Speed Bridge repair of tendoachilles in cases where surgical removal of Haglund exostosis is required allows faster rehabilitation as compared to other methods due to its inherent robust construct.
Dr. Shakti Swaroop, Department of Orthopedics, Institute of Medical Sciences, Siksha ‘O’ Anusandhan Deemed to be University, Ground Floor, Sum Hospital Road, Shampur, Bhubaneswar, Odisha 751003, India. E-mail: shaktiswaroop@soa.in.ac
Introduction: Retrocalcaneal pain in late adulthood and athletes has been attributed to insertional Achilles tendinosis (IAT). Another presentation of IAT is a degenerative Achilles tear, which can be partial or complete. Symptomatic patients with failed conservative management are treated by debridement and repair of the Achilles tendon. Often, they need augmentation with a tendon transfer. The flexor hallucis longus (FHL) is the most commonly used tendon for augmentation. The Speed Bridge technique to repair the degenerated tendoachilles tear gives better pullout strength and provides a larger surface area of contact between the bone and tendon.
Case Report: We included 12 patients with symptomatic degenerative Achilles tears repaired with the Speed Bridge technique and FHL augmentation. Post-operatively, all patients were allowed active ankle mobilization on day 1 and were allowed weight bearing as tolerated in an airwalker shoe. All patients went through an accelerated rehabilitation protocol. Pre-operative and post-operative American Orthopedic Foot and Ankle Hindfoot Score (AOFAS) and Visual Analog Scale (VAS) scores were compared for all the patients.
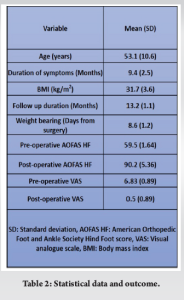
Conclusion: The mean age was 58.1 (range 50–68) years. The mean follow-up period was 13.1 (range 12–15) months. The mean pre- and post-operative AOFAS score at 12 months was 59.5 (range 58–71) and 90.2 (range 87–100), respectively. The mean pre-operative VAS for pain was 6.8 (range 6–8), and the mean post-operative VAS score was 0.5 (range 0–2). The mean interval to weight bearing was 8.4 days (range 7–10) days. Our study indicates that accelerated early rehabilitation and an early return to active life are possible with the Speed Bridge technique and FHL augmentation in degenerative Achilles tears. The mean post-operative AOFAS scores were comparable to other studies, but early return to activity, minimal need for immobilization, and accelerated rehabilitation were the advantages of the Speed Bridge technique in the repair of degenerative Achilles tears.
Keywords: Haglund deformity, degenerative Achilles tendinosis, speed bridge repair
Insertional Achilles tendinopathy (IAT) is a common occurrence among the active population [1]. In an epidemiologic investigation of 1394 nonathletes, Achilles tendinopathy was found in 5.6% of the subjects (4% insertional, 3.6% non-insertional, and 1.9% both forms) [2]. Haglund syndrome, described by Patrick Haglund in 1928, is a painful posterosuperior deformity of the heel of uncertain etiology. Haglund syndrome includes retrocalcaneal bursitis, Achilles tendon calcification, and Haglund deformity of the posterior superior calcaneus [3]. Various modalities of non-operative treatment have been mentioned for IAT in the literature; however, conservative treatment is tried for no longer than 6 months [4]. Operative management includes the removal of the degenerated tendon, pathological bursae, and removal of the bony growth from the calcaneum. The central incision with the tendon splitting approach gives adequate exposure to debride the pathological tendon and the Haglund deformity with good results [5,6]. After debridement of the pathological tendon, its reattachment to the calcaneum is mandatory. Soft bone anchors give us a very convenient and robust method of reattachment, even with complete or near-complete detachment of the Achilles tendon [7]. The suture bridge technique with knotless bone anchors for reattachment of Achilles tendon was first described by Witt et al. in four patients with good results after complete detachment of the TA [8]. Double-row repair has been proven biomechanically in insertional tendinopathy [9,10]. We describe a novel technique of reattachment of the Achilles tendon by the Speed Bridge SystemTM (Arthrex, Naples, FL) using knotless anchors with a crossing pattern of fiber tapes. Considering the lack of published literature for this technique of Achilles tendon repair in Haglund syndrome, our aim in this study is to present the functional outcome of speed bridge repair by comparing pre-operative and post-operative American Orthopedic Foot and Ankle Society (AOFAS) Hindfoot score (AOFAS HF) and secondary outcomes of comparison of pre-operative and post-operative VAS score for pain and note the complications of the procedure.
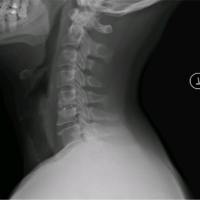
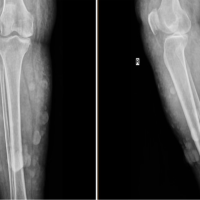
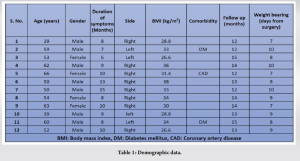
Twelve patients with retrocalcaneal pain who had failed conservative management for more than 6 months were evaluated clinically in a tertiary care center by a foot and ankle expert and further investigated. The radiological evaluation was done with standing radiographs and an MRI to evaluate the bony and Achilles tendon pathology. The degeneration of the tendon with the Haglund deformity was noted, and consent was taken for the central tendon splitting approach for the excision of the retrocalcaneal spur along with tendon debridement and repair with the speed bridge technique. A retrospective case series was done to evaluate the functional outcome and visual analog scale (VAS) score for pain and compare them preoperatively and postoperatively with a minimum of 12 months of follow-up. The patients included in the study were aged from July 2020 to October 2021. The patient record sheets were accessed, and data were collected as per the pro forma.
Data were collected from 12 patients retrospectively and was organized. Demographic data and comorbidities were noted (Table 1). The pre-operative AOFAS HF and VAS scores were noted, and the post-operative AOFAS hindfoot score and VAS score of patients with a minimum follow-up of 12 months were noted and entered in a Microsoft Excel sheet. The data were analyzed by a Student’s t-test (SPSS version 21, IBM, Armonk, NY, USA) to find the statistical significance (P < 0.05) between the mean pre-operative and mean post-operative scores of the AOFAS HF and VAS scores.
All surgical procedures were done by the senior foot and ankle surgeon. Under spinal anesthesia, a tourniquet was applied to the thigh. Prone position and roll the sheet under the distal leg. Midline tendon splitting incision is given to raise flaps at level of paratenon for about 8 cm from the superior edge of the posterior surface of the calcaneum. Mark the transverse line of insertion of the Achilles if it is found intact. Split Achilles tendon, extending not more than 5 cm proximal to its insertion, in the substance of the Achilles. Preserve attached corners if an incomplete tear occur. Raise the two split parts of the tendon and debride the degenerated part and review the plan for flexor hallucis longus (FHL) transfer excise Haglund tubercle with a saw and osteotome. Check tendon length, reaching up to the middle third of the posterior surface of the calcaneum. If not, plan a FHL transfer. Mark 2 rows about 20 mm apart for anchors: the proximal row in the proximal third and the distal row in the middle third of the posterior surface of the calcaneum. The central part should be able to accommodate a 6–7 mm interference screw for FHL insertion (if more than 50% of the tendon is lost after debridement). Drill directional K wires 1.5 mm thick at all 4 points and a beath pin for FHL. Hole drilled up to 6 mm for FHL insertion. FHL was harvested, whiplash sutures passed, thickness confirmed, and tendon passed through a hole drilled and held with an interference screw while the foot was held in neutral. 3.5-mm holes are made for anchors. Anchors loaded with fire tape (2 mm) and fiber wire no. 2 passed in proximal row. Fiber tape and wire passed 1.5 cm proximal to distal end of Achilles from anterior to posterior and tendon pulled with these to bring close to insertion point. The crossing pattern of tape is now inserted in the distal row with anchors to maintain appropriate tension. The fiber wire is brought out 1 cm proximal to the fiber tape and tightened to increase the surface area of the Achilles foot print on the posterior surface of the calcaneum. The wound was closed in layers, including the healthy paratenon, and a sterile padded dressing was done up to below the knee. Paratenon in these long-standing IATs is usually degenerated and not amenable to repair; however, whatever paratenon is left should be repaired.
Retrospectively, 12 patients were included in the study who had a complete follow-up of minimum 12 months. The mean pre-operative AOFAS HF score was 59.5 (SD = 1.64) and the mean post-operative AOFAS HF score was 90.2 (SD = 5.36). The pre-operative mean VAS score was 6.83 (SD = 0.89) and the post-operative mean VAS score was 0.5 (SD = 0.89). Details are in Table 2. Weight bearing was allowed for a mean of 8.6 days (SD = 1.2). Complications were noted in two patients, one with a superficial infection at the wound site that subsided with antibiotics, and one patient complained of persistent pain with a VAS score of 2. FHL transfer was done for four patients. Standard analgesics of aceclofenac 100 mg and paracetamol 325 mg tablets were given for 2 days for 2 weeks to these patients. However, patients who complained of longer duration pain were treated with sos analgesics.
Surgical management of IAT with partial degenerative Achilles tears and Haglund deformities is warranted when conservative methods have failed for more than 6 months [4]. Surgical excision of the Haglund deformity, debridement of the pathological Achilles tendon, and retrocalcaneal bursa are part of the procedure to achieve pain-free rehabilitation [6]. The central tendon splitting approach has been described as giving excellent exposure for the debridement of the Achilles tendon and the excision of the Haglund deformity [3,6,11,12]. Also, the central tendon splitting approach does not have a risk of injury to the sural nerve and limits damage to the blood supply [6].
FHL transfer was done for patients in whom more than 50% of the Achilles tendon was debrided, as advocated by Cottom et al. [13]. Kolodziej et al. in their cadaveric biomechanical study, concluded that up to 50% of the Achilles tendon can be debrided safely [14].
Double-row suture bridge repair
Double-row repair with bone anchors has been proven to be biomechanically better with a larger surface area of contact between bone and tendon [9,10,15]. Our technique to repair the Achilles tendon was a double row repair with bone anchors and fiber tape, which probably gives a stronger contact of the tendon to the bone over a larger surface area.
Fiber tape advantages
In a few biomechanical studies, tapes have been found to be stiffer and stronger than sutures, with a greater ultimate failure load [16,17]. Liu et al. reported that the tape provided a three-fold increase in the footprint contact pressure and a one and a half-fold increase in construct strength compared with the suture in a biomechanical study [18]. This is where our technique differs from suture bridge technique, as we are using tapes to cinch the tendon to the bone surface and probably gain the advantage of having a greater ultimate strength to failure and higher footprint contact pressure as compared to Suture Bridge. Furthermore, bone anchors give us the advantage of allowing early weight-bearing [19].
Early weight bearing and comparison to other studies
Thus, this technique, which combines the advantages of double row anchor and tape augmentation, gives us the confidence to start early weight bearing in the air walker boot as compared to the suture bridge technique. Weight bearing was allowed early in our series, as early as 7-day post-surgery. A study by Rigby et al. used suture bridges for reattachment of Achilles tendon after a central tendon splitting approach for Haglund disease and reported good outcomes after allowing early weight bearing with a mean of 10 (0–43) days from the day of surgery but also delayed weight bearing to 4 weeks in elderly, obese, and participants with FHL augmentation [20]. The range varied from 0 to 43 days, and their group of patients included 20 out of 43 participants who were athletes compared to our participants, who were mostly elderly. This may suggest that the speed bridge technique gives a better sense of security to the surgeon by allowing early weight bearing. However, this does need further evaluation in long-term comparative studies with a larger sample size. The air walker boot may be another helpful factor in allowing early weight bearing as it alleviates the need for the heel strike and toe off phases of the gait cycle due to its inherent rocker bottom design. Furthermore, it helps in early rehabilitation, as early mobilization prevents muscle atrophy. Other studies reporting the outcome of the suture bridge technique in Achilles tendon reattachment have reported allowing full weight bearing at 4 weeks from the day of surgery [5,12].
Final scores with other studies of suture bridge
Final AOFAS HF scores were compared to studies that have used Suture Bridge for a central tendon splitting approach. Rigby et al. reported a mean post-operative AOFAS HF score of 90 after a mean follow-up of 24 months in their series of 43 patients [20]. Post-operative AOFAS HF scores of 87 and 92 were reported by Gillis et al. and Güler et al. in their series of 9 and 24 patients [5,12]. We achieved a similar mean AOFAS HF score of 90.1 (SD = 5.36) in our series of 12 patients at a mean follow-up period of 13.2 (SD = 1.1) months. However, in our study, the patients were allowed early weight bearing as compared to other studies, which could be of clinical significance and may make the Speed Bridge technique a better procedure to reattach the Achilles tendon. This also needs further investigation in comparative analysis with a larger sample size.
An early rehabilitation and return to active life are possible with the Speed Bridge technique for Achilles tendon reattachment when using the central tendon splitting approach for surgical management of IAT. Excellent functional results with good pain relief were achieved by this technique in our study. The Speed Bridge technique using the central tendon splitting approach has not been mentioned in the literature with a follow-up of more than a year in the management of degenerative Achilles tendinopathy.
Very early rehabilitation is possible in cases where the tendo Achilles is split for the excision of the Haglund by a novel technique of reattaching the tendon called speed bridge repair. Speed bridge is a double-row repair with fiber tapes that substantially increases the surface area of contact of the tendon to the bone.
References
- 1.Li HY, Hua YH. Achilles tendinopathy: Current concepts about the basic science and clinical treatments. Biomed Res Int 2016;2016:6492597. [Google Scholar | PubMed]
- 2.Waldecker U, Hofmann G, Drewitz S. Epidemiologic investigation of 1394 feet: Coincidence of hindfoot malalignment and Achilles tendon disorders. Foot Ankle Surg 2012;18:119-23. [Google Scholar | PubMed]
- 3.DeOrio MJ, Easley ME. Surgical strategies: Insertional Achilles tendinopathy. Foot Ankle Int 2008;29:542-50. [Google Scholar | PubMed]
- 4.Irwin TA. Current concepts review: Insertional Achilles tendinopathy. Foot Ankle Int 2010;31:933-9. [Google Scholar | PubMed]
- 5.Gillis CT, Lin JS. Use of a central splitting approach and near complete detachment for insertional calcific Achilles tendinopathy repaired with an Achilles bridging suture. J Foot Ankle Surg 2016;55:235-9. [Google Scholar | PubMed]
- 6.Johnson KW, Zalavras C, Thordarson DB. Surgical management of insertional calcific Achilles tendinosis with a central tendon splitting approach. Foot Ankle Int 2006;27:245-50. [Google Scholar | PubMed]
- 7.Wagner E, Gould JS, Kneidel M, Fleisig GS, Fowler R. Technique and results of Achilles tendon detachment and reconstruction for insertional Achilles tendinosis. Foot Ankle Int 2006;27:677-84. [Google Scholar | PubMed]
- 8.Witt BL, Hyer CF. Achilles tendon reattachment after surgical treatment of insertional tendinosis using the suture bridge technique: A case series. J Foot Ankle Surg 2012;51:487-93. [Google Scholar | PubMed]
- 9.Jiang Y, Li Y, Tao T, Li W, Zhang K, Gui J, et al. The double-row suture technique: A better option for the treatment of Haglund Syndrome. Biomed Res Int 2016;2016:1895948. [Google Scholar | PubMed]
- 10.Beitzel K, Mazzocca AD, Obopilwe E, Boyle JW, McWilliam J, Rincon L, et al. Biomechanical properties of double- and single-row suture anchor repair for surgical treatment of insertional Achilles tendinopathy. Am J Sports Med 2013;41:1642-8. [Google Scholar | PubMed]
- 11.McGarvey W, Palumbo R, Baxter D, Leibman B. Insertional Achilles tendinosis: Surgical treatment through a central tendon splitting approach. Foot Ankle Int 2002;23:19-25. [Google Scholar | PubMed]
- 12.Güler Y, Birinci M, Hakyemez OS, Buyukdogan K, Çaçan MA, Arslanoglu F, et al. Achilles tendon-splitting approach and double-row suture anchor repair for Haglund syndrome. Foot Ankle Surg 2020;27:421-6. [Google Scholar | PubMed]
- 13.Cottom JM, Hyer CF, Berlet GC, Lee TH. Flexor hallucis tendon transfer with an interference screw for chronic Achilles tendinosis: A report of 62 cases. Foot Ankle Spec 2008;1:280-8. [Google Scholar | PubMed]
- 14.Kolodziej P, Glisson RR, Nunley JA. Risk of avulsion of the Achilles tendon after partial excision for treatment of insertional tendonitis and Haglund deformity: A biomechanical study. Foot Ankle Int 1999;20:433-7. [Google Scholar | PubMed]
- 15.Park M, ElAttrache N, Ahmad C, Tibone J. “Transosseous-equivalent” rotator cuff repair technique. Arthroscopy 2006;22:1360.e1-5. [Google Scholar | PubMed]
- 16.Bisson LJ, Manohar LM. A biomechanical comparison of the pullout strength of no. 2 fiber wire suture and 2-mm fiber wire tape in bovine rotator cuff tendons. Arthroscopy 2010;26:1463-8. [Google Scholar | PubMed]
- 17.Barber FA, Drew OR. A biomechanical comparison of tendon-bone interface motion and cyclic loading between single-row, triple-loaded cuff repairs and double-row, Suture-tape cuff repairs using biocomposite anchors. Arthroscopy 2012;28:1197-205. [Google Scholar | PubMed]
- 18.Liu RW, Lam PH, Shepherd HM, Murrell GA. Tape versus suture in arthroscopic rotator cuff repair. Orthop J Sports Med 2017;5:2325967117701212. [Google Scholar | PubMed]
- 19.Maffulli N, Testa V, Capasso G, Sullo A. Calcific insertional Achilles tendinopathy reattachment with bone anchors. Am J Sports Med 2004;32:174-82. [Google Scholar | PubMed]
- 20.Rigby RB, Cottom JM, Vora A. Early weightbearing using Achilles suture bridge technique for insertional Achilles tendinosis: A review of 43 patients. J Foot Ankle Surg 2013;52:575-9. [Google Scholar | PubMed]