Tuberculous osteomyelitis in the foot, though rare, should be considered in patients presenting with chronic, non-specific foot lesions, especially in high-risk populations.
Dr. Prabu Manoharan, Department of Orthopaedics, Government Medical College, Chennai, Tamil Nadu, India. E-mail: kevinprabu86@gmail.com
Introduction: Tuberculous (TB) osteomyelitis of the foot is a rare entity, often leading to diagnostic challenges due to its atypical presentation and similarity to other foot pathologies.
Case Report: A 19-year-old male presented with persistent pain and discharge in the left foot for 9 months. Despite previous incision and drainage, the condition progressed. Clinical examination revealed a 1 × 1 cm swelling with indurated margins and a discharging sinus. Diagnostic imaging suggested osteomyelitis, confirmed as TB in nature through histopathological examination, revealing caseous necrosis and langerhans giant cells.
Conclusion: This case illustrates the importance of considering TB osteomyelitis in differential diagnoses of chronic foot lesions and highlights the effectiveness of combined surgical and medical management.
Keywords: Tuberculosis, osteomyelitis, cuboid.
Tuberculosis (TB), a significant global health concern, poses unique challenges in its extrapulmonary forms, including osteomyelitis. Particularly in regions with high population density and socioeconomic challenges, TB remains prevalent. TB osteomyelitis, though less common among extrapulmonary TB manifestations, presents distinct diagnostic and therapeutic challenges [1,2]. The occurrence of TB in the foot, accounting for a minor fraction of osteoarticular and extrapulmonary TB cases, is especially rare [3,4]. The involvement of the foot in TB can affect various parts, such as the forefoot, midfoot, and ankle, and often mimic other conditions like pyogenic osteomyelitis or avascular necrosis [1,2]. The diagnostic process for TB osteomyelitis in the foot is complex due to its non-specific presentation and resemblance to other foot and ankle pathologies. This necessitates a high level of clinical suspicion, particularly in patients presenting with localized swelling and persistent draining sinuses [1,2]. Diagnosis often relies on a combination of imaging studies, histological examination, and microbiological culture. However, radiographic features can be non-specific, and even magnetic resonance imaging (MRI) findings, while helpful, are not definitive [1,2]. The management of TB osteomyelitis in the foot and ankle involves a combination of prolonged anti-TB therapy and surgical interventions, particularly in severe cases involving joint or bone deformities, pathological fractures, neurological compromise, or abscesses. The outcomes are generally favorable with appropriate treatment, which underscores the importance of early diagnosis and management [1,2].
A 19-year-old male was referred to our institution with a history of persistent pain and discharge from the left foot, persisting for approximately 9 months. The initial presentation was a swelling over the dorsum of the foot, which, despite receiving an incision and drainage at a local hospital about 8 months prior, had progressed to a chronic, seropurulent discharge. On clinical examination, we observed a 1 × 1 cm swelling on the lateral aspect of the left foot. The swelling, while not acutely inflamed, displayed indurated margins and was characterized by a discharging sinus. Notably, there was an absence of typical signs of inflammation such as warmth and redness. This clinical picture (Fig. 1) suggested a complex, possibly chronic infectious process, warranting further diagnostic evaluation.
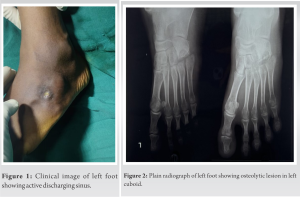
Imaging studies were a critical component of our diagnostic process. Initial radiographs of the foot revealed subtle yet significant changes suggestive of an underlying osteomyelitic process (Fig. 2). However, given the complexity of the case, an MRI scan was deemed essential for a more comprehensive assessment. The MRI images, as shown in Fig. 3, demonstrated findings consistent with osteomyelitis, particularly involving the tarsal bones. These findings were pivotal in confirming our clinical suspicion of a chronic infectious process, possibly of a tubercular etiology.
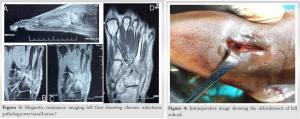
The decision to proceed to surgery was based on the need for both therapeutic and diagnostic interventions. Intraoperatively, extensive areas of caseous necrosis were encountered, along with the presence of Langerhans giant cells, as depicted in the intraoperative photographs in Fig. 4 and 5. These findings were highly suggestive of TB osteomyelitis, a relatively rare presentation in our clinical practice.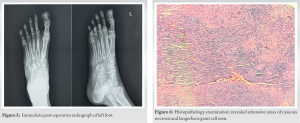
Histopathological examination of the biopsied tissue further confirmed our diagnosis (Fig. 6). The presence of caseating granulomas and Langerhans giant cells was consistent with TB infection, a diagnosis that has become increasingly rare in developed countries but remains a significant clinical entity in many parts of the world.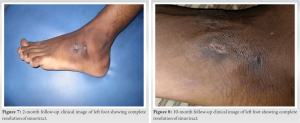
The management of this patient was multifaceted and tailored to the patient’s specific needs and the severity of the infection. We initiated a rigorous anti-TB therapy regimen of IP drugs (Isoniazid, Rifampicin, Pyrazinamide, and Ethambutol) every day for 4 months and CP drugs (Isoniazid, Rifampicin, and Ethambutol) every day for 2 months and was tailored to continue CP phase drugs for 2 more months. The patient has completed the treatment for 8 months. The follow-up at 2 and 10 months (Fig. 7 and 8), as evidenced by the X-ray image (Fig. 9 and 10), demonstrated significant radiological improvement. The patient reported a substantial reduction in pain and discharge, and there was a noticeable resolution of the swelling on clinical examination.
TB osteomyelitis accounts for a small fraction of extrapulmonary TB cases. A study in the Journal of Infectious Diseases in Developing Countries emphasizes the rarity of foot and ankle involvement in TB, noting that only about 1% of extrapulmonary TB patients exhibit this manifestation [5]. The clinical presentation is often non-specific, leading to diagnostic delays. As in the case presented, patients may exhibit chronic pain, swelling, and in some instances, sinus formation or discharge, which are common to various other conditions, thus necessitating a high index of suspicion. Diagnosing TB osteomyelitis is complicated due to its insidious onset and non-specific clinical and radiological features. The integration of clinical, radiological, and microbiological data is crucial. The study by Jha and Chaudhary outlines the significance of various imaging techniques such as conventional radiography, MRI, and computed tomography scans in detecting osteomyelitis [6]. These modalities are particularly useful in identifying TB osteomyelitis, which may show bone erosion, sclerosis, and soft-tissue involvement. However, these findings are not pathognomonic and can be seen in other conditions, necessitating further investigation. The definitive diagnosis often hinges on microbiological and histopathological evidence. Cultures and histopathology can confirm the presence of mycobacterium TB, as well as provide data on drug susceptibility, which is essential for guiding therapy. The presence of caseating granulomas and Langerhans giant cells, as observed in the current case, is suggestive of TB but not exclusive to it [7]. The management of TB osteomyelitis involves a combination of surgical and medical therapies. Surgical intervention often includes debridement and may involve bone grafting or stabilization in certain cases. Medical management is primarily prolonged antibiotic therapy, tailored to the organism’s drug susceptibility profile. The American family physician review highlights the need for prolonged anti-TB therapy, often lasting several months [7]. This approach aligns with the management in the presented case, where a regimen including Rifampicin, Isoniazid, and Ethambutol was used. Close follow-up is necessary to monitor treatment response and detect any recurrence. The radiological improvement and clinical response, as observed in the 2-month follow-up in the presented case, are encouraging but must be monitored over a longer period due to the risk of recurrence. Reviewing similar cases in the literature provides valuable insights into the variability of presentations and the need for individualized treatment plans [8,9]. A review of 125 cases of TB osteomyelitis further underscores the diversity in clinical presentations and the importance of considering this diagnosis in atypical cases of chronic osteomyelitis [10].
The presented case of TB osteomyelitis in the foot underscores the need for a high degree of clinical suspicion, particularly in patients presenting with chronic, non-specific symptoms. The integration of clinical, radiological, and microbiological data is paramount in establishing the diagnosis. The management involves a combined surgical and medical approach, with close follow-up to ensure treatment efficacy and monitor for recurrence. This case adds to the growing body of knowledge on the complex and varied presentations of TB osteomyelitis, highlighting the necessity for heightened clinical awareness and a tailored approach to patient care.
- Early and accurate diagnosis of TB osteomyelitis is crucial, requiring a high index of suspicion and a combination of clinical, radiological, and histopathological evaluations.
- Effective management involves a multidisciplinary approach, combining both surgical intervention and prolonged anti-TB therapy, tailored to individual patient needs.
References
- 1.Korim M, Patel R, Allen P, Mangwani J. Foot and ankle tuberculosis: Case series and literature review. Foot (Edinb) 2014;24:176-9. [Google Scholar | PubMed]
- 2.Faroug R, Psyllakis P, Gulati A, Makvana S, Pareek M, Mangwani J. Diagnosis and treatment of tuberculosis of the foot and ankle-A literature review. Foot (Edinb) 2018;37:105-12. [Google Scholar | PubMed]
- 3.Dhillon MS, Nagi ON. Tuberculosis of the foot and ankle. Clin Orthop Relat Res 2002;398:107-13. [Google Scholar | PubMed]
- 4.Vohra R, Kang HS, Dogra S, Saggar RR, Sharma R. Tuberculous osteomyelitis. J Bone Joint Surg Br 1997;79:562-6. [Google Scholar | PubMed]
- 5.Pes M, Amorese V, Baioni A, Donadu MG, Molicotti P, Milia F, et al. A rare presentation of tubercular osteomyelitis of the foot. J Infect Dev Ctries 2022;16:1655-9. [Google Scholar | PubMed]
- 6.Jha Y, Chaudhary K. Diagnosis and treatment modalities for osteomyelitis. Cureus 2022;14:e30713. [Google Scholar | PubMed]
- 7.Bury DC, Rogers TS, Dickman MM. Osteomyelitis: Diagnosis and treatment. Am Fam Physician 2021;104:395-402. [Google Scholar | PubMed]
- 8.Dhillon MS, Singh P, Sharma R, Gill SS, Nagi ON. Tuberculous osteomyelitis of the cuboid: A report of four cases. J Foot Ankle Surg 2000;39:329-35. [Google Scholar | PubMed]
- 9.Jeyaraman N, Jeyaraman M, Muthu S, Packkyarathinam RP. Tubercular osteomyelitis of cuboid. J Orthop Case Rep 2021;11:5-10. [Google Scholar | PubMed]
- 10.Martini M, Adjrad A, Boudjemaa A. Tuberculous osteomyelitis. A review of 125 cases. Int Orthop 1986;10:201-7. [Google Scholar | PubMed]