Osteochondroma is a tumor that can present in atypical locations and a high index of suspicion is required to diagnose it accurately.
Dr Prajwal Anand Srinivasan, Department of Orthopedics, St Helen and Knowsley NHS Trust, Warrington Road, Prescot, England. E-mail: prajwal.srinivasan@sthk.nhs.uk
Introduction: Osteochondroma (OC) is a common benign bone tumor that usually arises from the metaphyseal region of long bones. Rarely, it can present in atypical locations such as the wrist and posing diagnostic challenges.
Case Report: We present a 42-year-old female with an incidental finding of OC on the volar aspect of the right wrist. The patient was referred for a musculoskeletal assessment due to a painful swelling, which was slowly increasing in size over 2 years, following mild trauma. With a suspicion of ganglion, investigations including X-ray and ultrasound led to surgical excision and histological examination, which confirmed a diagnosis of a benign OC.
Conclusion: The case emphasizes the importance of considering OC in the differential diagnosis of wrist swellings and highlights the effectiveness of surgical intervention in resolving symptoms.
Keywords: Osteochondroma, wrist, ganglion.
Osteochondroma (OC) is a common benign bone tumor that usually arises from the metaphyseal region of long bones. Rarely, it can present in atypical locations such as the wrist, posing diagnostic challenges. It typically affects adolescents and young adults and may present as a painless mass; however, symptoms can arise due to mass effect on adjacent structures. This report underscores the significance of a thorough assessment and tailored management strategy for atypical presentations of OC [1].
The patient, a 42-year-old female, was referred to a musculoskeletal assessment clinic by her general practitioner due to concerns regarding a swelling on the volar aspect of her right wrist. This swelling had been gradually increasing in size over the past 2 years and was associated with pain. The patient recounted a history of mild trauma to the wrist, which she believed might have precipitated or contributed to the swelling. Despite the slow but progressive increase in size, the swelling’s dimensions fluctuated without following a discernible pattern and never completely subsided. Notably, the patient denied any significant use of anticoagulants or the presence of other similar swellings elsewhere on her body. There was no evidence of systemic symptoms such as hypercalcemia.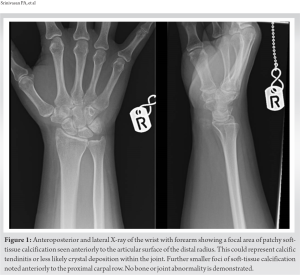
Her medical history was significant for several conditions, including a hiatus hernia, Barrett’s esophagus, and a previously identified breast lump that was determined to be non-malignant after thorough investigation. There was no notable family history of malignancy, which could suggest a genetic predisposition to certain types of tumors.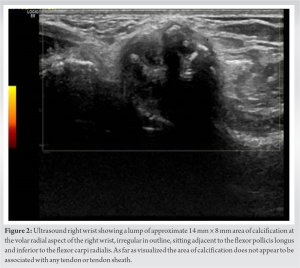
On clinical examination, the swelling was found to be well-defined, localized to the volar and radial compartment of the wrist, extending up to the first dorsal space. It was tender on palpation but was characterized as mobile and not adherent to underlying structures. Furthermore, the swelling was neither warm to the touch nor capable of transillumination, characteristics that could suggest an infectious or cystic nature [2].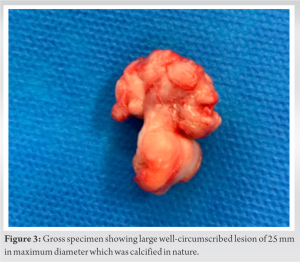
The patient’s pain was mainly localized but did not exhibit a specific pattern that could easily point to a singular diagnosis. The complexity of her symptoms and the physical characteristics of the swelling necessitated further investigation to arrive at a precise diagnosis and formulate an appropriate management plan. The initial concern, given the patient’s history and presentation, was oriented toward conditions that could manifest in similar fashions, such as ganglion cyst and tendinitis. The decision to proceed with imaging was driven by the need to elucidate the nature of the swelling and to inform the subsequent steps in her care.
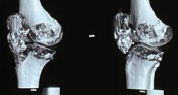
Initial X-rays showed soft-tissue calcification anterior to the distal radius’s articular surface (Fig. 1). An ultrasound identified a 14 × 8 mm calcification at the volar and radial aspect of the wrist, not involving tendons sitting below the flexor carpi radialis (FCR) and adjacent to flexor pollicis longus (FPL) not involving any tendon or tendon sheath (Fig. 2). Blood results revealed normal infection and inflammation markers, Vitamin-D, and calcium levels. A differential of possible ganglion cyst was made and the findings prompted surgical excision under general anesthesia for further evaluation.
Differential diagnosis
Differential diagnoses considered at that point of time was calcific tendinitis and ganglion cyst. The clinical presentation and imaging studies suggested a calcified mass, leading to surgical intervention for definitive diagnosis.
Treatment
The patient underwent an excision biopsy under general anesthesia. MRI was not considered before surgery as the swelling size was small and did not meet the criteria for a soft-tissue sarcoma referral or workup as per regional trust guidelines. Henry’s approach was used, with careful dissection revealing a well-encapsulated lesion radial to the FCR and under the FPL, not attached to the bone. The lesion was removed in toto, with the site thoroughly irrigated, and the patient discharged home neurovascularly intact. The lesion was sent for histopathology and no perioperative complications were noted.
Outcome and follow-up
Histological analysis confirmed a benign OC, characterized by a large well-circumscribed lesion of 25 mm in maximum diameter comprising a cap of well-differentiated hyaline cartilage in continuity with mature bone (Fig. 3). The patient’s post-operative course, reviewed at 2 weeks, was uneventful, with complete resolution of symptoms and no requirement for further analgesia. Although a follow-up plan was provided at 6- and 12-month period, the patient was lost to follow-up, likely due to symptom resolution. She has hence now been discharged to the community with a patient-initiated follow-up for review if symptoms represent.
OCs are benign bone tumors characterized by their cartilage-capped bony projections stemming from the metaphysis of long bones, most commonly affecting the distal femur, proximal tibia, and humerus [3]. Their occurrence in the wrist is relatively rare, which can present a diagnostic and therapeutic challenge due to the anatomical complexity and the need to preserve function in this region. The case of a 42-year-old female with an incidental OC of the wrist underscores several important considerations in the management of such atypical presentations [4]. First, the differential diagnosis for wrist swellings is broad, encompassing various benign and malignant conditions, including ganglion cysts, giant cell tumors of the tendon sheath, and soft-tissue sarcomas. In this context, OC must be considered, particularly in patients presenting with a slowly enlarging mass, pain, or functional impairment. Advanced imaging modalities play a crucial role in narrowing down the differential diagnoses [5]. While X-rays provide initial insights into the presence of calcification or bone involvement, ultrasound, and magnetic resonance imaging can offer detailed information regarding the lesion’s relation to soft tissue and its internal characteristics. Hence, need for additional soft tissue imaging should always be considered in lesions with suspicious morphology. It is of great importance that we have a high suspicion for soft tissue tumors in benign case presentations. This case emphasizes the utility of a multimodal imaging approach in formulating a precise diagnosis[6]. Surgical excision is the mainstay of treatment for symptomatic OCs or when there is uncertainty regarding the nature of the mass. The surgical approach must be carefully planned to minimize damage to surrounding structures while ensuring complete removal of the lesion. The successful outcome in this case, with the patient becoming symptom-free postoperatively, highlights the efficacy of surgical intervention. Histopathological examination post-excision serves a dual purpose of confirming the diagnosis and ruling out malignant transformation, which, although rare, represents a significant concern with OCs[7]. The literature supports the notion that complete surgical resection of OC generally results in excellent outcomes, with low recurrence rates and high levels of patient satisfaction. However, the risk of recurrence, although minimal, necessitates a structured follow-up, especially in growing children and in cases where the resection margins are close or uncertain[8]. This case also draws attention to the importance of a comprehensive approach that integrates clinical assessment, imaging, and surgical expertise. It underscores the need for awareness of less common presentations of common conditions and the value of a multidisciplinary team in managing complex musculoskeletal tumors [9,10].
The management of atypical OC of the wrist, as demonstrated in this case, requires a nuanced understanding of the condition, a thorough diagnostic workup, and meticulous surgical planning. This case contributes to the body of evidence supporting surgical excision as a definitive and curative treatment for OC, emphasizing the role of histopathology in confirming the diagnosis and guiding post-operative care. Future research and case reports will continue to refine our understanding of atypical presentations and optimize management strategies for OC and similar lesions.
- OC, although common, can present atypically in locations such as the wrist, challenging clinicians.
- A thorough clinical and diagnostic workup is crucial for accurate diagnosis, particularly when the presentation deviates from the norm.
- Surgical excision of OC, even in atypical locations, can result in complete symptom resolution and has a low rate of recurrence.
- Post-operative follow-up is essential, though patient’s symptom-free after successful treatment may not perceive the need for further medical attention.
References
- 1.Murphey MD, Choi JJ, Kransdorf MJ, Flemming DJ, Gannon FH. Imaging of osteochondroma: Variants and complications with radiologic-pathologic correlation. Radiographics 2000;20:1407-34. [Google Scholar | PubMed]
- 2.Bovée JV. Multiple osteochondromas. Orphanet J Rare Dis 2008;3:3. [Google Scholar | PubMed]
- 3.Woertler K. Benign bone tumors and tumor-like lesions: Value of cross-sectional imaging. Eur Radiol 2010;20:1927-41. [Google Scholar | PubMed]
- 4.Malghem J, Vande Berg B. Tumors and tumor-like lesions of the bone. In: Imaging of Bone Tumors and Tumor-Like Lesions: Techniques and Applications. Berlin, Heidelberg: Springer; 2008. p. 75-110. [Google Scholar | PubMed]
- 5.Hameetman L, Szuhai K, Yavas A, Knijnenburg J, van Duin M, van Dekken H, et al. The role of EXT1 in nonhereditary osteochondroma: Identification of homozygous deletions. J Natl Cancer Inst 2007;99:396-406. [Google Scholar | PubMed]
- 6.Peterson HA. Deformities and problems of the forearm in children with multiple hereditary osteochondromata. J Pediatr Orthop 1989;9:543-53. [Google Scholar | PubMed]
- 7.Schmale GA, Conrad EU 3rd, Raskind WH. The natural history of hereditary multiple exostoses. J Bone Joint Surg Am 1994;76:986-92. [Google Scholar | PubMed]
- 8.Kitsoulis P, Galani V, Stefanaki K, Paraskevas G, Karatzias G, Agnantis NJ, et al. Osteochondromas: Review of the clinical, radiological and pathological features. In Vivo 2008;22:633-46. [Google Scholar | PubMed]
- 9.Garrison RC, Unni KK, McLeod RA, Pritchard DJ, Dahlin DC. Chondrosarcoma arising in osteochondroma. Cancer 1982;49:1890-7. [Google Scholar | PubMed]
- 10.Pierz KA, Stieber JR, Kusumi K, Dormans JP. Hereditary multiple exostoses: One center’s experience and review of etiology. Clin Orthop Relat Res 2002;401:49-59. [Google Scholar | PubMed]