Osteoblastoma mainly affects the spine but can also manifest in the sacrum, with CT scan preferred for imaging and surgical excision favored for treatment, requiring regular follow-up to monitor for potential recurrence and malignant transformation.
Dr. M Harsha Vardhan Reddy, Department of Orthopedics, All India Institute of Medical Sciences, Nagpur, Maharashtra - 441 108, India. E-mail: m.harshareddy1998@gmail.com
Introduction: Osteoblastoma is an uncommon benign bone tumor characterized by the formation of osteoid tissue, occurring more frequently in men than in women. It is often associated with osteoid osteoma and can be found at various locations in the skeleton, although it is rare in the sacrum. Typically, these lesions involve the posterior elements of the spine, including the pedicle and the lamina. We would like to present a case of sacral osteoblastoma, clinically presenting as lumbar radiculopathy, which was treated at our institute.
Case Report: A 23-year-old male presented to us with left gluteal pain radiating to the left lower limb pain for 2 years. He had multiple consultations elsewhere and was being treated as a probable case of a lumbar disc lesion with left lower limb radiculopathy. X-rays appeared normal. Magnetic resonance imaging of the lumbar spine and pelvis revealed a T2 hyperintense lesion affecting the posterior elements of S3, compressing the nerve roots. Computed tomography (CT) was a better investigation modality for osteoblastoma. En bloc excision and curettage were performed, and the histopathological analysis confirmed the diagnosis of osteoblastoma. The patient had immediate relief of symptoms postoperatively with no complications. At 2-year follow-up, the patient had no evidence of recurrence on a follow-up CT scan.
Conclusion: Osteoblastomas predominantly occur in the spine, with rare instances in the sacrum. Treatment typically involves en bloc excision. Confusing clinical presentation may delay diagnosis, resulting in persistent morbidity.
Keywords: Osteoblastoma, sacrum, excisional curettage.
Osteoblastomas are benign bone-forming tumors characterized by well-vascularized connective tissue, active osteoid, and primitive woven bone production. They are more prevalent in men than women and often arise secondary to osteoid osteomas [1]. While they can occur in any skeletal region, they typically involve the posterior elements of the spine, such as the pedicle and lamina. Axial skeleton osteoblastomas constitute 40% of cases, with 20% occurring in the long bones of the lower extremities. However, sacral involvement is rare, comprising only 9% of all primary bone tumors in the sacrum [1,2]. This report outlines the clinical presentation and treatment experience of a rare case of osteoblastoma in the sacrum of a 23-year-old male.
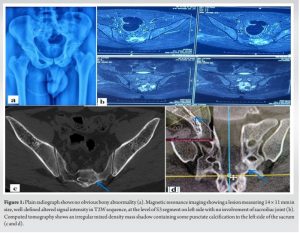
A 23-year-old male patient presented to our department’s spine clinic with complaints of left gluteal region pain and left lower limb pain for 2 years that had been progressive, more at night, and he also experienced paresthesia around the perianal area and claudication pain on walking. He had multiple consultations elsewhere for these complaints and was being treated as a probable case of lumbar disc lesion with left lower limb radiculopathy. On examination, the SLR test was negative; there was no motor deficit, decreased sensation in the S2 and S3 dermatomes, and tenderness over the left SI joint region. The radiographs were unremarkable (Fig. 1a). The patient had already done magnetic resonance imaging (MRI) (Fig. 1b), which showed a lesion measuring 14 × 11 mm in size with a well-defined hyperintense signal in the T2 sequence at the level of the S3 segment on the left side with no involvement of the sacroiliac joint. Given the clinical presentation of night pain and MRI findings indicating a potential neoplastic etiology, we pursued further definitive imaging with a computed tomography (CT) scan. The CT scan revealed a lesion measuring 10 × 7 mm in the sacral canal, predominantly on the left side, with some punctate calcification (Fig. 1c and d) indicative of osteoid osteoma/osteoblastoma. The patient was planned for en bloc excision of the lesion.
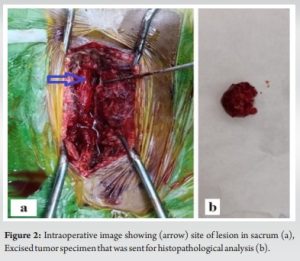
The patient was placed in a prone position under general anesthesia, and laminectomy from S1 extending downward till S3 was done to reach the lesion, which was removed en bloc, and the surrounding area was further curetted (Fig. 2a and b). The tumor was sent for histopathological analysis. Postoperatively, the patient had complete relief of symptoms with no neurological complications.
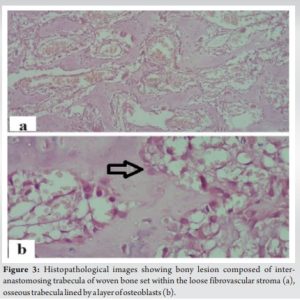
The histopathological analysis of the resected tissue showed bony tissue composed of anastomosing trabecula of woven bone set within loose fibrovascular stroma, consistent with osteoblastoma (Fig. 3a and b).
The patient was discharged without any complications. The patient was completely free from pain during daily activities, and there has been no evidence of recurrence in the CT scan till 2-year follow-up (Fig. 4).

Typically, osteoblastoma manifests in young adults, with a slightly higher incidence in males [1]. Spinal osteoblastoma may present with symptoms such as radicular pain [2], scoliosis, and neurological defects. There is often a delay of several months between the onset of pain and surgical intervention, as it is often overlooked and neglected at the sacrum compared to other sites, possibly due to the broad range of differential diagnoses for lower back pain in routine medical practice [3]. Osteoblastoma’s radiographic presentation is non-specific, posing a risk of misdiagnosis as with other bone tumors. The initial diagnosis relies on plain radiographs at the pain site. CT scans aid in assessing bony aspects of the lesion, sclerosis degree, and bony involvement. MRI offers superior insights into osteoblastoma extent and soft-tissue involvement, complementing CT findings. However, MRI’s role in spinal osteoblastomas is limited due to potential misinterpretation from adjacent inflammatory changes [4,5]. In a series of 18 sacral tumor cases, Ruggeri et al. recommend a comprehensive pre-operative evaluation using both CT and MRI. CT is deemed essential for assessing bony involvement, whereas MRI offers additional insights into the canal, nerve roots, soft tissues, and extraspinal extension. Jambhekar et al. described osteoblastoma histologic morphology as interconnecting osteoid seams lined by plump osteoblasts with numerous ecstatic stromal vessels [6]. Hence, histopathological confirmation is crucial for accurate diagnosis, particularly as CT or MRI may not reveal the osteoblastoma’s special nature. Treatment options for osteoblastoma range from minimally invasive radiofrequency ablation (RFA) to radical excision [7]. RFA utilizes thermal energy to induce coagulation necrosis and is preferred for small, non-aggressive osteoblastomas in long bones [8]. It is also considered when en bloc resection is impractical, especially for large tumors in challenging surgical areas such as the sacrum and recurrent or inappropriately removed tumors. Whittingham-Jones et al. described the sacral osteoblastoma involving the left SI joint treated with en bloc resection [9]. Reynolds et al. described the use of neoadjuvant denosumab and en bloc resection in aggressive sacral osteoblastoma [10]. While wide-margin surgery theoretically minimizes recurrence, it raises the risk of surgical morbidity, particularly for lesions in the sacrum. Local adjuvants do not seem to decrease the risk of local recurrence when combined with surgery [10]. In the surgical treatment of osteoblastoma, ensuring the complete removal of tumor lesions is imperative, along with preserving the sacral nerves, which becomes equally essential. In our case, after weighing the pros and cons and taking the size of the tumor into account, the decision was taken to perform an excision with a simple curettage without instrumentation. At a 2-year follow-up, there is no tumor recurrence in the CT scan and no disability in the patient.
Mimickers do exist for osteoblastoma such as osteoid osteoma, osteosarcoma, and ossifying fibroma. It is crucial due to clinical, radiographic, or histopathological similarities. Especially areas like the sacrum pose challenges in diagnosis, emphasizing the significance of early diagnosis is essential to prevent neurological symptoms and consequences such as cauda equina. Overall, when treated early and promptly, osteoblastoma typically carries a good prognosis.
Osteoblastoma of the sacrum presents a rare but significant diagnostic and treatment challenge. While surgical excision remains the mainstay of treatment, careful consideration of biopsy findings and vigilant follow-up are essential due to the potential for recurrence and malignant transformation.
References
- 1.Ruggieri P, Huch K, Mavrogenis AF, Merlino B, Angelini A. Osteoblastoma of the sacrum: Report of 18 cases and analysis of the literature. J Spine (Phila Pa 1976) 2014;39:E97-103. [Google Scholar | PubMed]
- 2.Saghieh S, Rameh C, Birjawi G, Lakkis S. Sacral osteoblastoma presenting as a L5-S1 disc herniation. Int Surg 2005;90:289-92. [Google Scholar | PubMed]
- 3.Li ZH, Ma H, Fu Q, Hou TS. Clinical manifestation and surgical treatment of spinal osteoblastoma. Zhonghua Wai Ke Za Zhi 2012;50:110-4. [Google Scholar | PubMed]
- 4.Patnaik S, Jyotsnarani Y, Uppin SG, Susarla R. Imaging features of primary tumors of the spine: A pictorial essay. Indian J Radiol Imaging 2016;26:279-89. [Google Scholar | PubMed]
- 5.Huang Z, Fang T, Si Z, Li Y, Zhang L, Zheng C, et al. Imaging algorithm and multimodality evaluation of spinal osteoblastoma. BMC Musculoskelet Disord 2020;21:240. [Google Scholar | PubMed]
- 6.Jambhekar NA, Desai S, Khapake D. Osteoblastoma: A study of 12 cases. Indian J Pathol Microbiol 2006;49:487-90. [Google Scholar | PubMed]
- 7.Sar C, Eralp L. Surgical treatment of primary tumors of the sacrum. Arch Orthop Trauma Surg 2002;122:148-55. [Google Scholar | PubMed]
- 8.Wang B, Han SB, Jiang L, Yuan HS, Liu C, Zhu B, et al. Percutaneous radiofrequency ablation for spinal osteoid osteoma and osteoblastoma. Eur Spine J 2017;26:1884-92. [Google Scholar | PubMed]
- 9.Whittingham-Jones P, Hughes R, Fajinmi M, Lehovsky J, Saifuddin A. Osteoblastoma crossing the sacro-iliac joint. Skeletal Radiol 2007;36:249-52. [Google Scholar | PubMed]
- 10.Reynolds JJ, Rothenfluh DA, Athanasou N, Wilson S, Kieser DC. Neoadjuvant denosumab for the treatment of a sacral osteoblastoma. Eur Spine J 2018;27 Suppl 3:446-52. [Google Scholar | PubMed]











