Neonatal compartment syndrome is a rare phenomenon that has a unique presentation but with etiologies that have not been fully discerned; thus, clinicians should maintain high clinical suspicions even without a clear etiology.
Dr. Nathan Cai, Department of Education, The University of Miami Leonard M. Miller School of Medicine, Miami - 33136, Florida, United States. E-mail: nac157@miami.edu
Introduction: Neonatal compartment syndrome is a rare phenomenon with a limited number of cases reported in the literature with varying etiologies. Current literature categorizes etiologies as either intrinsic or extrinsic. To the best of our knowledge, difficult delivery and delivery through vacuum are the only two iatrogenic etiologies that have been reported in the literature. Thus, this may be the first reported case of neonatal compartment syndrome secondary to a failed peripherally inserted central catheter (PICC) insertion.
Case Report: We present a case of a pre-mature neonate with diffuse discoloration, paralysis, and loss of palpable pulses of the right upper extremity after a failed PICC insertion. The clinical features led to a diagnosis of compartment syndrome. Interventions were not carried out due to the pre-maturity and instability of the patient. The patient passed away at 38 days of age due to refractory hypotension and patent ductus arteriosus.
Conclusion: We present a case of neonatal compartment syndrome caused by a previously unreported etiology, highlighting the current dearth of knowledge. Clinicians should be aware of the unique clinical presentation of neonatal compartment syndrome and maintain high suspicion even without an obvious etiology.
Keywords: Compartment syndrome, neonates, vascular.
Compartment syndrome is defined as a condition in which there is increased pressure within a closed, osseofacial compartment, causing a decrease in perfusion and possible muscle and neurovascular damage. It is often a complication of fractures, crush injuries, extended application of tight dressings, extravasation of IV fluids, and burns. These injuries can lead to an increase in interstitial pressure through bleeding and edema. The elevated pressure causes vascular occlusion in the form of decreased venous outflow relative to arterial inflow. Neonatal compartment syndrome presents differently than adult compartment syndrome. Adult compartment syndrome in the extremities typically presents as swelling, pain on passive stretch, paresthesias, paralysis, and absent peripheral pulses. On the other hand, neonatal compartment syndrome is often diagnosed by swelling, discoloration of a limb, and sentinel skin lesions such as bullae, eschars, and ulcers [1,2]. The size of the lesions is usually directly correlated with the severity of the ischemia [1]. The differential diagnosis for neonatal compartment syndrome includes necrotizing fasciitis, aplasia cutis, neonatal gangrene, congenital varicella, and amniotic band syndrome [3]. Neonatal compartment syndrome is a rare phenomenon with a limited number of cases reported [4]. Literature divides the etiologies of this syndrome between extrinsic and intrinsic causes. Extrinsic causes include difficult delivery, amniotic band constriction, and oligohydramnios [1,5]. Intrinsic causes include hypercoagulable states leading to arterial or venous thromboses [1,5]. To our knowledge, difficult delivery and delivery through vacuum are the only two iatrogenic etiologies of neonatal compartment syndrome, and there have been no reported cases of peripherally inserted central catheter (PICC) insertion as a potential etiology [4,6].
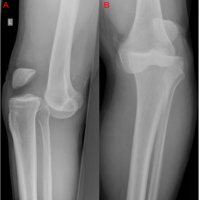
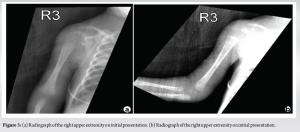
A male baby was born at 24.3 weeks through spontaneous vaginal delivery after a pre-term pre-mature rupture of the membranes with post-delivery acute respiratory failure requiring intubation. The patient suffered from a bilateral grade IV germinal matrix intraventricular hemorrhage without hydrocephalus and a hemodynamically significant patent ductus arteriosus. The pregnancy was complicated by chorioamnionitis. The mother was obese but had no other past medical history. Twelve days after birth, physicians in the neonatal intensive care unit attempted to place a PICC line in the right upper extremity. The procedure failed, and the right upper extremity immediately became pale. Ultrasound after the procedure demonstrated loss of flow in the brachial, radial, and ulna arteries. In the following days, three more attempts at placing a PICC line in the right upper extremity did not succeed. After the third attempt, pediatric surgery successfully placed a broviac central venous catheter in the right internal jugular vein. Serial ultrasounds demonstrated improved flow through the brachial artery but no appreciable reconstitution of blood flow through the radial and ulnar arteries. On examination, there was duskiness of the index finger along with diffuse molding of the arm and forearm. There was sloughing of the skin on the palm and fingertips, with gangrene at the index fingertip. In addition, there was diffuse erythema and swelling of the entire extremity, with dispersed areas of ecchymosis up the hand, forearm, and arm (Fig. 1 and 2). There were no palpable ulnar or radial pulses with a poor waveform from the wrist pulse ox, showing 65% saturation. The patient did not spontaneously move the right upper extremity during the examination. The compartments were soft and compressible throughout the upper extremity. The infectious workup of the patient showed a white blood cell count and erythrocyte sedimentation rate that were within the normal reference range for a pre-mature neonate. Standard radiographs of the upper right extremity showed soft-tissue swelling of the medial arm (Fig. 3). Given the examination and objective findings, a clinical diagnosis of compartment syndrome was made.

Vascular surgery was consulted, and they could not recommend anticoagulation due to the patient’s grade IV intraventricular hemorrhage. In addition, they did not recommend revascularization because of the age and instability of the patient. On reevaluation 6 days later, the forearm remained discolored with stable necrotic tissue on the distal index finger. The patient was able to fire the biceps and triceps spontaneously. The patient was unable to fire wrist or hand muscle groups, with all digits resting in a claw position. Serial ultrasound showed minimal interval reconstitution of the axillary, ulnar, and radial arteries. Per protocol, physical therapy would have been consulted for weight-bearing recommendations, but given the pre-maturity and clinical status of the patient, it was deferred. Over the next 2 weeks, the patient continued to suffer from intractable seizures, anuric renal failure, and worsening respiratory failure despite medical management. The patient passed away at 38 days of age due to refractory hypotension and patent ductus arteriosus.
Neonatal compartment syndrome is a recognized neonatal emergency, although it is poorly understood. Treatment of neonatal compartment syndrome is typically decompressive fasciotomy to prevent further loss of tissue and functionality [1]. Expert advice from pediatric plastic/orthopedic surgery, in conjunction with neonatal/pediatric intensivists, should be promptly obtained for appropriate management. To the best of our knowledge, this is the first reported case of neonatal compartment syndrome in the upper extremity secondary to failed PICC line attempts. Thrombosis is an uncommon but documented complication of PICC line insertions in neonates, with an incidence of 0.26–0.80% [7]. We hypothesize that the etiology of this case is due to a loss of outflow caused by thrombosis from PICC line insertion, leading to increased compartment pressures. This case introduces a new extrinsic cause of neonatal compartment syndrome, highlighting the current dearth of knowledge. Neonatal compartment syndrome is a rare condition, with 26 studies reporting 60 cases [4]. In an evaluation of 50 cases, Agrawal et al. found that 18% of the neonates involved were pre-mature [5]. In addition, a majority of cases reported involved the upper extremity [4]. Diagnosis is typically based on the clinical findings as there are no standard pressure gradients available for neonates [1]. Because the average diastolic pressure in a term neonate is below 40 mmHg, a small increase in compartment pressure will rapidly impair muscle perfusion [8]. Clinical features that are suggestive of this diagnosis include skin discoloration, restricted movement, diminished perfusion, and a sentinel skin lesion, all of which were seen in this case except for a sentinel skin lesion [1,9]. Classic symptoms in adults, such as paresthesia and pain on passive movement, are not useful in diagnosing compartment syndrome in a neonate. Early diagnosis and treatment of neonatal compartment syndrome are critical. Treatment is typically a decompressive fasciotomy to prevent further loss of tissue and functionality [1]. In this case, however, surgical intervention was not carried out due to the pre-maturity of the patient and the critical condition of the patient. Post-anesthetic mortality in children younger than 30 days is significantly higher than that of older children [10]. Patients who are treated experience an average of 1.65 negative outcomes per patient [4]. Long-term negative outcomes include Volkmann contractures, bone growth abnormalities, nerve palsies, scar contractures, and amputation [4,5].
The rarity of neonatal compartment syndrome continues to shroud the extent of its etiologies and associated factors. We present a case of neonatal compartment syndrome with an iatrogenic etiology that has yet to be reported in the literature to our knowledge. Operative intervention was not performed due to the clinical status of the patient, but it may be considered in others.
Neonatal compartment syndrome is a rare phenomenon with etiologies that have yet to be reported in the literature. This case adds to the previously unreported iatrogenic etiology of neonatal compartment syndrome and further documents its unique clinical presentation. Surgeons and clinicians should be aware of the unique clinical presentation of neonatal compartment syndrome and maintain high suspicion even without an obvious etiology. Operative treatment of compartment syndrome may be successful, but it should be considered with respect to a patient’s entire clinical picture and is not without complications, especially in pre-mature patients.
References
- 1.Ragland R 3rd, Moukoko D, Ezaki M, Carter PR, Mills J. Forearm compartment syndrome in the newborn: Report of 24 cases. J Hand Surg Am 2005;30:997-1003. [Google Scholar | PubMed]
- 2.Cherry I, Franck D, Urbain F. Neonatal limb compartment syndrome: A comprehensive review. J Hand Surg Am 2023;S0363-5023(23)00493-8. [Google Scholar | PubMed]
- 3.Cham PM, Drolet BA, Segura AD, Esterly NB. Congenital volkmann ischaemic contracture: A case report and review. Br J Dermatol 2004;150:357-63. [Google Scholar | PubMed]
- 4.Shen AH, Tevlin R, Kwan MD, Ho OH, Fox PM. Neonatal compartment syndrome and compound presentation at birth. J Hand Surg Glob Online 2020;2:166-70. [Google Scholar | PubMed]
- 5.Agrawal H, Dokania G, Wu SY. Neonatal volkmann ischemic contracture: Case report and review of literature. AJP Rep 2014;4:e77-80. [Google Scholar | PubMed]
- 6.Rios M, Ribeiro C, Soares P, Amorim R, Osorio A, Leitao B, et al. Volkmann ischemic contracture in a newborn. BMJ Case Rep 2011;2011:bcr0520114201. [Google Scholar | PubMed]
- 7.Chen H, Zhang X, Wang H, Hu X. Complications of upper extremity versus lower extremity placed peripherally inserted central catheters in neonatal intensive care units: A meta-analysis. Intensive Crit Care Nurs 2020;56:102753. [Google Scholar | PubMed]
- 8.Versmold HT, Kitterman JA, Phibbs RH, Gregory GA, Tooley WH. Aortic blood pressure during the first 12 hours of life in infants with birth weight 610 to 4,220 grams. Pediatrics 1981;67:607-13. [Google Scholar | PubMed]
- 9.Martin B, Treharne L. Neonatal compartment syndrome. Ann R Coll Surg Engl 2016;98:e111-3. [Google Scholar | PubMed]
- 10.van der Griend BF, Lister NA, McKenzie IM, Martin N, Ragg PG, Sheppard SJ, et al. Postoperative mortality in children after 101,885 anesthetics at a tertiary pediatric hospital. Anesth Analg 2011;112:1440-7. [Google Scholar | PubMed]