Risk of rapidly progressive hip osteoarthritis after an intra-articular injection is heightened due to chondrotoxicity and patient health factors.
Dr. Justin Turcotte, Anne Arundel Medical Center, 2000 Medical Parkway, Suite 503, Annapolis, Maryland 21401, United States. E-mail: jturcotte@aahs.org
Introduction: Rapidly progressive hip osteoarthritis (OA) leading to femoral head collapse (FHC) following intra-articular (IA) corticosteroid injections is a perplexing variant of OA. We explored eight cases of chronic joint pain treated with IA corticosteroid injections. Subsequently, they experienced swift deterioration of the femoral head integrity within as little as 10 weeks. These cases underscore the need for a comprehensive assessment of risk factors versus benefits in this patient population.
Case Report: The study reveals a complex interplay between comorbidities, treatments, and outcomes. Patients exhibited various health factors, including obesity, smoking history, cancer treatment, and deficiencies in Vitamin D levels, which have been found to increase the risk of FHC. Furthermore, the study explores the chondrotoxicity of corticosteroids and local anesthetics used in IA injections. In vitro studies show complete loss of chondrocyte viability after a single dose of corticosteroids, potentially leading to cartilage degradation. In addition, local anesthetics may induce cellular demise and structural alterations in the articular cartilage. These factors highlight various influences affecting treatment outcomes in patients with OA.
Conclusion: In conclusion, this case series highlights the rare adverse outcome of rapidly progressive hip OA and FHC following IA corticosteroid injections and possible risk factors. While a definitive etiology remains unclear, the study provides valuable conclusions to aid in future treatment decision-making.
Keywords: Rapidly progressive hip osteoarthritis, intra-articular injections, corticosteroid injections, femoral head collapse.
Osteoarthritis (OA) is a common joint disorder, affecting millions worldwide with its hallmark destruction of joint cartilage and underlying bone matrix. However, within this landscape of degeneration, rapidly progressive osteoarthritis of the hip (RPOH) leading to femoral head collapse (FHC) has emerged as a perplexing variant characterized by accelerated erosion of joint integrity with limited studies exploring its etiology [1]. RPOH is marked by chondrolysis exceeding 2 mm within a year in the absence of osteonecrosis, neuropathy, infection, or inflammatory conditions [2]. Yet, the origins of RPOH remain debatable, with various studies looking at factors such as demographics, comorbidities, alcohol abuse, smoking, radiation therapy, and intra-articular (IA) corticosteroid toxicity [3]. However, with limited literature, the risk factors for FHC remain not well-defined. IA injections, a common OA management intervention, serve as pain relief and diagnostic tools. However, they raise concerns about unintended consequences, potentially fueling the progression of RPOH [3]. Notably, as much as 40% of rapid hip OA cases have been suspected to be linked to the usage of corticosteroids [4]. Yet, there is limited literature and reported cases of rapid OA and collapse of the femoral head after an IA injection. Within this context, we present an account of eight occurrences of destructive FHC ensuing after a temporally related IA corticosteroid with local analgesic injection at our facility. We explore the clinical manifestations, explore potential triggers, and dissect controversies surrounding IA interventions and their ramifications.
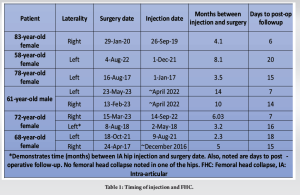
We present a series of eight cases involving patients aged 58–83 years old who presented with varying degrees of joint pain and dysfunction. All patients had a history of chronic joint issues, primarily OA, and had previously received conservative management, including physical therapy and oral medications. Due to persistent symptoms, they were referred for IA corticosteroid injections administered by either an orthopedic surgeon, physical medicine physician, anesthesiologist, radiologist, or physician assistant. Patients received either betamethasone or triamcinolone steroid mixed with either 1% lidocaine or bupivacaine. Injections were imaged guided by the use of an ultrasound or fluoroscopy. Initially, the injected patients reported transient pain alleviation, aligning with the anticipated outcomes of corticosteroid therapy. However, within a remarkably brief period post-injection, these individuals encountered a swift deterioration in joint function, accompanied by heightened pain and constrained range of motion (Table 1). Diagnostic imaging uncovered indications of accelerated progression of OA, characterized by significant femoral head sphericity loss. Subsequent consultations with orthopedic specialists confirmed FHC and underscored the necessity for surgical intervention involving total hip replacement to address the advanced joint damage and mitigate the pain.
This patient cohort exhibited an array of pertinent comorbidities and medical backgrounds. Each patient’s body mass index (BMI) fell within the overweight or obese classification. Among the group, five out of seven patients had a substantial history of smoking. One patient had undergone treatment for anal carcinoma with intravenous chemotherapy. In addition, patients reported instances of Vitamin D deficiencies, hypothyroidism, and diabetes, underscoring the complexity of factors influencing their treatment outcomes.
This study reported eight cases of rapidly progressive OA resulting in FHC. Patients initially presented with hip pain and OA, which deteriorated rapidly into severe femoral head failure requiring surgery in as little as 10 weeks (Fig. 1) following an IA corticosteroid with local analgesic injection. Notably, this patient cohort exhibited a range of comorbidities, including obesity, a smoking history, prior cancer treatment, and deficiencies in Vitamin D levels. This convergence of factors underscores the complex interplay between treatment outcomes and individual health circumstances, warranting a comprehensive assessment of risk factors and potential benefits prior to initiating such interventions.

IA corticosteroid therapy has been a longstanding method to alleviate joint inflammation and pain. Its effectiveness in relieving symptoms associated with OA, structural issues, and inflammatory conditions is well-established. Nevertheless, this therapy has raised worries about possible negative impacts on joint cartilage. Research has shown the influence of corticosteroids on the well-being of cartilage, revealing a total decline in the viability of chondrocytes and compromised integrity of the cartilage itself [5]. Notably, in vitro studies revealed complete loss of chondrocyte and synoviocyte viability after a single dose of betamethasone, methylprednisolone, or triamcinolone, potentially leading to cartilage degradation and compromised integrity [6]. These results show fast cell destruction, which may play a role in the integrity of the hip joint. While information is still limited concerning the damaging effects on the cartilage in IA injections for the hip, the chondrotoxicity of local anesthetics utilized in these injections has also been suggested [6-8]. This could potentially lead to cellular demise and structural alterations in the articular cartilage, leading to osteonecrosis and/or collapse of the bone matrix. Research suggests that their application could induce cell death and structural changes in the articular cartilage in a matter of weeks [8]. Recent in vitro research by Mwale et al. in 2023 found that bupivacaine, levobupivacaine, and ropivacaine triggered apoptosis, as indicated by increased caspase-3 activity, within 24 h of induction of the drug [9]. Properly evaluating the balance between short-term pain relief benefits and potential long-term cartilage risks is essential when considering what combination of IA injections to utilize. One patient within the cohort underwent injections in both hips, but a notable distinction emerged in terms of the ensuing outcomes (Fig. 2). Rapid OA leading to FHC manifested unilaterally, presenting an intriguing contrast. The divergent factor lay in the choice of local anesthetic used (Table 2). Both hips received triamcinolone corticosteroid injections in combination with a local anesthetic. Specifically, the right hip received treatment with bupivacaine and exhibited FHC 6 months later (Fig. 2a and b). Conversely, the left hip, treated with lidocaine, showed no indications of FHC (Fig. 2c and d). Studies have shown that both bupivacaine and lidocaine are more chondrotoxic than others [10]. However, Farkas et al. discovered in their in vitro studies that 0.5% bupivacaine was more toxic than 1% lidocaine. Bupivacaine induced almost 100% cell necrosis after 24 h of exposure to human chondrocytes [11]. This leads to the need for caution when determining the type of IA injection to use.

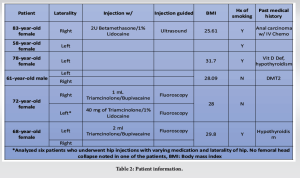
The observed patient cohort presented a diverse range of relevant comorbidities and individual medical histories, warranting a comprehensive consideration of their impact on treatment outcomes. Each patient’s BMI was categorized as overweight or obese, a factor that has been shown to correlate with joint-related issues and treatment responses [12]. Kelly et al. found that patients who developed FHC after IA injection had higher mean BMIs [1]. The presence of such weight-related factors could potentially contribute to the progression of joint degeneration. Within this cohort, a notable portion of patients, five out of seven, had a significant smoking history. Smoking has been associated with adverse effects on joint health, including impaired wound healing and compromised circulation, which could conceivably influence the healing process post-injection [13]. Careful history-taking and attention should be given to this patient population. Furthermore, the history of malignancy and the subsequent chemotherapy in one patient adds a layer of complexity. Chemotherapy agents can impact various bodily systems, potentially affecting the joint environment and responses to treatment. One study found that patients who developed FHC after IA injection had a higher percentage history of cancer therapy (14.3% vs. 6.1%, P = 0.012) [1]. Radiation and chemotherapy are linked to bone and muscle damage, loss, and increased fracture risk [14]. Cautious consideration should be given to this patient population when determining treatment. Moreover, reported instances of Vitamin D deficiencies, hypothyroidism, and diabetes highlight the interconnected nature of systemic health and joint well-being. These underlying medical conditions have been shown to influence bone health and the progression of OA. Vitamin D deficiency, for instance, could potentially impact cartilage integrity and the overall health of the joint [1,15]. Finally, we must rule out infective causes of this rapid joint destruction. This patient cohort had an average of under two weeks to postoperative follow-up, with no signs of infections noted and no reoperation due to infectious etiologies. Collectively, the interplay of these multifaceted health factors underscores the intricate web of influences affecting treatment outcomes in this patient cohort. It is essential to acknowledge the limitations of this case series, including the absence of a control group and the relatively small sample size. Nevertheless, these cases emphasize the need for clinicians to carefully weigh the potential benefits against the risks of such interventions and explore alternative treatment options for individuals with certain risk factors.
The cases presented in this report highlight a rare but concerning adverse outcome of rapid OA progression and FHC following IA corticosteroid injections. While a definitive etiology of rapid OA with FHC is unclear, we have drawn potential conclusions that can help in future treatment decision-making.
Rapid OA is a difficult pathway of OA to understand as it may have a multifaceted etiology. Our study highlights important risk factors that may lead down this path of rapid FHC and can be used to manage this patient population.
References
- 1.Kelly BJ, Williams BR, Gravely AA, Schwanz K, Sechriest VF 2nd. Femoral head collapse after hip intra-articular corticosteroid injection: An institutional response to improve practice and increase patient safety. PLoS One 2021;16:e0259242. [Google Scholar | PubMed]
- 2.Yasuda T, Matsunaga K, Hashimura T, Tsukamoto Y, Sueyoshi T, Ota S, et al. Characterization of rapidly progressive osteoarthritis of the hip in its early stage. Eur J Rheumatol 2020;7:130-4. [Google Scholar | PubMed]
- 3.Sanguino RA, Sood V, Santiago KA, Cheng J, Casey E, Mintz D, et al. Prevalence of rapidly progressive osteoarthritis of the hip following intra-articular steroid injections. PM R 2023;15:259-64. [Google Scholar | PubMed]
- 4.Ahmed AF, Hammad M, Salameh M, Ahmed GO. Destructive osteonecrosis of the femoral head after a single intra-articular corticosteroid injection: A report of two cases. Int J Surg Case Rep 2020;77:711-5. [Google Scholar | PubMed]
- 5.Wernecke C, Braun HJ, Dragoo JL. The effect of intra-articular corticosteroids on articular cartilage: A systematic review. Orthop J Sports Med 2015;3(5). [Google Scholar | PubMed]
- 6.Sherman SL, Khazai RS, James CH, Stoker AM, Flood DL, Cook JL. In vitro toxicity of local anesthetics and corticosteroids on chondrocyte and synoviocyte viability and metabolism. Cartilage 2015;6:233-40. . [Google Scholar | PubMed]
- 7.Jayaram P, Kennedy DJ, Yeh P, Dragoo J. Chondrotoxic effects of local anesthetics on human knee articular cartilage: A systematic review. PM R 2019;11:379-400. [Google Scholar | PubMed]
- 8.Asan CY, Agyuz G, Canpolat DG, Demirbas AE, Asan M, Yay A, et al. Chondrotoxic effects of intra-articular injection of local anaesthetics in the rabbit temporomandibular joint. Int J Oral Maxillofac Surg 2022;51:1337-44. [Google Scholar | PubMed]
- 9.Mwale C, Sunaga T, Wang Y, Bwalya EC, Wijekoon HM, Kim S, et al. In vitro chondrotoxicity of bupivacaine, levobupivacaine and ropivacaine and their effects on caspase activity in cultured canine articular chondrocytes. J Vet Med Sci 2023;85:515-22. [Google Scholar | PubMed]
- 10.Kreuz PC, Steinwachs M, Angele P. Single-dose local anesthetics exhibit a type-, dose-, and time-dependent chondrotoxic effect on chondrocytes and cartilage: A systematic review of the current literature. Knee Surg Sports Traumatol Arthrosc 2018;26:819-30. [Google Scholar | PubMed]
- 11.Farkas B, Kvell K, Czömpöly T, Illés T, Bárdos T. Increased chondrocyte death after steroid and local anesthetic combination. Clin Orthop Relat Res 2010;468:3112-20. [Google Scholar | PubMed]
- 12.Reyes C, Leyland KM, Peat G, Cooper C, Arden NK, Prieto-Alhambra D. Association between overweight and obesity and risk of clinically diagnosed knee, hip, and hand osteoarthritis: A population-based cohort study. Arthritis Rheumatol 2016;68:1869-75. [Google Scholar | PubMed]
- 13.Vicaş RM, Bodog FD, Ciursaş AN, Fugaru OF, Grosu F, Lazăr L, et al. Aseptic necrosis of femoral head-clinical study. Curr Health Sci J 2021;47:228-36. [Google Scholar | PubMed]
- 14.Sturgeon KM, Mathis KM, Rogers CJ, Schmitz KH, Waning DL. Cancer-and chemotherapy-induced musculoskeletal degradation. JBMR Plus 2019;3:e10187. [Google Scholar | PubMed]
- 15.Mabey T, Honsawek S. Role of vitamin D in osteoarthritis: Molecular, cellular, and clinical perspectives. Int J Endocrinol 2015;2015:383918. [Google Scholar | PubMed]