is the increased patient care access. Far-Riera et al. [20] described being able to operate on an average of three more patients a day by implementing the WALANT technique for routine hand procedures in their hospital. Cutting the time from signing up for surgery to having surgery for standard hand procedures by half of what it was before the implementation of the technique. Specifically, though, in Dr. Aluvaala’s facility, the average number of cases daily has doubled from four to eight since implementing a full-time WALANT room. Since the publication of Lalonde et al.’s findings in 2005, WALANT surgery has empowered surgeons to explore novel frontiers [2]. This procedure enables surgeons with limited resources to achieve more and offers a viable alternative to the expensive and constrained GA. Perhaps most significantly, it is helping alleviate some of the challenges associated with accessing surgical care. Our case highlights these core benefits of wide-awake local anesthesia surgery. There are some absolute limitations to our experience that should be emphasized before applying our technique to other proximal humerus fractures. The patient must be aware of the procedure and its consequences, including the drilling background noise and the discomfort of being motionless while lying supine for a long period of time. Patient cooperation is vital, and patients should be selected carefully.
Most commonly, surgeons employ the WALANT surgical technique for minor hand procedures. This case study is the first to describe applying the wide-awake local anesthesia technique for a proximal humerus fracture, specifically a peri-implant proximal humerus fracture. Our case highlights the feasibility and success of wide-awake local anesthesia surgery in addressing more complex orthopedic scenarios, providing a cost-effective alternative for patients with financial constraints, and safely increasing accessibility to surgical care. The presented case not only underscores the economic advantages of WALANT over traditional GA but also emphasizes its role in addressing health-care disparities by enhancing access to surgical interventions, particularly in resource-limited settings. The technique’s ability to streamline surgical processes, as demonstrated by increased daily case volumes in the facility, further reinforces its potential to optimize health-care delivery. While WALANT has been previously reported for various fractures, including distal radius, ankle, and clavicle, this case represents a novel application for proximal humerus fractures, highlighting the versatility of the WALANT, or wide-awake local anesthesia-only surgical technique.
This article demonstrates the successful application of the wide-awake local anesthesia surgical technique for treating a peri-implant proximal humerus fracture. The case emphasizes the feasibility and success of using wide-awake local anesthesia in more complex orthopedic scenarios in resource-limited regions. It highlights its cost-effectiveness potential to address health-care disparities and streamline surgical processes, thereby enhancing access to surgical interventions in resource-limited settings.
References
- 1.Denkler K. Comprehensive review of epinephrine in the finger: To do or not to do. Plast Reconstr Surg 2001;108:114. [Google Scholar | PubMed]
- 2.Lalonde D, Bell M, Benoit P, Sparkes G, Denkler K, Chang P. A multicenter prospective study of 3,110 consecutive cases of elective epinephrine use in the fingers and hand: The Dalhousie Project clinical phase. J Hand Surg Am 2005;30:1061-7. [Google Scholar | PubMed]
- 3.Leblanc MR, Lalonde DH, Thoma A, Bell M, Wells N, Allen M, et al. Is main operating room sterility really necessary in carpal tunnel surgery? A multicenter prospective study of minor procedure room field sterility surgery. Hand (N Y) 2011;6:60-3. [Google Scholar | PubMed]
- 4.Saleh E, Saleh J, Govshievich A, Ferland-Caron G, Lin JC, Tremblay DM. Comparing minor hand procedures performed with or without the use of a tourniquet: A randomized controlled trial. Plast Reconstr Surg Glob Open 2021;9:e3513. [Google Scholar | PubMed]
- 5.Gunasagaran J, Sean ES, Shivdas S, Amir S, Ahmad TS. Perceived comfort during minor hand surgeries with wide awake local anaesthesia no tourniquet (WALANT) versus local anaesthesia (LA)/tourniquet. J Orthop Surg (Hong Kong) 2017;25:2309499017739499. [Google Scholar | PubMed]
- 6.Miller A, Kim N, Ilyas AM. Prospective evaluation of opioid consumption following hand surgery performed wide awake versus with sedation. Hand (N Y) 2017;12:606-9. [Google Scholar | PubMed]
- 7.Dar QA, Avoricani A, Rompala A, Levy KH, Shah NV, Choueka D, et al. WALANT hand surgery does not require postoperative opioid pain management. Plast Reconstr Surg 2021;148:121-30. [Google Scholar | PubMed]
- 8.Aultman H, Roth CA, Curran J, Angeles J, Mass D, Wolf JM, et al. Prospective evaluation of surgical and anesthetic technique of carpal tunnel release in an orthopedic practice. J Hand Surg Am 2021;46:69.e1-7. [Google Scholar | PubMed]
- 9.Ribak S, Folberg CR, André de Oliveira Alves J. The Brazilian perspective of WALANT in fracture fixation from the hand to the elbow. J Hand Surg Glob Online 2022;4:471-6. [Google Scholar | PubMed]
- 10.Huang YC, Hsu CJ, Renn JH, Lin KC, Yang SW, Tarng YW, et al. WALANT for distal radius fracture: Open reduction with plating fixation via wide-awake local anesthesia with no tourniquet. J Orthop Surg Res 2018;13:195. [Google Scholar | PubMed]
- 11.Arik HO, Coskun T, Kose O. Management of spaghetti wrist under WALANT technique. Hand Surg Rehabil 2021;40:655-9. [Google Scholar | PubMed]
- 12.Bilgetekin YG, Kuzucu Y, Öztürk A, Yüksel S, Atilla HA, Ersan Ö. The use of the wide-awake local anesthesia no tourniquet technique in foot and ankle injuries. Foot Ankle Surg 2021;27:535-8. [Google Scholar | PubMed]
- 13.Li YS, Chen CY, Lin KC, Tarng YW, Hsu CJ, Chang WN. Open reduction and internal fixation of ankle fracture using wide-awake local anaesthesia no tourniquet technique. Injury 2019;50:990-4. [Google Scholar | PubMed]
- 14.Poggetti A, Del Chiaro A, Nicastro M, Parchi P, Piolanti N, Scaglione M. A local anesthesia without tourniquet for distal fibula hardware removal after open reduction and internal fixation: The safe use of epinephrine in the foot. A randomized clinical study. J Biol Regul Homeost Agents 2018;32:57-63. [Google Scholar | PubMed]
- 15.Bajuri MY, Saidfudin NS, Mazli N, Azriq NA, Azemi AF. Safety of wide-awake local anesthesia with no tourniquet (WALANT) in for lower limb surgery: A potential alternative in times of emergency. Front Surg 2022;9:848422. [Google Scholar | PubMed]
- 16.Kafiabadi MJ, Sabaghzadeh A, Biglari F, Sadighi M, Ebrahimpour A. Effects of fixation of clavicle fracture using wide-awake local anesthesia no tourniquet (WALANT) technique on intra-operative bleeding volume, surgical duration, and post-operatively visual analog scale (VAS); A case series study. Injury 2023;54:557-60. [Google Scholar | PubMed]
- 17.Ahmad AA, Ubaidah Mustapa Kamal MA, Ruslan SR, Abdullah S, Ahmad AR. Plating of clavicle fracture using the wide-awake technique. J Shoulder Elbow Surg 2020;29:2319-25. [Google Scholar | PubMed]
- 18.Niempoog S, Tanariyakul Y, Jaroenporn W. Wide-awake local anesthesia for clavicle fracture fixation: A case report. Int J Surg Case Rep 2021;79:112-5. [Google Scholar | PubMed]
- 19.Lalonde DH. Ten questions about wide awake local anaesthesia no tourniquet (WALANT) surgery. J Hand Surg Asian Pac Vol 2022;27:219-25. [Google Scholar | PubMed]
- 20.Far-Riera AM, Perez-Uribarri C, Serrano MJ, González JM. Impact of WALANT hand surgery in a secondary care hospital in Spain. Benefits to the patient and the health system. J Hand Surg Glob Online 2023;5:73-9. [Google Scholar | PubMed]