This manuscript describes a simple and useful technique with a broad scope of applications, for the calibration of femoral component rotation using the posterior condylar axis as the reference, during image-free robot-assisted total knee arthroplasty.
Dr. Apurve Parameswaran, Department of Orthopaedic Surgery, Medicover Hospitals, Hyderabad, Telangana, India. E-mail: doctorapurve@gmail.com
Introduction: The use of image-free robotic systems for total knee arthroplasty (TKA) is gaining popularity. Although the surgical transepicondylar axis (sTEA) is considered the optimal femoral rotational reference during TKA, it is difficult to define intra-operatively. Conventional and image-free robot-assisted TKA (RA-TKA) therefore rely on the use of Whiteside’s axis (WSA) or the posterior condylar axis (PCA) as surrogate references. The PCA is considered to be associated with less variability than WSA. The authors present a simple technique to permit calibration of femoral component rotation (FCR) using the PCA as a reference for image-free robotic systems that do not permit this option.
Technique: The image-free robotic systems used by the authors (Navio and CORI, Smith and Nephew, Memphis, TN, USA) permit calibration of FCR only when the perpendicular to WSA is used as a reference. When the PCA is selected as a reference, a fixed 3° of external rotation is set by the robot. The technique proposed by the authors involves the use of the former setting, followed by internal rotation of the perpendicular to WSA to co-align it with the PCA. The planning menu subsequently permits virtual surgical planning using the PCA as the femoral rotational reference and permits adjustments in rotational positioning of the femoral component while displaying the effect of rotation on bony resection and vice versa in real time. In addition, coaligning the perpendicular to WSA with the anatomic trans-epicondylar axis (aTEA) displays the internal rotation of the PCA with respect to the aTEA. This information can be used for setting rotational boundaries with respect to the PCA while using various alternate alignment strategies, like functional alignment, since the relation between the aTEA and sTEA is less likely to be affected by dyplasia and wear when compared with the PCA or WSA.
Conclusion: This simple technique permits optimally calibrated rotational positioning of the femoral component during image-free RA-TKA, using the PCA as a reference. It can be applied for optimizing surgery in knees with altered or outlier anatomy, as well as routinely, especially when alternate alignment strategies are used.
Keywords: Femoral component rotation, robot-assisted total knee arthroplasty, posterior condylar axis, trans-epicondylar axis, image-free robotics.
Recent advances in surgical technology, including computer navigation, patient-specific cutting blocks, and robotic surgery, have led to an increase in the use of personalized alignment strategies during total knee arthroplasty (TKA) [1]. Robot-assisted TKA (RA-TKA) permits accurate planning of component positioning while providing real-time feedback on the precise effect of calibrated multi-planar alterations in bony resection on the gap status [2]. This has led to a growing interest in alternate alignment strategies like functional and inverse kinematic alignment and permitted refinement of the existing options of mechanical, kinematic, and restricted kinematic alignment [1]. Robotic systems using pre-operative computed tomography scans permit the surgeon to base femoral rotational alignment on the surgical trans-epicondylar axis (sTEA). Image-free robots, however, continue to rely on the use of the posterior condylar axis (PCA) or Whiteside’s axis (WSA), since they use intra-operative bone-mapping to generate a free-collection mesh on which surgical planning is based. Image-free RA-TKA is gaining in popularity since it avoids exposure to radiation while providing comparable surgical accuracy [3]. The authors have used the Navio (Smith and Nephew, Memphis, TN, USA) and CORI (Smith and Nephew, Memphis, TN, USA) robotic systems extensively in their practice. These systems present two options for defining the femoral rotational axis: (a) a line at 3° of external rotation from the system-generated, mesh-derived PCA and (b) the perpendicular to a user-defined femoral anteroposterior axis. Though both options permit subsequent calibration of bony resection, at the time of preparing this manuscript, the former precluded an assessment of its effect on femoral component rotation (FCR) and patient-specific calibration of FCR using the PCA as a reference. This led to the development of a simple but useful technique by the authors to circumvent this limitation. This technique is applicable for both Navio and CORI robotic systems (Smith and Nephew, Memphis, TN, USA).
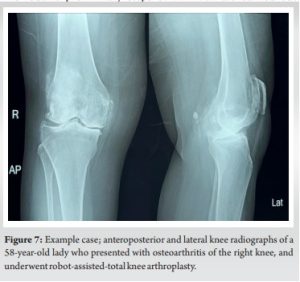
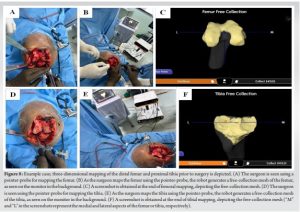
The routine preliminary steps of RA-TKA are carried out. Following appropriate anesthesia, the patient is placed supine. The lower limb is painted and draped over a tourniquet. Surgical preferences including the chosen method of defining the femoral rotational axis are entered into the robotic system interface. An anterior midline approach is used. The preferred arthrotomy and surgical exposure of the joint are performed. Registration of bony landmarks and the centers of rotation of the hip, knee and ankle are carried out. The distal femur and proximal tibia are three-dimensionally mapped using a pointer probe and trackers, to generate a free-collection mesh, which shall be used for surgical planning. When the “use PCA” option for defining the femoral rotational axis is selected (Fig. 1), a fixed value of 3° of external rotation from the mesh-generated PCA is employed by the system. The surgical planning menu subsequently does not provide the value of FCR in real-time while performing alterations in component positioning (Fig. 2), since this rotation is considered appropriate by the system.
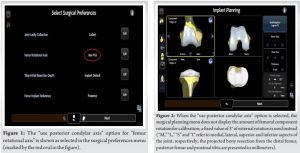
Although 3° of external rotation from the PCA might be adequate for most patients, its universal application would result in flexion gap imbalance in a large proportion of patients. Lack of the ability to titrate bony resection while assessing the impact on the gap status would be a suboptimal usage of the robot. On the other hand, when the “manually define” option for setting the femoral rotational axis (Fig. 3) is chosen, an additional step needs to be performed in the work-flow, following mesh generation. The axial view of the mapped distal femur is presented to the surgeon, to manually define the anteroposterior axis of the femur (WSA), between the deepest point of the trochlear groove and the center of the inter-condylar notch (Fig. 4).
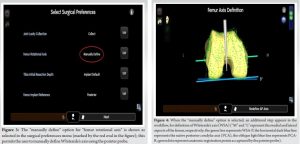
A system-generated perpendicular axis to the WSA is depicted on the interface (WSA-P), representing the resultant rotational orientation. Two posterior axes are also depicted, representing the mesh-derived PCA, and an axis parallel to WSA-P representing rotational deviation from the PCA (PCA-R). The angle between the PCA and the PCA-R is presented in real-time, and is indicative of the rotation of the WSA-P with respect to the PCA. The surgical planning menu now displays the value of FCR in relation to the WSA-P (Fig. 5). The authors modified the technique of the “manually define” option, resulting in a third method for defining the femoral rotational axis that not only uses the PCA as a reference but also permits the surgeon to calibrate FCR for a given knee and observe the effect of alterations in bony resection on FCR and vice versa. This technique involves manual positioning of the pointer probe in a manner such that the PCA-R co-aligns with the PCA, thereby presenting a rotational angle of 0° (Fig. 6).
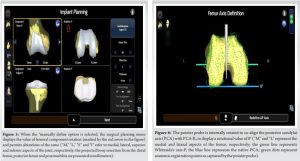
The deliberate misrepresentation of WSA is inconsequential, as the planning menu now permits fine-tuning of FCR “unwittingly” using the PCA as the reference axis, despite the use of a setting meant for WSA-P-based referencing. Intra-operative pictures of an example case depicting the execution of the technique are depicted in Fig. 7-9.
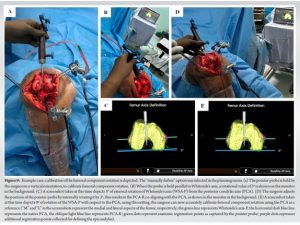
An extended use of this technique involves preliminary coalignment of the WSA-P with the mesh-derived anatomic trans-epicondylar axis (aTEA) to derive the aTEA/PCA angle (Fig. 10), followed by execution of the remaining steps as mentioned above.

This addition to the original technique is immensely relevant in the context of setting safe boundaries for FCR during functionally aligned RA-TKA. Rotational boundaries are defined with respect to the sTEA, which lies approximately 2° internally rotated from the aTEA [1,4]. The aTEA/sTEA angle is relatively constant, as it is less likely to be affected by trochlear dysplasia, femoral condylar hypoplasia, posterior condylar wear, or posteromedial femoral condyle hypertrophy [5]. It can be used to indirectly assess the sTEA/PCA angle when the aTEA/PCA angle is known. In the example shown in Fig. 10, the aTEA/PCA angle is 8°, indicating a sum total of approximately 2° from the aTEA/sTEA angle and 6° from the sTEA/PCA angle. Therefore, to set rotational boundaries of ±3° from the sTEA, the surgeon would have to consider the boundaries of the FCR as 3° and 9° of external rotation from the PCA for implants that do not have an externally rotated design (like the Legion [Smith and Nephew, Memphis, TN, USA] system used by the authors). Where components with externally rotated designs (for example, the Genesis II system [Smith and Nephew, Memphis, TN, USA]) are used, the technique remains applicable, though appropriate boundary adjustments need to be made by the surgeon. The rest of the surgery is performed customarily. Titrated bony resections to achieve optimal gap balance are planned and executed. Anteroposterior positioning of the femoral component can be adjusted during the planning process, for an appropriate posterior offset without anterior femoral notching. Soft-tissue releases are performed where necessary. Trial components are fixed in situ to assess the adequacy of the surgical procedure. Definitive implants are finally fixed.
Application of the technique: general day-to-day use
Appropriate FCR during TKA is critical for healthy patello-femoral joint mechanics, tibio-femoral joint stability, and prosthetic longevity [6]. Optimal FCR has a strong positive correlation with clinical outcomes following TKA [7]. Malrotation of the femoral component could result in numerous patellofemoral complications such as maltracking, subluxation, dislocation, wear, anterior pain syndrome, or the need for lateral retinacular release. It could also affect tibiofemoral flexion gap balance adversely and result in stiffness, instability, post-cam impingement, asymmetric compartment loading, polyethylene wear, mid-flexion pain, component loosening, or prosthetic failure [8,9]. The sTEA is considered the most reliable reference for FCR but is difficult to define intra-operatively due to soft-tissue coverage [9,10]. To overcome this impediment, the PCA and WSA are used as surrogate references for femoral rotational alignment [11]. Despite the possibility of errors with either of these references, the PCA has been shown to be associated with less variability than the WSA [11]. The use of a fixed 3° external rotation from the PCA, however, as was the general practice in the past, has been questioned in recent times [10]. The technique presented herein is simple and finds application in multiple specific case scenarios, as outlined below, apart from having the potential for routine day-to-day use. The application of this technique is primarily during the surgical steps associated with correcting mediolateral gap imbalances in flexion rather than extension, since alterations of the FCR affect the flexion gap. However, any residual extension-flexion gap mismatch following coronal plane balancing can be subsequently addressed in the planning stage through appropriate alterations of the distal femoral resection level, femoral component flexion, or posterior tibial slope. Moreover, the increased ease of obtaining flexion balance while remaining within acceptable boundaries of FCR could potentially obviate the need for posterior cruciate ligament recession or release in several patients.
Application of the technique: valgus knee deformity
Hypoplasia of the lateral femoral condyle in knees with valgus deformities is well documented in the literature [12]. It results in internal rotation of the femoral component when a fixed 3° of external rotation from the PCA is used to define the femoral rotational axis during TKA. Calibration of FCR through the use of appropriate boundaries would prevent implant mal-positioning among these knees.
Application of the technique: posterior medial femoral condyle hypertrophy
The increasing severity of knee varus deformities is associated with the incidence of posterior medial condyle hypertrophy of the femur, especially among knees with anterior cruciate ligament insufficiency [5]. Individualized titration of FCR on a case-by-case basis would prevent erroneous, internally rotated placement of the femoral component during TKA.
Application of the technique: various alignment strategies
Kinematic and restricted kinematic alignment aim to retain native femoral rotation, which varies from patient to patient [1]. Our technique results in 0° of rotation from the PCA as a starting point for performing alterations in component positioning, which would be the exact rotational alignment required in these strategies. Functional alignment uses alterations in femoral component positioning within pre-defined boundaries to attain improved gap balance [1]. The aforementioned strategies would permit the execution of functionally aligned RA-TKA.
Application of the technique: anatomic variations and outliers
The PCA is more internally rotated in relation to the sTEA among women than men [11]. The orientation of the PCA also varies across ethnic groups [13,14]. The possibility of outliers with sub-optimal knee biomechanics also exists. Assessing the relationship between the various described rotational axes of the femur in each case rather than using empirical values, and appropriately orienting component placement would prevent re-creation of inferior anatomy and could translate to superior clinical outcomes.
The technique presented by the authors is simple and finds application in specific case scenarios as well as routine use during RA-TKA. The accuracy of image-free robotic systems in terms of alignment and component positioning is well established. However, execution of the manufacturer-recommended workflow using default settings presents a limitation in practical usage, leading to suboptimal utilization of the robot. While it could be possible to address this limitation in future software updates, the alternate strategy presented herein would help surgeons calibrate FCR using the PCA as a reference for improved gap balancing in the meanwhile.
Though the sTEA is considered the most reliable reference for FCR during TKA, WSA, and the PCA continue to be used as surrogate references during conventional and image-free robot-assisted surgery. This manuscript describes a simple and useful technique with wide applicability for calibrating FCR using the posterior condylar axis as the reference during image-free RA-TKA.
References
- 1.Lustig S, Sappey-Marinier E, Fary C, Servien E, Parratte S, Batailler C. Personalized alignment in total knee arthroplasty: Current concepts. SICOT J 2021;7:19. [Google Scholar | PubMed]
- 2.Selvanathan N, Ayeni FE, Sorial R. Incidence of soft tissue releases in robotic assisted cementless TKA with mechanical alignment and flexion gap balancing. Arthroplasty 2023;5:28. [Google Scholar | PubMed]
- 3.Doan GW, Courtis RP, Wyss JG, Green EW, Clary CW. Image-free robotic-assisted total knee arthroplasty improves implant alignment accuracy: A cadaveric study. J Arthroplasty 2022;37:795-801. [Google Scholar | PubMed]
- 4.Victor J. Rotational alignment of the distal femur: A literature review. Orthop Traumatol Surg Res 2009;95:365-72. [Google Scholar | PubMed]
- 5.Eachempati KK, Parameswaran A, Apsingi S, Dannana C, Gautam D, Sheth NP. How does anterior cruciate ligament incompetence influence the varus osteoarthritic knee? J Am Coll Surg 2022;235:S62-3. [Google Scholar | PubMed]
- 6.Cho Y, Lee MC. Rotational alignment in total knee arthroplasty. Asia Pac J Sports Med Arthrosc Rehabil Technol 2014;1:113-8. [Google Scholar | PubMed]
- 7.Valkering KP, Breugem SJ, van den Bekerom MP, Tuinebreijer WE, van Geenen RC. Effect of rotational alignment on outcome of total knee arthroplasty. Acta Orthop 2015;86:432-9. [Google Scholar | PubMed]
- 8.Castelli CC, Falvo DA, Iapicca ML, Gotti V. Rotational alignment of the femoral component in total knee arthroplasty. Ann Transl Med 2016;4:4. [Google Scholar | PubMed]
- 9.Song SJ, Lee HW, Kim KI, Park CH. Appropriate determination of the surgical transepicondylar axis can be achieved following distal femur resection in navigation-assisted total knee arthroplasty. Knee Surg Relat Res 2021;33:41. [Google Scholar | PubMed]
- 10.Gurava Reddy AV, Mathur RK, Mugalur A, Eachempati KK, Reddy A. Reference axes for optimal femoral rotational alignment in varus osteoarthritic Indian knees - A CT based study. J Clin Orthop Trauma 2016;7:215-9. [Google Scholar | PubMed]
- 11.Patel AR, Talati RK, Yaffe MA, McCoy BW, Stulberg SD. Femoral component rotation in total knee arthroplasty: An MRI-based evaluation of our options. J Arthroplasty 2014;29:1666-70. [Google Scholar | PubMed]
- 12.Rossi R, Rosso F, Cottino U, Dettoni F, Bonasia DE, Bruzzone M. Total knee arthroplasty in the valgus knee. Int Orthop 2014;38:273-83. [Google Scholar | PubMed]
- 13.Murgier J, Chantalat É, Li K, Chiron P, Telmon N, Huang W, et al. Distal femoral torsion: Differences between caucasians and asians. A multicentre computed tomography study of 515 distal femurs. Orthop Traumatol Surg Res 2018;104:997-1001. [Google Scholar | PubMed]
- 14.Mullaji AB, Sharma AK, Marawar SV, Kohli AF, Singh DP. Distal femoral rotational axes in Indian knees. J Orthop Surg (Hong Kong) 2009;17:166-9. [Google Scholar | PubMed]