Non-traumatic bilateral femur neck fracture in young patients can be the first presentation of an underlying chronic systemic disease.
Dr. Raghad A Ramadan, School of Medicine, The University of Jordan, Amman 11942, Jordan. E-mail: ramadan.raghad@yahoo.com
Introduction: Spontaneous femur neck fracture is rare, especially when they occur bilaterally. Renal osteodystrophy is among the causes of these fractures that should be kept in mind. We report a case of a young female who presented with bilateral hip pain and was found to have bilateral femur neck fracture due to renal osteodystrophy. This was the first presentation of an undiagnosed end-stage kidney disease. This case report aims to highlight the importance of investigating the cause of these rare fractures in young patients and discuss available surgical options.
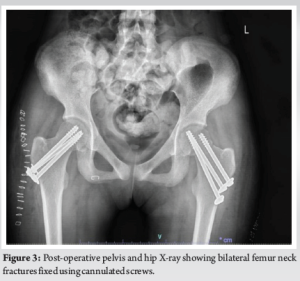
Case Report: A 19-year-old female presented complaining of bilateral hip pain. On physical examination, there was tenderness on palpation of both thighs. Her workup was significant for anemia, a high level of creatinine, hypocalcemia, elevated alkaline phosphatase, and parathyroid hormone. A pelvis radiograph showed bilateral femur neck fracture. Considering her very young age, the metabolic derangements she had and to avoid exposing her to a major surgery, we treated her fractures by fixation using three cannulated screws on each side. We aimed to report this case as it is an unusual presentation of a previously undetected stage 5 chronic kidney disease (CKD) in a very young patient.
Conclusion: Renal osteodystrophy due to CKD can present with spontaneous bilateral femur neck fracture. Physicians should have a high index of suspicion for this condition not to miss a chronic disease with multiple sequelae. Furthermore, these fractures carry a high risk of complications and mortality, so they should be addressed promptly.
Keywords: Renal osteodystrophy, chronic kidney failure, bilateral femur neck fracture.
Fractures occurring in the femoral neck of adults under the age of 50 make up around 2–3% of all femur neck fractures [1,2], primarily resulting from high-energy impacts [1,3]. Spontaneous bilateral femoral neck fractures are exceedingly rare and usually linked to metabolic conditions such as renal osteodystrophy, osteomalacia, and osteoporosis [4,5]. These fractures are at increased risk of developing adverse outcomes such as malunion, non-union, and avascular necrosis [6,7]. There is limited literature available on such cases. Here, we present a case of a 19-year-old female patient who presented with bilateral hip pain, unmasking atraumatic bilateral femur neck fracture, which led to the diagnosis of end-stage kidney disease.
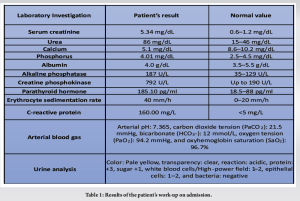
A 19-year-old single female patient was transferred to our hospital with a 2-day history of left hip pain. The pain was so severe that any movement of her hip would result in severe pain, and she was not able to bear weight or walk. A few days before, her family noticed that she developed a slight limping, but they did not seek any help as they though it could be due to a muscular cause. Her left hip pain was sudden in onset, spastic in nature, not radiating, exacerbated by any movement. It was continuous and lasted for about 2 h followed by the development of the same pain in her right hip. This was the first time she experienced this. She denied any history of trauma, falls, current nausea, vomiting, pruritus, metallic taste, dysuria, hematuria, diarrhea, constipation, abdominal pain, weakness, back pain, fever, chills, cough, muscle spasm, peri-oral numbness, photophobia, skin rash, oral ulcers, joint pain or swelling, chest pain, shortness of breath, or weight loss. No history of seizures, smoking, or steroid use. Her family history was significant for a 27-year-old aunt who has chronic kidney disease (CKD). She denies any family history of autoimmune diseases. Her medical history was significant for anemia and Vitamin D deficiency in the past 5 years and she was not compliant to the treatment. On physical examination, she was awake, alert and in pain. There was tenderness to palpation in both thighs. Lower-limb pulses were intact bilaterally, there was no lower limb edema, no hotness or discoloration, no swelling, and no joint tenderness. Sensation was intact. Power and reflexes were difficult to assess due to muscle pain. Negative Chvostek’s and Trousseau’s signs. No periorbital edema or facial rash. Her work-up was significant for anemia, elevated serum creatinine which was 5.34 mg/dL (N: 0.6–1.2 mg/dL), hypocalcemia, and elevated parathyroid hormone. She also had elevated alkaline phosphatase (ALP), creatine phosphokinase (CPK), erythrocyte sedimentation rate, and C-reactive protein (CRP). Furthermore, her arterial blood gas (ABG) showed metabolic acidosis on presentation. Results of her investigations are shown in Table 1.
Renal ultrasound was done showing an atrophied echogenic right kidney and a small left kidney. No hydronephrosis was present bilaterally. Her pelvis and femur X-ray (Fig. 1) showed bilateral Garden 4 femur neck fractures.

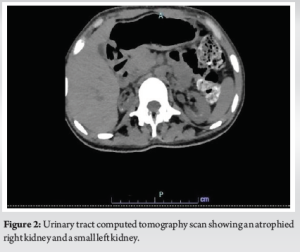
Urinary tract computed tomography (UTCT) scan showed an atrophied right kidney with cortical thinning, along with a small left kidney and deep cortical calcifications in both kidneys (Fig. 2).
Her fractures were repaired surgically 3 days following her admission after the stabilization of her medical condition. The patient’s management involved performing basic laboratory investigations, sending a blood crossmatch, and administering analgesia. These steps are crucial for ensuring proper care and treatment. The operation was done under general anesthesia. Starting at the left side, closed reduction, and fixation were done. Three cannulated screws were inserted inferiorly, anterosuperiorly, and posterosuperiorly. On the right side, it was difficult to achieve reduction in a closed manner, so open reduction and internal fixation were achieved through an anterior approach and three cannulated screws were inserted (Fig. 3). The surgery went uneventful. The patient is comfortable in bed. She is under investigation for a definitive diagnosis of her stage 5 CKD. Furthermore, she is planned for dialysis and a possible kidney transplant.
Despite the rarity of atraumatic bilateral femur neck fractures, known causes of this phenomenon include seizure activity, electrical shock, altered bone metabolism, or abnormal anatomy [5,8-18]. Several studies have documented seizure attacks or electrical injuries as contributors to this type of fracture [8,9]. The proposed mechanism suggests that strong muscle spasms during a seizure attack may lead to fractures, as demonstrated in Finelli and Cardi study [19]. Abnormal anatomy can also be a factor in bilateral stress fractures of the neck of femur. An example is provided in the case report by Annan and Buxton, where the abnormal length and more varus position of the femoral neck placed additional stress on it [12]. Multiple papers have reported bilateral neck of femur fractures secondary to altered bone metabolism, whether due to osteoporosis [10], Vitamin D deficiency [11], or as a part of renal osteodystrophy [5, 13-18]. Renal osteodystrophy can be histologically classified into high- or low-turnover states, with the predominant mechanism being the high-turnover state [20]. The primary cause is secondary hyperparathyroidism, attributed to multiple factors, including phosphate retention, hypocalcemia, Vitamin D deficiency, and low fibroblast growth factor 23 [20]. The prevalent outcome of this high turnover state is the osteitis fibrosa pattern. Conversely, the low turnover state is associated with developing osteomalacia and adynamic bone disease [20]. Various studies have reported spontaneous bilateral neck of femur fractures attributed to renal osteodystrophy, leading to bone weakening [5,13-18]. Other research indicates that renal osteodystrophy, in association with uremic or hypocalcemic-induced seizures, may be the cause [21]. John et al. reported three cases of end-stage renal disease patients on hemodialysis sustaining bilateral neck of femur fractures following uremic or hypocalcemic-induced seizures [21]. In our case, the patient had hypocalcemia and secondary hyperparathyroidism, but there was no history of seizures and the patient denied experiencing any uremic symptoms. This strongly supports the conclusion that our patient’s fracture is mostly explained by renal osteodystrophy alone, without a concomitant hypocalcemia-induced seizure or uremia. Karapinar et al. reported a case of a 23-year-old male known to have CKD as a consequence of myelomeningocele complications. He presented similar to our case with bilateral hip pain [13]. Another case reported by Sathyanarayana et al. had a different presentation. The patient was a 23-year-old male with CKD and reflux nephropathy who was hospitalized for complaints of dysuria, pyuria, and loss of appetite. During his stay in the hospital, he suffered from inability to move his lower limbs. At first, they attributed his weakness to a hypocalcemia-induced seizure, but his bilateral hip pain persisted despite treating his hypocalcemia. Following that, a pelvis radiograph was done which showed vertical subcapital fractures of bilateral neck of femur. His work-up results were similar to our case including hypocalcemia, elevated ALP, and hyperparathyroidism [5]. Interestingly, our case had an elevated CPK, which is not typically elevated in this situation without generalized muscle weakness. Elevated levels of CPK are typically associated with a range of causes outside the neuromuscular realm. These include endocrine disorders, metabolic disturbances, the impact of certain medications, and malignancies. They usually present with muscle weakness or myalgia [22]. A pelvis X-ray was the first imaging investigation done in our case and the two cases mentioned above to investigate bilateral hip pain [5,13]. Karapinar et al. also reported the use of pelvis computed tomography, dual-energy X-ray absorptiometry scan of the lumbar spine and hips in addition to abdominal ultrasound compared to our case where we did a UTCT and a renal ultrasound in addition to pelvis X-ray [13]. While arthroplasty was the surgical procedure done in the two cases mentioned above, we chose to treat our patient using fixation [5,13]. Considering the very young age of our patient and her metabolic derangements, we favored not to expose her for a major surgery. In contrast, cemented total hip arthroplasty and bilateral uncemented modular bipolar hemiarthroplasty were the two surgeries done in the cases reported by Karapinar et al. and Sathyanarayana et al., respectively [5,13]. In the latter case, they explained choosing arthroplasty as the fracture had a high risk of avascular necrosis. In addition, internal fixation would carry a poor prognosis as the patient had osteoporosis secondary to renal osteodystrophy [5]. In the management of hip fractures among individuals with renal failure, conservative care might initially seem like a safer and more cautious approach for these vulnerable patients. However, Schaab et al. reported a study where they found that surgical intervention is superior to the conservative approach [23]. This study included 11 cases of femoral neck fractures in 11 patients with renal osteodystrophy receiving chronic dialysis, seven of whom underwent surgery. They compared the outcomes between operative and conservative treatments. They concluded that operative management exhibited better outcomes in terms of complications and mortality rates in patients with femur neck fractures who have advanced renal osteodystrophy in addition to different medical problems and on chronic dialysis. However, these fractures occurred in older individuals with an average dialysis dependency of 9.2 years, indicating severe CKD, a prerequisite for such injuries, unlike our case which was not diagnosed with CKD before her presentation [23]. The significance of renal osteodystrophy as the cause of bilateral neck of femur fractures lies in the higher risk of nonunion found in patients with CKD, even in acutely and adequately treated cases, due to secondary bone changes [24]. In addition, the combination of hip fracture and renal failure is associated with high mortality [25]. There is limited data on the mortality of such cases in the younger age group as our patient. However, Klein et al. reported a 38% mortality rate within the 1st-year post-surgical treatment of hip fractures in renal failure patients. This study encompassed nine fractures in eight patients averaging 63 years old; six were dependent on dialysis, and two had functioning renal transplants. Three patients passed away within a year after the operation due to reasons unrelated to the surgery [25]. In light of these statistics, it is crucial to acknowledge the challenges that hip fractures in CKD patients, like the case at hand, pose for surgeons. The complexity of treatment involves considerations of various patient factors, different surgical techniques, comprehensive care involving multiple specialties, and post-operative support. In our case, spontaneous simultaneous bilateral femoral neck fracture was the first presentation of an undiagnosed stage 5 CKD in a 19-year-old patient, which is an unusual presentation occurring in a very young patient. Therefore, we aimed to report this unique case to emphasize the importance of systematically investigating the root cause of clinical presentations among physicians, which may reveal a chronic problem that remained hidden for years.
Non-traumatic bilateral femur neck fracture can occur in younger patients and present significant challenges for surgeons. Physicians should maintain a high index of suspicion for these cases due to their intricate diagnosis and management. Collaborative consultation with a multidisciplinary team for reaching a diagnosis in addition to providing sufficient perioperative care proves essential and impactful. Early detection followed by prompt surgical intervention could lead to more favorable recovery outcomes considering the high risk of complications and mortality these fractures carry in renal failure patients.
End-stage kidney disease can present late with spontaneous bilateral femur neck fracture, especially in young patients. The diagnosis and management of such cases are challenging. This case report sheds the light on the importance of having awareness of this possible unusual presentation of CKD among physicians, which will help to address these patients adequately.
References
- 1.Robinson CM, Court-Brown CM, McQueen MM, Christie J. Hip fractures in adults younger than 50 years of age. Epidemiology and results. Clin Orthop Relat Res 1995;312:238-46. [Google Scholar | PubMed]
- 2.Zetterberg C, Elmerson S, Andersson GB. Epidemiology of hip fractures in Göteborg, Sweden, 1940-1983. Clin Orthop Relat Res 1984;191:43-52. [Google Scholar | PubMed]
- 3.Protzman RR, Burkhalter WE. Femoral-neck fractures in young adults. J Bone Joint Surg Am 1976;58:689-95. [Google Scholar | PubMed]
- 4.Vijayvargiya M, Shetty V, Makwana K, Agarwal N. Bilateral simultaneous neck femur fracture following domestic fall in an elderly patient: A rare case report. Rev Bras Ortop 2017;52:363-5. [Google Scholar | PubMed]
- 5.Sathyanarayana V, Patel MT, Raghavan S, Naresh D. Simultaneous bilateral femur neck fracture in a young adult with chronic renal failure-a case report and review of literature. J Orthop Case Rep 2015;5:24-6. [Google Scholar | PubMed]
- 6.Slobogean GP, Sprague SA, Scott T, Bhandari M. Complications following young femoral neck fractures. Injury 2015;46:484-91. [Google Scholar | PubMed]
- 7.Stockton DJ, O’Hara LM, O’Hara NN, Lefaivre KA, O’Brien PJ, Slobogean GP. High rate of reoperation and conversion to total hip arthroplasty after internal fixation of young femoral neck fractures: A population-based study of 796 patients. Acta Orthop 2019;90:21-5. [Google Scholar | PubMed]
- 8.Shah HM, Grover A, Gadi D, Sudarshan K. Bilateral neck femur fracture following a generalized seizure-a rare case report. Arch Bone Jt Surg 2014;2:255-7. [Google Scholar | PubMed]
- 9.Nekkanti S, Vijay C, Theja JS, RaviShankar R, Raj S. An unusual case of simultaneous bilateral neck of femur fracture following electrocution injury-a case report and review of literature. J Orthop Case Rep 2016;6:70-2. [Google Scholar | PubMed]
- 10.Arisumi S, Mawatari T, Ikemura S, Matsui G, Iguchi T, Mitsuyasu H. Spontaneous bilateral femoral neck fractures in a young male adult: A case report and literature review. BMC Musculoskelet Disord 2019;20:449. [Google Scholar | PubMed]
- 11.Maramreddy LV, Mittal R, Anand A, Vatsya P. Bilateral nonunion of femoral neck fractures because of nutritional osteomalacia: A report of 2 cases. JBJS Case Connect 2022;12(4):e22.00314. [Google Scholar | PubMed]
- 12.Annan IH, Buxton RA. Bilateral stress fractures of the femoral neck associated with abnormal anatomy--a case report. Injury 1986;17:164-6. [Google Scholar | PubMed]
- 13.Karapinar H, Ozdemir M, Akyol S, Ulkü O. Spontaneous bilateral femoral neck fractures in a young adult with chronic renal failure. Acta Orthop Belg 2003;69:82-5. [Google Scholar | PubMed]
- 14.Zhu Y, Hu J, Han W, Lu J, Zeng Y. Simultaneous bilateral femoral neck fractures in a dialysis-dependent patient: Case report and literature review. BMC Musculoskelet Disord 2020;21:242. [Google Scholar | PubMed]
- 15.Kumar PA, Vupputuri A, Naidu MC, Gollangi S, Boddapalli UK. Spontaneous simultaneous bilateral femoral neck fracture secondary to renal osteodystrophy: A case report and review of literature. J Evol Med Dent Sci 2014;3:3484. [Google Scholar | PubMed]
- 16.Devkota P, Ahmad S. Bilateral impacted femoral neck fracture in a renal disease patient. Niger Med J 2013;54:354-5. [Google Scholar | PubMed]
- 17.Rednah D, Brinji OS, Aldakhil M, Alshareef E, Alshehri M. Surgical challenge in the management of spontaneous, bilateral, nontraumatic, neglected femoral neck fractures in a patient with end-stage renal disease: A case report and literature review. Cureus 2023;15:e38633. [Google Scholar | PubMed]
- 18.Hung KH, Lee CT, Gau YL, Chen JB. Neglected bilateral femoral neck fractures in a patient with end-stage renal disease before chronic dialysis. Ren Fail 2001;23:827-31. [Google Scholar | PubMed]
- 19.Finelli PF, Cardi JK. Seizure as a cause of fracture. Neurology 1989;39:858-60. [Google Scholar | PubMed]
- 20.Shah A, Aeddula NR. Renal osteodystrophy. In: StatPearls. Treasure Island, FL: StatPearls; 2023. [Google Scholar | PubMed]
- 21.John R, Kumar P, Aggarwal S, Rajnish RK, Agarwal S, Vatsyan K. Simultaneous, non-traumatic, bilateral neck femur fractures in uremic renal osteodystrophy: A report of three cases and literature review. J Orthop Case Rep 2018;8:90-4. [Google Scholar | PubMed]
- 22.Moghadam-Kia S, Oddis CV, Aggarwal R. Approach to asymptomatic creatine kinase elevation. Cleve Clin J Med 2016;83:37-42. [Google Scholar | PubMed]
- 23.Schaab PC, Murphy G, Tzamaloukas AH, Hays MB, Merlin TL, Eisenberg B, et al. Femoral neck fractures in patients receiving long-term dialysis. Clin Orthop Relat Res 1990;260:224-31. [Google Scholar | PubMed]
- 24.Kalra S, McBryde CW, Lawrence T. Intracapsular hip fractures in end-stage renal failure. Injury 2006;37:175-84. [Google Scholar | PubMed]
- 25.Klein DM, Tornetta P 3rd, Barbera C, Neuman D. Operative treatment of hip fractures in patients with renal failure. Clin Orthop Relat Res 1998;350:174-8. [Google Scholar | PubMed]











