This is a case report regarding a rare location of desmoplastic fibroblastoma on the ankle of a 76-year-old female.
Dr. Thomas Cuinet, Department of Orthopedic Surgery, Centre Chirurgical Emile Gallé, University Hospital of Nancy, Nancy, France. E-mail: cuinet.thomas@gmail.com
Introduction: Desmoplastic fibroblastoma is a rare, slow-growing benign soft tissue tumor. It has a wide anatomical distribution and mainly affects adult males. Fourteen percent of cases occur in the ankle or foot.
Case Report: In this study, we report a rare location of desmoplastic fibroblastoma on the ankle of a 76-year-old female, discovered as a slowly growing mass. Discussion: Desmoplastic fibroblastoma is an anatomical and clinical entity. It appears macroscopically as a pseudocartilaginous structure and histologically as a stellate or spindle-shaped fibroblastic proliferation in a collagenous stroma.
Conclusion: Desmoplastic fibroblastoma has anatomical specificities and should still be clearly distinguished from certain malignant tumors.
Keywords: Ankle, benign tumor, fibroblastoma.
Desmoplastic fibroblastoma is a rare benign soft tissue tumor first described by Evans in 1996 [1]. This tumor is considered benign by the World Health Organization’s classification of tumors of soft tissue and bone. It shares some characteristics with other soft tissue lesions, such as desmoid tumors, and very rarely affects bony structures. A misdiagnosis of this type of pathology can lead to unnecessary and debilitating surgical treatment. Here, we report a case on the ankle, illustrating the different clinical, histological, and iconographic aspects of this lesion.
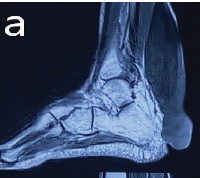
A 76-year-old female presented with a complaint of a mass adjacent to her right lateral malleolus that had been increasing in size for 3 months with no apparent trauma or infection. This mass caused discomfort when putting on shoes and walking, prompting her to seek treatment. On clinical examination, the patient presented with a firm, right lateral retromalleolar mass, 4 cm in length and uniform in depth (Fig. 1). There was no associated skin disorder or locoregional adenopathy. There was no sensorimotor deficit, and the rest of the examination was unremarkable.
Standard radiographs were unremarkable, apart from some soft tissue swelling. There was no osteolysis (Fig. 2). Ultrasound examination of the lesion revealed a solid, heterogeneous polylobed mass 40 mm in length and 29 mm wide, located between the Achilles tendon and the peroneal tendons, in the Kager’s fat pad. Doppler ultrasound of the mass indicated moderate superficial vascularization. A computed tomography (CT) scan of the right ankle was performed as part of the usual tumor workup at our center. It revealed the presence of bone edema of the posterior process of the talus, which may be secondary to the mechanical stresses induced by the tissue lesion (Fig. 3). There was a lateral focal talocrural arthropathy with a moderate joint effusion and signs of mechanical synovitis.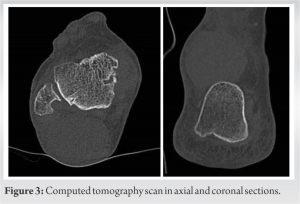
Magnetic resonance imaging (MRI) confirmed the existence of a fibrous tissue lesion of the posterolateral soft tissues of the ankle developed within Kager’s fat pad measuring 40 × 33 mm axially by 42 mm in height. The lesion was in contact with the posterior surface of the Achilles tendon approximately 21 mm in height and in contact with the retinaculum of the peroneal tendons in their retromalleolar portion approximately 30 mm in height. On this MRI, there was no intralesional hemosiderin deposit, and a progressive and heterogeneous raising without washout was observed (Fig. 4 and 5).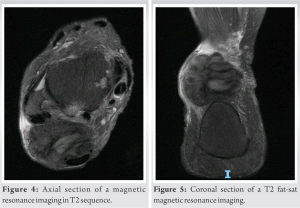
Overall, the imaging workup revealed a fibrous tissue lesion developed within Kager’s fat pad of the right ankle, of undetermined malignancy, meeting the posterior surface of the Achilles tendon and within the retinaculum of the peroneal tendons in the retromalleolar space. A biopsy under ultrasound was performed, which identified a spindle cell proliferation showing no signs of malignancy, and the appearance was compatible with desmoplastic fibroblastoma (Fig. 6).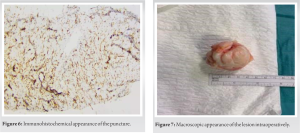
After a group discussion, the patient elected to proceed with surgical excision. A whitish, homogeneous polylobed lesion of firm consistency measuring 5 × 5 × 3.2 cm was excised, and its histological examination confirmed the diagnosis of desmoplastic fibroblastoma (Fig. 7-9).
The postoperative recovery was simple, with the lesion healing well and immediate weight-bearing possible. At 1 year’s follow-up, no sign of recurrence was observed, and functional recovery was satisfactory.
Desmoplastic fibroblastoma is a distinct anatomical and clinical entity. The tumor was first described by Evans in 1995 [1]. This tumor was renamed collagenous fibroma in 1996 by Nielsen et al. [2], corresponding better to the histological description of the lesion comprising mature fibroblasts and collagenous tissue. In 1998, the name “stellate-shaped fibroma” was given to this lesion by Miettinen and Fetsch in view of the presence of stellate or spindle-shaped fibroblasts within the tumor proliferation [3]. It presents clinically as a well-defined, firm, asymptomatic subcutaneous mass, with a slow evolution. It occurs mainly in adult males (sex ratio 2.5/1), between 50 and 70 years old. Very few cases have been described. It has a wide anatomical distribution with various locations, including arms, forearms, shoulders, and back [4]. Desmoplastic fibroblastoma in the ankle or foot is rare (14% of cases) [5,6]. The tumor size varies between 1 and 4 cm on average, and the reports have shown as large as 20 cm [3]. The diagnostic and therapeutic strategy for this tumor depends on its size, as in soft tissue tumors. Usually, an MRI or a CT scan is assessed before performing a surgical biopsy to allow for an anatomical and pathological diagnosis. After confirmation of the diagnostic, a complete excision with negative margins should be offered to the patient. When the lesion is superficial, small, and well-delineated, primary excision is possible without biopsy. MRI offers the greatest accuracy among available imaging tests. The lesion is described as well delineated, with a low signal predominant in the areas of high collagen density, with heterogeneous areas of strong signal hypercellularity in the T2 sequence (Fig. 4 and 5). Moderate raising of the walls can be observed, especially in intramuscular lesions. This is a key point for differentiating it from more aggressive lesions where the liquid signal dominates as in fibromyxoid sarcomas [7,8]. On standard radiography, there is sometimes more or less defined bone remodeling. CT scan is not very accurate for this type of lesion. Desmoplastic fibroblastomas are soft tissue tumors that macroscopically appear as limited, oval lesions. Histologically, they present with a thin fibrous capsule. The lesions contain a homogeneous eosinophilic collagen matrix, with some areas of hyalinization. The cells are dispersed in the fibrous tissue, whereas on the periphery, the cells are relatively compact. The cells are like to activate fibroblasts with an eosinophilic cytoplasm. The nucleus is oval, without atypia, and basophilic [9]. Mitotic activity is low within the cell and mainly localized in the periphery. There are no necrotic areas within these lesions. Blood vessels are few and small within the matrix, with thin walls. Infiltration of adjacent tissues is rare but possible. The immunohistochemical aspect is essential for the differential diagnosis of these tumors. The main differential diagnosis is a desmoid tumor. On the histological level, these are lesions of greater cellularity, vascular, and infiltrative on the periphery. MRI finds larger areas with a strong T2 signal, explained by greater cellularity. In addition, both desmoid tumor and desmoplastic fibroblastoma express smooth muscle actins, but 70–75% of desmoid tumors express beta-catenin, unlike desmoplastic fibroblastomas. Other differentials include lymphomas, histiocytomas, fibrosarcomas, or chondrosarcomas that have a greater peripheral infiltration and a necrotic portion on MRI. Finally, another differential is tendon sheath fibroma, which presents a t(2;11) (q31;q12) translocation just like desmoplastic fibroblastoma. Smooth muscle actins are expressed in both tumor types. However, tendon sheath fibroma is attached to the tendons. Microscopic examination of the fibromas reveals sheaths of collagen bundle tendons with some peripheral vessels, unlike desmoplastic fibroblastomas [10-14]. The treatment of these lesions is surgical, with a complete excision of the lesion in negative margins [2]. The prognosis for these tumors is very good, with very few recurrences for a period of up to 12 years. They do not give rise to metastases, even with small excision margins, which distinguishes them from desmoid tumors.
Desmoplastic fibroblastoma tends to affect elderly male patients and appears in various anatomical distributions. The large size of the tumor and its slow growth suggest that it is a lesion of a benign nature. It should still be clearly distinguished from certain malignant tumors.
This article reports a rare location of desmoplastic fibroblastoma, which is a benign tumor. We developed the anatomical, histological, and radiological specificities, in order to distinguish this pathology from certain malignant tumors.
References
- 1.Evans HL. Desmoplastic fibroblastoma. A report of seven cases. Am J Surg Pathol 1995;19:1077-81. [Google Scholar | PubMed]
- 2.Nielsen GP, O’Connell JX, Dickersin GR, Rosenberg AE. Collagenous fibroma (desmoplastic fibroblastoma): A report of seven cases. Mod Pathol 1996;9:781-5. [Google Scholar | PubMed]
- 3.Miettinen M, Fetsch JF. Collagenous fibroma (desmoplastic fibroblastoma): A clinicopathologic analysis of 63 cases of a distinctive soft tissue lesion with stellate-shaped fibroblasts. Hum Pathol 1998;29:676-82. [Google Scholar | PubMed]
- 4.Evans S, Ramasamy A, Jeys L, Grimer R. Desmoplastic fibroma of bone: A rare bone tumour. J Bone Oncol 2014;3:77-9. [Google Scholar | PubMed]
- 5.Sassi SH, Doghri R, Kanoun ML, Maitig MB, Driss M, Mrad K, et al. Desmoplastic fibroblastoma of the foot. Rev Chir Orthop Reparatrice Appar Mot 2008;94:188-92. [Google Scholar | PubMed]
- 6.Koba T, Susa M, Nakayama R, Watanabe I, Horiuchi K, Mukai M, et al. Desmoplastic fibroma arising in the distal phalanx of the great toe: A case report. J Foot Ankle Surg 2014;53:71-4. [Google Scholar | PubMed]
- 7.Ng E, Tandon AA, Ho BC, Chong BK. Characterising benign fibrous soft-tissue tumours in adults: Why is it so difficult and what do we need to know? Clin Radiol 2015;70:684-97. [Google Scholar | PubMed]
- 8.Urigo C, Schenkel MC, Assal M, Bianchi S. Calcified desmoplastic fibroblastoma of the foot: imaging findings. Skeletal Radiol 2017;46:565-9. [Google Scholar | PubMed]
- 9.Wang J, Lu H, Shi D, Zhu X, Zhang R. The morphological characteristics of desmoplastic fibroblastoma. Zhonghua Bing Li Xue Za Zhi 2000;29:331-3. [Google Scholar | PubMed]
- 10.Laredo JD. Imagerie Rhumatologique et Orthopédique. Montpellier: Sauramps Médical; 2016. [Google Scholar | PubMed]
- 11.Allen R, Parks C, Dini M. Desmoplastic fibroblastoma (collagenous fibroma) of the foot: A case report of a rare benign tumor in an atypical patient. J Am Podiatr Med Assoc 2022;112:19-20. [Google Scholar | PubMed]
- 12.Jariwala T, Gazes MI, Pressman MM. Desmoplastic fibroblastoma: A case of a rapidly growing mass in the foot. J Am Podiatr Med Assoc 2022;112:20-97. [Google Scholar | PubMed]
- 13.Bakhshwin A, Oaxaca G, Armstrong S, Ko J, Billings S. Superficial desmoplastic fibroblastoma (collagenous fibroma): Clinicopathologic study of 11 cases. J Cutan Pathol 2024;51:70-5. [Google Scholar | PubMed]
- 14.Lee SM, Ha DH, Kang SH, Kim SW, Choi YR. Desmoplastic fibroblastoma mimicking tenosynovial giant cell tumor encasing a tendon of the foot. Skeletal Radiol 2019;48:637-41. [Google Scholar | PubMed]