This report focuses on the potential link between TKA and the development of a popliteal cyst, with the importance of recognizing that surgical procedures themselves can precipitate cyst development when presenting and interacting with multiple other factors such as pre-existing medical conditions and/or infections.
Dr. Ramy Samargandi, Department of Orthopedic Surgery, Hôpital Trousseau, CHRU de Tours, Avenue de la République, Chambray-Lès-Tours, 37044 Tours Cedex 9, France, Faculté de Médecine, université de Tours, France. E-mail: ramy.samargandi@hotmail.com
Introduction: A popliteal cyst, or Baker’s cyst, is often associated with joint diseases such as osteoarthritis and rheumatoid arthritis (RA). It is rare for these cysts to develop following total knee arthroplasty (TKA), but understanding when and why they might can optimize patient care. Presented here is a unique case of a massive, chronically recurring infected popliteal cyst in a patient with RA and prior TKA, shedding light on an unusual complication worth attention in the orthopedic literature.
Case Report: In this case, the patient had longstanding, difficult-to-treat RA. Following left TKA, the patient developed a painful popliteal cyst, leading to hospitalization in 2023. Microbiological analysis identified Staphylococcus lugdunensis as the infectious agent despite negative mycobacterial and mycological cultures. Surgical intervention involved a one-stage procedure, encompassing resection of the extensive thigh cyst and prosthesis replacement. Notably, the cyst reached an unprecedented size, measuring 32 cm at its peak, presenting a unique challenge in management.
Conclusion: This case report contributes significantly to orthopedic literature by highlighting the intricate interplay between joint pathologies, surgical interventions, and infections. It highlights the importance of multidisciplinary collaboration in managing complex musculoskeletal conditions. The rarity of a massive and infected popliteal cyst post-TKA emphasizes the need for heightened vigilance in patient care post-surgery. Furthermore, this case report serves as a valuable addition to the understanding of potential complications associated with TKA, offering insights that may inform future treatment strategies and optimize patient outcomes in orthopedic practice.
Keywords: Cyst, arthroplasty, infection, knee, post-operative complication, soft-tissue mass.
Popliteal cysts, also known as Baker’s cysts, are fluid cystic formations that typically arise from the posterior aspect of the knee joint. The common belief is that they are caused by traumatic or pathological and inflammatory conditions related to the joint, such as meniscal tears, anterior cruciate ligament tears, osteoarthritis, and rheumatoid arthritis (RA). These pathologies can cause excess synovial fluid to accumulate within the cyst [1]. In parallel, total knee arthroplasty (TKA) is a widely practiced orthopedic procedure in patients with severe knee joint degeneration to alleviate pain and restore functional capacity [2]. The intersection between these two entities resides in the potential emergence of cysts as a post-operative complication following TKA. While cysts are a rare occurrence after TKA, they are still present [3-5]. The surgical procedure itself may disrupt the normal synovial environment of the knee joint, potentially triggering cysts [4,6]. In this report, we present the case of a patient who after undergoing a total knee replacement procedure not only developed a joint infection years later but also presented with a massive chronically reoccurring infected popliteal cyst.
The patient’s medical history began in 1998 with a diagnosis of RA, marked by inflammatory joint pain primarily affecting the knees and later involving the hands. Laboratory findings indicated positive rheumatoid factor and negative anti-cyclic citrullinated peptide antibodies. Over the years, various therapeutic modalities were employed to manage the disease, including methotrexate, leflunomide, humira, and JAK inhibitors. Despite these treatments, the patient’s RA remained challenging to control. In October 2018, a primary left total knee replacement was performed to address gonarthrosis and a 17° valgus deformity using the Keblish approach. It should be noted that the extensor mechanism was chronically dislocated laterally. However, in 2020, a new complication emerged in the form of a painful popliteal cyst localized in the left knee. The cyst, initially small in size, gradually extended into the posterior aspect of the thigh and descended into the gastrocnemius muscle over the course of many months despite multiple therapeutic attempts. Initial interventions, including aspiration and injections, provided only partial and transient relief.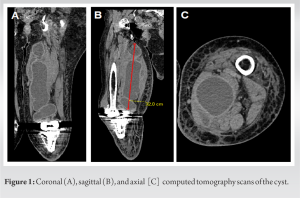
On April 2023, the patient’s condition deteriorated, necessitating hospitalization. Knee aspiration of the thigh cyst was performed, and microbiological analysis identified Staphylococcus lugdunensis, despite, initially notably, having negative mycobacterial and mycological cultures. The presence of this infectious agent prompted discussions within a multidisciplinary team, including rheumatologists, orthopedic surgeons, and infectious disease specialists.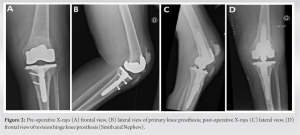
Clinical examination revealed inflammatory joint pain in the knees, shoulders, elbows, and wrists, attributed to the pre-existing RA, although no objective swelling was observed except for the lesion on the posterior left thigh. Yet despite these symptoms, there were no systemic or local signs of infection present. Laboratory tests indicated normal white blood cell counts of 8.75 G/L (normal range: 4–10 G/L) and neutrophil counts of 7.1 G/L (normal range: 1.5–7.5 G/L) but showed an elevated level of C-reactive protein level of 178.3, reflecting the ongoing inflammatory process. The disease activity score was 5.34, indicating strong disease activity. A series of four blood culture were done and were negative. Radiographic computed tomography (CT) scan examinations highlighted the presence of a multilobulated cyst measuring over 32 cm in the superoinferior axis on a CT scan from May 2023 while there were not any signs of prosthetic loosening (Fig. 1). Magnetic resonance imaging was not performed due to the patient’s claustrophobia. Given the patient’s complex medical history, including advanced RA and respiratory insufficiency, a challenging decision needed to be made regarding the surgical approach. Ultimately, after extensive discussions with the patient, a one-stage procedure was chosen. This involved the resection of the extensive cyst and the replacement of the total knee prosthesis all at once. Due to joint laxity and extensor mechanism failure, TKA with a constrained hinged design was implanted.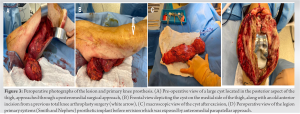
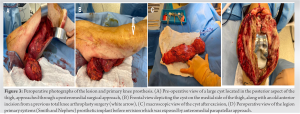
The first stage of the operation involved the resection of the thigh cyst. A longitudinal incision was made just in front of the gracilis muscle. Care was taken to preserve the great saphenous vein. The fascia lata was opened, and dissection proceeded, carefully separating the cystic lesion from surrounding tissues. The lesion extended into various muscle compartments, necessitating meticulous dissection to release it. Superficial femoral vessels were spared to minimize the risk of seroma formation. Clipping and sectioning of the descending genicular artery were performed. The tendon of the great adductor was preserved, and the lesion was detached from the ischium. The lesion was then carefully removed, ligated, and sent for histopathological examination (Fig. 2 and 3). Bacteriological samples were taken, and the area was thoroughly washed and rinsed before closure. The second stage involved a one-stage prosthetic replacement and synovectomy. The surgical procedure was done by a lateral parapatellar arthrotomy. Serous fluid and extensive synovitis were observed. A partial synovectomy was performed, and synovial fluid samples were collected. The polyethylene was removed, and the femoral and tibial components were carefully extracted. Minimal bone loss was observed. After thorough cleaning and preparations, trial implants were placed to assess the joint’s stability. Tibia and femur preparations were carried out, and the final prosthetic components were implanted (Fig. 2). The extensor mechanism was checked for integrity, and the knee was stabilized and closed.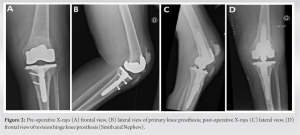
Postoperatively, the patient’s course remained uneventful. Full weight-bearing was resumed with the use of a brace, and passive flexion on the arthromotor was achieved up to 60°. Medications included pain relievers and prophylactic anticoagulation with low-molecular-weight heparin for 45 days, with weekly platelet monitoring. Antibiotic therapy consisted of RIFAMPICIN 600 mg once daily and LEVOFLOXACIN 500 mg once daily for 3 months. Microbacterial cultures remained negative post-surgery and histopathological examination of the cyst contents ruled out malignancy. The patient underwent regular clinical follow-ups, with no signs of cyst recurrence or infection observed in the clinical examination during the past follow-up at 10 months.
While Baker’s cysts are frequently associated with joint pathologies such as osteoarthritis and RA, surgical intervention is rarely mentioned in literature as a contributing factor. When a knee joint has suffered severe degeneration, TKA can alleviate pain and restore function. However, the disruption of the normal synovial environment during TKA may have some consequences. It is essential to consider whether the surgical manipulation and alteration of the knee’s anatomical structures, combined with the pre-existing RA, might have contributed to the formation of the cyst. RA poses significant challenges in its management, especially when it resists various therapeutic modalities. The patient’s long-standing and challenging-to-control RA undoubtedly played a significant role in this case. The risk of complications after TKA in RA patients is relatively higher, because soft tissue is less likely to heal, deep wound infections are more common, pre-operative joint deformity and laxity is severe, bone stock is low, and multiple joints are involved, making rehabilitation difficult [7]. Deep wound infections could be the most important complication affecting TKA results in RA patients [8]. The chronic inflammation and synovitis characteristic of RA can trigger the production of excess synovial fluid, potentially exacerbating cyst formation [9]. Moreover, the patient’s history of failed treatments, including Methotrexate, Leflunomide, Humira, and JAK inhibitors, exemplifies the ongoing struggle to manage the disease. The massive size of the popliteal cyst is an extremely unusual feature of this case. This cyst extended into multiple compartments measuring 32 cm at one point, spanning from the thigh to the leg, defying the typical anatomical boundaries associated with Baker’s cysts. The reasons behind such extensive cyst growth could include but are not limited to, prolonged inflammation, persistent joint pathology, and complications related to the TKA procedure. This exceptionally large and compartmentally extensive cyst is a rare manifestation of a relatively common condition, adding a layer of complexity to the clinical presentation. Infection is a central element in this case, both regarding joint and cyst. However, definitively attributing the primary cause among factors such as RA, infection, or the cyst itself remains a complex challenge. It is possible that any of which caused the other, and the possibility of their simultaneous occurrence within this scenario warrants consideration. The isolation of S. lugdunensis raises questions about the origin and progression of the infection. This bacterium, though relatively rare, is known for its virulence and propensity to cause infections, particularly in prosthetic joints of the knee [10]. The isolation of this bacterium prompts further questions about its source and its role in the chronicity of the cyst. The enigmatic nature of the infection, in this case, is further compounded by the negative mycobacterial and mycological cultures. Along with the equally perplexing absence of both local and systemic signs of infection around the knee joint, a phenomenon rarely encountered in such cases. This atypical presentation challenges conventional clinical expectations and highlights the need for vigilance in diagnosing and managing musculoskeletal infections. The chronic and recurrent nature of the popliteal cyst in this case adds yet another layer of complexity. Despite multiple therapeutic attempts, including aspiration and injections, the cyst persisted over time. This recurrence may be attributed to underlying joint pathologies, persistent inflammation, or complications related to previous interventions. Similar cases have been mentioned before in the literature, some where patients formed cyst after TKA, others where patients had RA [3,4,9]. The cases mentioned in the literature involved cysts that though large, hardly actually compare to the size of the cyst presented in this case. What makes this case unique is its complexity, involving multiple factors, all of which could be equally held accountable.
Following TKA, Baker’s cysts developed along with an infection of the prosthetic implant, highlighting the complexity in treating complex orthopedic and rheumatological conditions. Further emphasis is placed on the nature of this case due to the lack of signs of infection. Therefore, we are again reminded of the importance of multidisciplinary collaboration and tailor-made approaches. The case emphasizes the importance of considering long-term outcomes and exploring alternative treatment modalities for challenging cases, all in hopes of achieving the best possible outcomes in such complex medical situations.
This case emphasizes the intricate interplay between joint pathologies, surgical procedures, and infections as well as the importance of multidisciplinary collaboration and personalized approaches to patient care.
References
- 1.Herman AM, Marzo JM. Popliteal cysts: A current review. Orthopedics 2014;37:e678-84. [Google Scholar | PubMed]
- 2.NIH Consensus Panel. NIH Consensus Statement on total knee replacement December 8-10, 2003. J Bone Joint Surg Am 2004;86:1328-35. [Google Scholar | PubMed]
- 3.Tofte JN, Holte AJ, Noiseux N. Popliteal (Baker’s) cysts in the setting of primary knee arthroplasty. Iowa Orthop J 2017;37:177-80. [Google Scholar | PubMed]
- 4.Niki Y, Matsumoto H, Otani T, Yoshimine F, Inokuchi W, Morisue H. Gigantic popliteal synovial cyst caused by wear particles after total knee arthroplasty. J Arthroplasty 2003;18:1071-5. [Google Scholar | PubMed]
- 5.Akisue T, Kurosaka M, Matsui N, Yamaguchi M, Hasuda K, Bauer TW, et al. Paratibial cyst associated with wear debris after total knee arthroplasty. J Arthroplasty 2001;16:389-93. [Google Scholar | PubMed]
- 6.Moretti B, Patella V, Mouhsine E, Pesce V, Spinarelli A, Garofalo R. Multilobulated popliteal cyst after a failed total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2007;15:212-6. [Google Scholar | PubMed]
- 7.Kim JW, Suh CH. Systemic manifestations and complications in patients with rheumatoid arthritis. J Clin Med 2020;9:2008. [Google Scholar | PubMed]
- 8.Lee JK, Choi CH. Total knee arthroplasty in rheumatoid arthritis. Knee Surg Relat Res 2012;24:1-6. [Google Scholar | PubMed]
- 9.Adiyeke L, Bılgın E, Duymus TM, Ketencı İE, Ugurlar M. Giant Baker’s cyst associated with rheumatoid arthritis. Case Rep Orthop 2017;2017:4293104. [Google Scholar | PubMed]
- 10.Lourtet-Hascoët J, Bicart-See A, Félicé MP, Giordano G, Bonnet E. Staphylococcus lugdunensis, a serious pathogen in periprosthetic joint infections: Comparison to Staphylococcus aureus and Staphylococcus epidermidis. Int J Infect Dis 2016;51:56-61. [Google Scholar | PubMed]





