In this case report, we have shown the safety and effectiveness of bilateral stellate ganglion phenol chemical neurolysis in a patient suffering from Buerger’s disease of both hands.
Dr. Rampal Singh (Additional Professor), A-Block OT Complex, 4th Floor, Department of Anaesthesiology, All India Institute of Medical Sciences, Raipur, Chhattisgarh, India. E-mail: drrampalsingh@aiimsraipur.edu.in
Introduction: Thromboangiitis obliterans (TAO) or Buerger’s disease (BD) is a small and medium-sized arteriovenous segmental occlusive inflammatory disease frequently occurring in men as compared to women. Although a common etiological agent is smoking or tobacco consumption, it has also been reported infrequently in non-smokers. Except for smoking other etiological agents, HLA, autoimmune diseases like systemic lupus erythematosus, and periodontitis have also been suggested. Minimally invasive pain and spine intervention (MIPSI) like stellate ganglion neurolysis with 8% phenol, 10 days apart in patients suffering from bilateral digital ischemia of both hands is a safe and effective treatment.
Case Report: Fifty-five-year-old female with chief complaints of burning pain, swelling, and blackening of all five fingers of the right and four fingers of the left hands excluding the thumb for the past 3 months. On examination, pulse was almost absent at the wrist in both hands. There was no history of smoking. Under aseptic precautions, fluoroscopy and radiocontrast guidance stellate ganglion neurolysis with a 22G spinal needle, 2 ml of 8% phenol, 2 ml of 0.25% bupivacaine and 4 mg of dexamethasone were given at C7 vertebral level 10 days apart on both sides. After 3-4 months of stellate ganglion phenol chemical neurolysis, involved fingers were saved except the gangrenous part which was autoamputated itself in due course of time.
Conclusion: Bilateral interval (10 days apart) chemical neurolysis of stellate ganglion in Buerger’s disease involving both hands is a safe and effective technique in terms of control of disease progression, pain, cardiac complications, and recurrent laryngeal nerve-related complications.
Keywords: Buerger’s disease bilateral hands, phenol chemical neurolysis, stellate ganglion neurolysis.
Thromboangiitis obliterans (TOA) or Buerger’s disease (BD) is a non-atherosclerotic segmental occlusive segmental small and medium-sized arteriovenous disease most commonly occurring in chronic young smokers. The first complete description of the disease was done by Leo Buerger in 1908 who published a complete description of changes in arteries (intimal thickening, occlusive thrombus, and preservation of arterial architecture) in young smokers and named the disease. Disease is prevalent worldwide ranging from 0.5 (Western Europe) to 66% (Asian countries, Japan, and Korea) [1] and 45 to 63% in India [2]. Onset occurs between 40 and 45 years with male-to-female ratio of 100:1. Disease has been strongly associated with tobacco consumption [3] but hereditary susceptibility, immune response, coagulation changes, and infection have also been suggested [1]. The disease has also been reported infrequently in non-smokers [4].
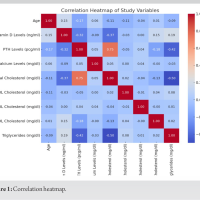
A 50-year-old female patient presented to our pain clinic in November 2017 with chief complaints of pain (burning), swelling, cold peripheries, and blackening of all five fingers of the right (Fig. 1c and d) and four fingers of the left (except thumb) hands (Fig. 1a and b) for the past 3 months. Pain was present during rest, increasing while lifting hands and relieving on bringing down. Diagnosis was made based on clinical examination and the color Doppler study of both upper limbs (Table 1). The patient was consulted with a colleague surgeon who referred the patient.
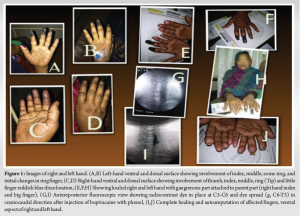
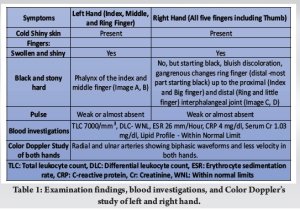
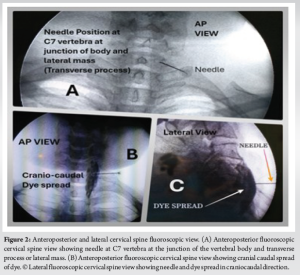
Under all aseptic precautions, 4-5 stellate ganglion blocks were given [accurate needle position (Fig. 2a) was confirmed in anteroposterior and lateral fluoroscopic view (Fig. 2a and c) and craniocaudal dye spread of dye (Fig. 2b) and excluding intravascular position] simply with 0.25% bupivacaine with 4 mg of dexamethasone (only once on both sides) on an alternate day basis using a 22G spinal needle under all aseptic precautions and C-Arm (fluoroscope) guidance at C6 level. After such blocks, chemical neurolysis was successfully done with 2 ml of 8% phenol mixed with 2 ml of 0.25% bupivacaine and 1 ml of radiocontrast non-ionic iodine dye, iohexol 300 under continuous fluoroscopic guidance (to avoid intravascular spread and apical pleura puncture) at C7. Phenol was injected after confirmation of needle position at the junction of the vertebral body and transverse process (Fig. 2a) at C7 in anteroposterior and lateral (Fig. 2c) view and with craniocaudal spread (Fig. 2b) of dye (1 ml, iohexol 300) with the excluding intravascular injection of dye (Fig. 1g, and 2b and c) 10 days apart on both sides (Fig. 1i and Fig. 2b and c) to avoid cardiac complications (bradycardia) and bilateral recurrent laryngeal nerve palsy. After the successful accomplishment of the procedure, there was an increase in the temperature of the hands, an improvement in vascularity and a reduction in swelling and pain. There was a dropping of eyelids, enophthalmos and conjunctival congestion for a transient period. The patient was monitored after every block for at least 2 h in the post-procedure room. In due course of time, the affected salvageable portion of the fingers was saved (Fig. 1e, f and h). The patient was kept on a tramadol-paracetamol combination, pregabalin 75 mg at bedtime, asprin 75 mg once daily, cilastazole 100 mg twice a day, and isosorbide mononitrate 10 mg twice a day by oral route. The patient was followed up for 5-6 months when the gangrenous part was detached from the healthy part (Fig. 1j). Recently till February 2024, there was no recurrence of disease as evident from telephonic contact.
Although exposure to tobacco consumption in any form is strongly associated with Buerger’s disease but it has been found in nonsmokers also [4]. There are risk factors other than tobacco such as periodontal disease, chronic anerobic periodontitis [5], HLA (A9 and B5) antigens, hypercoagulability, endothelial dysfunction, and immunologic mechanisms that have been proposed [6]. Raynaud’s phenomenon is present in about 44% of patients with thromboangiitis obliterans [1] which could be present in this patient. Preganglionic sympathetic nervous system fibers to the upper extremity originate in the first four or five thoracic segments (T1-T4/5) and synapse in the superior, middle, and inferior (stellate) cervical ganglia. In 80% of cases, the stellate ganglion comprises both the inferior cervical and first thoracic ganglia. Post-ganglionic nerves from the cervical ganglia extend into the head, neck, upper extremities, heart, and lungs and carry afferent pain fibers along with them. Postganglionic fiber distribution justifies stellate ganglion neurolysis or block in various chronic painful conditions of the upper limb [7]. Keeping in mind the complications [8] of bilateral stellate ganglion block at a time, we decided to go for a unilateral block on one side (left or right) and on the next day on the other side. We did chemical neurolysis at an interval of 10 days apart after confirming that there was no complication. Simultaneous bilateral stellate ganglion block is only indicated in pulmonary thromboembolism [9]. Bilateral stellate ganglion block is rarely given due to the concern of phrenic and recurrent laryngeal nerve palsy. However, in a case report of a systemic lupus erythematosus (SLE) patient involving fingers of both hands, the author had given repeated stellate ganglion block with 0.25% bupivacaine for the management of progressive gangrene due to vasculitis [10]. Phenol is a neurolytic agent and causes Wallerian degeneration of the nerve axon distal to the lesion [11]. Gabor B. Racz and Jerry T. Holubec used a solution of 2.5 mL of 6% phenol in saline, 1 mL of 80 mg methylprednisolone, and 1.5 mL of 0.5% bupivacaine (giving a 3% phenol solution) to perform a neurolytic block of the stellate ganglion [12]. We used 5-6 ml of drug volume consisting of 3-4 ml of 8% phenol, 1 ml of dexamethasone, and 1 ml of 0.25% bupivacaine and did not find any adverse event or effect. However, phenol has been used in different concentrations ranging from 3 to 12% for neurolysis in different studies [11]. Although smoking cessation is the mainstay of treatment for Buerger’s disease, this patient was a non-smoker. The patient also received oral treatment in the form of blood thinners such as cilostazol 100 mg twice daily [13,14] and asprin 75 mg [15] once a day, for neuropathic pain due to nerve damage by ischemia, pregabalin [16] 75 mg at bedtime, and the collaterals which have been developed during disease process due to ischemia were tried to open up by vasodilators such as isosorbide mononitrate 10 mg twice a day [17].
Minimally invasive percutaneous stellate ganglion interval (10 days apart) phenol chemical neurolysis is a safe and effective treatment in terms of disease pain relief, disease progression, and complications related to cardiac (bradycardia) and recurrent laryngeal nerve in a patient suffering from Buerger’s disease of both hands.
Minimally invasive percutaneous bilateral stellate ganglion phenol chemical neurolysis a few days apart with 2 ml of 8% phenol with 0.25% bupivacaine under the guidance of continuous fluoroscope and radiocontrast dye iohexol 300 is a safe and effective treatment in Buerger’s disease involving both hands.
References
- 1.Cacione DG. Buerger’s disease: Clinical aspects and evidence-based treatments. Vasculitis in Practice - An Update on Special Situations - Clinical and Therapeutic Considerations. London: InTech; 2018. [Google Scholar]
- 2.Arkkila PE. Thromboangiitis obliterans (Buerger’s disease). Orphanet J Rare Dis 2006;1:14. [Google Scholar]
- 3.Sasaki S, Sakuma M, Yasuda K. Current status of thromboangiitis obliterans (Buerger’s disease) in Japan. Int J Cardiol 2000;75:S175-81. [Google Scholar]
- 4.Kulkarni S, Kulkarni GS, Shyam AK, Kulkarni M, Kulkarni R, Kulkarni V. Management of thromboangiitis obliterans using distraction osteogenesis: A retrospective study. Indian J Orthop 2011;45:459-64. [Google Scholar]
- 5.Iwai T, Inoue Y, Umeda M, Huang Y, Kurihara N, Koike M, et al. Oral bacteria in the occluded arteries of patients with Buerger disease. J Vasc Surg 2005;42:107-15. [Google Scholar]
- 6.Vijayakumar A, Tiwari R, Kumar Prabhuswamy V. Thromboangiitis obliterans (Buerger’s disease)-current practices. Int J Inflam 2013;2013:156905. [Google Scholar]
- 7.Openanesthesia. Autonomic Innervation: Upper Extremity. Openanesthesia. Available from: https://www.openanesthesia.org/keywords/autonomic_innervation_upper_extremity/# [Last accessed on 2023 Oct 27]. [Google Scholar]
- 8.Goel V, Patwardhan AM, Ibrahim M, Howe CL, Schultz DM, Shankar H. Complications associated with stellate ganglion nerve block: A systematic review. Reg Anesth Pain Med 2019;???:rapm-2018-100127. [Google Scholar]
- 9.Waldman SD. Pain management. Philadelphia, PA: Elsevier, Saunders; 2011. [Google Scholar]
- 10.Punj J. Multiple bilateral ultrasound-guided stellate ganglion blocks to treat acute vasculitis in a recently diagnosed patient of systemic lupus erythematosus. Indian J Anaesth 2019;63:851-5. [Google Scholar]
- 11.D’souza RS, NSW. Phenol Nerve Block Continuing Education Activity. Available from: https://www.ncbi.nlm.nih.gov/books/nbk525978 Last assessed August 28, 2023 [Google Scholar]
- 12.Prithvi Raj P, Erdine S. Percutaneous block and lesioning of the stellate ganglion. In: Pain-Relieving Procedures: The Illustrated Guide. 1st ed. Chichester, West Sussex, UK: John Wiley and Sons Limited; 2012. p. 207-8. [Google Scholar]
- 13.Liu Y, Shakur Y, Yoshitake M, Kambayashi JJ. Cilostazol (pletal): A dual inhibitor of cyclic nucleotide phosphodiesterase type 3 and adenosine uptake. Cardiovasc Drug Rev 2001;19:369-86. [Google Scholar]
- 14.Bedenis R, Stewart M, Cleanthis M, Robless P, Mikhailidis DP, Stansby G. Cilostazol for intermittent claudication. Cochrane Database Syst Rev 2014;2014:CD003748. [Google Scholar]
- 15.Brunton LL, Chabner BA, Knollmann BC, editors. Goodman and Gilman’s the Pharmacological basis of Therapeutics. 12th ed. New York: McGraw-Hill Companies; 2011. p. 977-82. [Google Scholar]
- 16.Verma V, Singh N, Singh Jaggi A. Pregabalin in neuropathic pain: Evidences and possible mechanisms. Curr Neuropharmacol 2014;12:44-56. [Google Scholar]
- 17.Balasubramanian S, Chowdhury YS. Isosorbide. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557839 [Last accessed on 2023 May 16]. [Google Scholar]