To understand mechanisms, radiographic findings, and available treatments for hip avulsion injuries.
Dr. Giulia D’Amone, Department of Radiology, Fondazione Policlinico Universitario Campus Bio-Medico di Roma, Roma, Italy. E-mail: damonegiulia@gmail.com
Introduction: Pelvic apophyseal avulsion fractures are uncommon injuries that frequently affect adolescents while participating in sports. This occurs because the enthesis cannot withstand the tractional force applied because the apophysis has not yet fully fused. Due to its complex muscular structure, being the origin of several muscles that cross two lower extremity joints, the pelvis has an increased risk for such injuries. The diagnosis of pelvic avulsion injuries depends heavily on imaging. The best way to detect soft-tissue changes, including tendon or muscle strain, bone marrow edema, hematomas, and soft tissue avulsion injuries, is with an magnetic resonance imaging . It is also the best at showing tendon retraction and can help the clinician spot patients who might benefit from surgical treatment.
Case Report: We report six cases of adolescents professional footballers that suffered avulsion injuries while playing football. The patients had painfully restricted hip range of motion and were unable to bear weight. Some of them on physical examination felt pain at the palpation of the injured area. Magnetic resonance revealed apophysis growth plate avulsion with or without displaced bone fragments that were treated conservatively with an excellent clinical and radiological outcome.
Conclusion: For an accurate diagnosis of pelvic avulsion injuries and clinical management, it is important that everyone caring for this patient population is aware of the common injury mechanisms, radiographic findings, and available treatments.
Keywords: Musculoskeletal radiology, pelvis, musculotendinous junction, avulsion, enthesis, apophysis.
Pelvic avulsion fractures of the apophysis are a particular injury that affects kids and teenagers. Enthesis or apophysis avulsion injuries can result in a wide variety of pathologies, ranging from a single tendon or ligamentous insertional strain at the attachment site to a complete apophysis or bone fragment displacement along with an avulsion fracture. In terms of anatomy, the term “enthesis” refers to the location of a tendon or ligament’s insertion and the nearby tissues that are connected to it functionally [1]. It plays crucial roles in stress reduction, smooth movement, and in the transfer of force between different tissue media and can be classified as direct and indirect, as well as fibrous and fibrocartilaginous [2,3]. Apophyses are secondary ossification sites that affect the size, shape, but not the length, of the bones [4]. As the weakest part of the muscle-tendon-bone complex, the apophyses are more prone to avulsion fractures as a result of abrupt eccentric contractions of attached muscle groups. For proper management of these injuries, clinicians must have in-depth knowledge of the muscle groups and their attachments to the individual apophyses due to the wide variety of presentations.
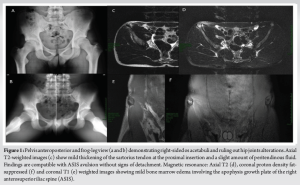
Case 1
Pelvis anteroposterior (AP) and frog-leg view (a and b) demonstrating right-sided os acetabuli and ruling out hip joints alterations. Magnetic resonance: Axial T2 (d), coronal proton density fat-suppressed (f) and coronal T1 (e) weighted images showing mild bone marrow edema involving the apophysis growth plate of the right anterosuperior iliac spine (ASIS). Axial T2-weighted images (c) show mild thickening of the sartorius tendon at the proximal insertion and a slight amount of peritendinous fluid. Findings are compatible with ASIS avulsion without signs of detachment. ASIS avulsion injury is relatively common and represents about 28% of all pelvic avulsion injuries. Sprinters or jumpers are typical athletes at risk for this type of injury that occurs during forceful extension and sudden sprain of the hip [5] (Fig. 1).
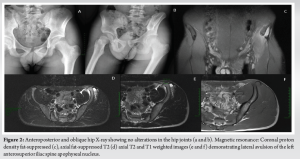
Case 2
AP and oblique hip X-ray showed no alterations in the hip joints (a and b). Magnetic resonance: Coronal proton density fat-suppressed (c), axial fat-suppressed T2 (d) axial T2 and T1 weighted images (e and f) demonstrating lateral avulsion of the left ASIS apophyseal nucleus with an estimated diastasis of 1.2 cm. Modest adjacent fluid is visible (Fig. 2).
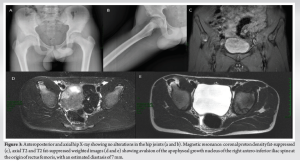
Case 3
AP and axial hip X-ray showed no alterations in the hip joints (a and b). Magnetic resonance: Coronal proton density fat-suppressed (c), axial T2 and T2 fat-suppressed weighted images (e and d) showing avulsion of the apophyseal growth nucleus of the right anteroinferior iliac spine (AIIS) at the origin of rectus femoris, with an estimated diastasis of 7 mm. Modest peripheral fluid share and fluid imbibition of the right iliac muscle was visible. AIIS avulsion injuries account for about 20–25% of all pelvic avulsion injuries. The rectus femoris muscle extends the leg at the knee and flexes the hip joint. A forceful hip extension can result in a strain of this specific muscle or an avulsion injury of the AIIS. These injuries are frequent in sports like soccer and can happen during sprinting, jumping, or kicking [5] (Fig. 3).
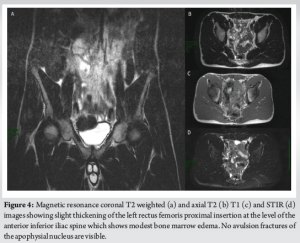
Case 4
Magnetic resonance coronal T2 weighted (a) and axial T2 (b) T1 (C) and STIR (d) images showed slight thickening of the left rectus femoris proximal insertion at the level of the AIIS which shows modest bone marrow edema. No avulsion fractures of the apophysial nucleus are visible (Fig. 4).
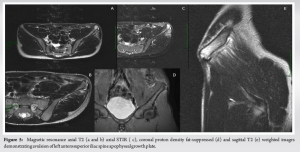
Case 5
Magnetic resonance axial T2 (a and b) axial STIR (c), coronal proton density fat-suppressed (d), and sagittal T2 (e) weighted images demonstrating avulsion of left ASIS apophyseal growth plate. Modest thickening of the sartorius tendon proximal insertion is visible (Fig. 5).
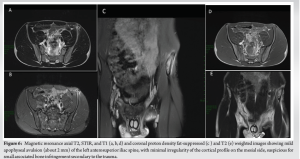
Case 6
Magnetic resonance axial T2, STIR, and T1 (a, b, c) and coronal proton density fat-suppressed (d) and T2 (e) weighted images showing mild apophyseal avulsion (about 2 mm) of the left ASIS, with minimal irregularity of the cortical profile on the mesial side, suspicious for small associated bone infringement secondary to the trauma. Mild bone marrow edema of the left iliac crest (IC) (Fig. 6).
The most frequently injured apophyses are the rectus femoris insertion at the AIIS, the hamstrings insertion at the ischial tuberosity, the sartorius insertion at the ASIS, the tensor fasciae latae insertion on the IC, the iliopsoas insertion on the lesser trochanter, or the rectus abdominis insertion at the superior corner of the pubic symphysis [6,7]. Sprinting, kicking, and tennis are frequently mentioned as mechanisms of injury [8-10]. Diagnosing pelvic avulsion injuries requires a lot of imaging. Conventional radiographs, which help in defining the osseous separation of apophyses or bone fragments, are the primary diagnostic tool in traumatic pelvic injuries but can be of limited value because of tissue overlap. Typical trauma histories, clinical examinations, and results from standard radiographs are frequently enough, without the need for additional imaging, for diagnosis. Computed tomography (CT) and magnetic resonance imaging (MRI) allow a better evaluation of anatomical details. The preferred method for confirming the presence of a dislocated ossified apophysis or bone fragment CT, which can also reveal the degree of callus formation or heterotopic ossification as a result of long-lasting or recent avulsion injuries. On the other hand, MRI is the most effective at displaying soft-tissue changes such as tendon or muscle strain, hematoma, edema of the bone marrow, and soft-tissue avulsion injuries. In addition, it works best for illustrating tendon retraction and can help the clinician find patients who might benefit from surgical treatment. If a pelvic or hip avulsion injury is suspected, it is frequently advantageous to begin with an axial or coronal PD/T2-weighted sequence with fat saturation and a wide field of view (maximum 40 cm, at least 5–6-mm slice thickness, 256 x 256 matrix) including the entire pelvis as a bilateral survey. The following sequences should be acquired with a small field of view if the injury site can be quickly identified (max. 16–24 cm) with imaging of either just one hamstring/adductor origin, or both. T1 weighting without fat saturation should be used for at least one sequence. The best option might be coronal T1. Additional PD or intermediate weighted sequences in the appropriate orientations (axial, sagittal, and coronal) for the injury site should be run. Non-fat-suppressed T2-weighted images might also be advantageous. Unilateral sequences ought to provide as much anatomical detail as possible; it is recommended to use a small field of view with a high in-plane resolution (at least 1.0 mm 1.0 mm in-plane) and through plane resolution (maximum 3.5-mm slice thickness). In the acute setting, ultrasound is also a great tool for showing avulsion injuries, but it heavily depends on the sonographer’s skill and frequently cannot show the anatomical relationship of the injuries. There are no established treatment recommendations in the literature for avulsion fractures but the vast majority of injuries has responded well to non-operative treatment, which includes analgesics, restricted activity, and partial weight bearing while using crutches for at least 3–6 weeks [10-13]. Surgery should be considered as a treatment option in these cases with significant fragment displacement (>15 mm) and in patients with a high functional demand. In addition, authors increasingly suggest surgical treatment for apophyseal fractures as a result of these encouraging results [14-17]. In summary, patients who receive surgical treatment (open reduction and screw fixation) recover faster and resume their normal activities faster. Conservative therapy may result in non-union or heterotopic ossifications as potential complications. These could lead to chronic pain at the location of the fracture as well as a markedly reduced capacity to perform sports. Despite this, surgical management carries a risk of restricted movement, keloid scarring, prolonged wound healing, skin irritation, and irritability of metal work, which could cause patients abandon their sports activity. We support an informed, patient-centered approach. choosing which treatments are most effective, and reserving surgery for those who have a related articular condition.
Adolescent athletes frequently suffer apophyseal avulsion injuries around the hip and pelvis. To ensure appropriate and prompt recognition and management, it is important that everyone caring for this patient population is aware of the common mechanisms, radiographic findings, and available treatments.
Appropriate and prompt recognition and management of apophyseal avulsion injuries, frequently suffered from adolescent athletes, is important for everyone caring for these patients, from radiologists to orthopaedic surgeons.
References
- 1.Benjamin M, McGonagle D. The anatomical basis for disease localisation in seronegative spondyloarthropathy at entheses and related sites. J Anat 2001;199:503-26. [Google Scholar | PubMed]
- 2.Shaw HM, Benjamin M. Structure-function relationships of entheses in relation to mechanical load and exercise. Scand J Med Sci Sports 2007;17:303-15. [Google Scholar | PubMed]
- 3.Benjamin M, Toumi H, Ralphs JR, Bydder G, Best TM, Milz S. Where tendons and ligaments meet bone: Attachment sites (‘entheses’) in relation to exercise and/or mechanical load. J Anat 2006;208:471-90. [Google Scholar | PubMed]
- 4.Kjellin I, Stadnick ME, Awh MH. Orthopaedic magnetic resonance imaging challenge: Apophyseal avulsions at the pelvis. Sports Health 2010;2:247-51. [Google Scholar | PubMed]
- 5.Albtoush OM, Bani-Issa J, Zitzelsberger T, Springer F. Avulsion injuries of the pelvis and hip. Rofo 2020;192:431-40. [Google Scholar | PubMed]
- 6.McKinney BI, Nelson C, Carrion W. Apophyseal avulsion fractures of the hip and pelvis. Orthopedics 2009;32:42. [Google Scholar | PubMed]
- 7.Coulier B. Acute avulsion of the iliac crest apophysis in an adolescent indoor soccer. J Belg Soc Radiol 2015;99:20-4. [Google Scholar | PubMed]
- 8.Casabianca L, Rousseau R, Loriaut P, Massein A, Mirouse G, Gerometta A, et al. Iliac crest avulsion fracture in a young sprinter. Case Rep Orthop 2015;2015:302503. [Google Scholar | PubMed]
- 9.Chan C, Sohail MZ, Buddhdev P. Case report of combined iliac crest and ASIS apophysis avulsion fracture in an adolescent footballer. J Surg Case Rep 2021;2021:rjab573. [Google Scholar | PubMed]
- 10.Metzmaker JN, Pappas AM. Avulsion fractures of the pelvis. Am J Sports Med 1985;13:349-58. [Google Scholar | PubMed]
- 11.Serbest S, Tosun HB, Tiftikçi U, Oktas B, Kesgin E. Anterior inferior iliac spine avulsion fracture: A series of 5 cases. Medicine (Baltimore) 2015;94:e562. [Google Scholar | PubMed]
- 12.Uzun M, Alpan B, Özger H. Avulsion fractures involving the straight and reflected heads of the rectus femoris. Hip Int 2014;24:206-9. [Google Scholar | PubMed]
- 13.Linni K, Mayr J, Höllwarth ME. Apophyseal fractures of the pelvis and trochanter minor in 20 adolescents and 2 young children. Unfallchirurg 2000;103:961-4. [Google Scholar | PubMed]
- 14.Schuett DJ, Bomar JD, Pennock AT. Pelvic apophyseal avulsion fractures: A retrospective review of 228 cases. J Pediatr Orthop 2015;35:617-23. [Google Scholar | PubMed]
- 15.Pogliacomi F, Calderazzi F, Paterlini M, Ceccarelli F. Surgical treatment of anterior iliac spines fractures: Our experience. Acta Biomed 2014;85:52-8. [Google Scholar | PubMed]
- 16.Kautzner J, Trc T, Havlas V. Comparison of conservative against surgical treatment of anterior-superior iliac spine avulsion fractures in children and adolescents. Int Orthop 2014;38:1495-8. [Google Scholar | PubMed]
- 17.Kosanović M, Brilej D, Komadina R, Buhanec B, Pilih IA, Vlaović M. Operative treatment of avulsion fractures of the anterior superior iliac spine according to the tension band principle. Arch Orthop Trauma Surg 2002;122:421-3. [Google Scholar | PubMed]











