Minimally invasive spinal tumor resection, using a tubular retractor, spares muscles, reduces morbidity, and enables a quicker return to work and activities.
Dr. Jonathan Carmouche, Department of Orthopaedic Surgery, Carilion Clinic Institute for Orthopaedics and Neurosciences 2331 Franklin Road SW, Roanoke, Virginia, United States of America. E-mail: jjcarmouche@carilionclinic.org
Introduction: Open surgical resection involves extended recovery and soft-tissue damage, prompting the development and increasing adoption of less invasive techniques. While Mast Quadrant tubular retractors have been used in spine fusion and endoscopic procedures, their application in minimally invasive tumor resections has not been widely discussed. This report showcases the use of a Mast Quadrant tubular retractor for the minimally invasive resection of a lumbar vertebral body osteoid osteoma.
Case Report: A 38-year-old Caucasian man, suffering from six years of lumbar pain and refractory osteoid osteoma, underwent resection using a minimally invasive lateral approach with a Mast Quadrant tubular retractor. This came after the failure of less invasive treatment modalities, including facet injections and radiofrequency facet ablation.
Conclusion: Vertebral body osteoid osteomas can be resected with no recurrence using a tubular retractor to spare paravertebral muscles and the morbidity of open resection, allowing patients an earlier return to work and activity.
Keywords: Osteoid osteoma, minimally invasive, spine, tumor, tubular retractor, lumbar, case report, vertebral body.
Osteoid osteomas are benign, osteoblastic tumors, measuring <1.5 cm in size [1,2], affecting mainly males under 40 years old. They are commonly found in the cortices of long bones and makeup about 2–3% of all bone tumors and 11% of benign bone tumors [3-5]. In the spine, where they occur 10% of the time, they are most often seen in the lumbar region, followed by the cervical and thoracic regions in the posterior elements [2,5,6]. When present in the vertebral column, these tumors can induce muscle spasms due to pain and inflammation, potentially leading to scoliosis [7]. The classic clinical presentation includes nocturnal pain, which responds to non-steroidal anti-inflammatory drugs (NSAIDs) [8,9]. Although most osteoid osteomas regress within 5–7 years, pain resolution often occurs after about three years of NSAID therapy, and enduring such symptoms for that duration may be challenging, and long-term NSAID use can lead to complications [7,9]. When NSAID therapy fails, alternative options such as radiofrequency ablation, thermal ablation, or surgical resection are considered [10]. However, wide block surgical resection, the standard of care after failed NSAID therapy, is not without disadvantages and carries a significant risk of complications [1,2]. Open surgical resection requires lengthy recovery periods and involves damage to surrounding soft tissues. Consequently, less invasive surgical techniques have been developed. This report presents the successful management of a patient with progressive back pain attributed to a lumbar vertebral body osteoid osteoma that was unresponsive to routine treatment, including computed tomography (CT) guided radiofrequency ablation. The patient was effectively treated through a minimally invasive lateral approach and tubular retractor.
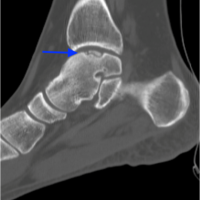
A 38-year-old Caucasian man presented with a 6-year history of persistent lower back pain, most severe in the morning with improvement throughout the day. His medical history included type 1 diabetes and lumbosacral muscle strain from two motor vehicle accidents (MVA). X-rays after both MVAs, six and five years before his presentation, showed stable lumbar arthropathy, L4-L5 degeneration with disc height loss, and no fractures, dislocations, or lesions (Fig. 1 and 2).
He received conservative pain management: NSAIDs, rest, heat, ice, transcutaneous electrical nerve stimulation, epidural steroid injections, and physical therapy. However, after the second MVA, the pain persisted. He trialed muscle relaxers and opioids, as well as lumbar facet injections targeting L4-L5, and CT-guided radiofrequency facet ablation of L2-5. These procedures initially resulted in a 75% and 25% reduction in back pain, respectively, but the relief was temporary. Subsequent single-photon emission CT (SPECT-CT) revealed increased uptake and vertebral degeneration at the superior endplate on the left side of the L5 vertebral body. CT-scan showing the typical feature was considered conclusive for osteoid osteoma (Fig. 3 and 4). Two CT-guided biopsies were performed at 1 and 4 months after the scan confirming the diagnosis.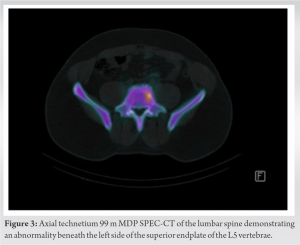
After six years of pain and exhausting non-surgical options, the patient was counseled on surgical alternatives, including their associated risks and benefits. Following informed consent, a partial vertebrectomy was performed, guided by pre-operative magnetic resonance imaging (MRI) in addition to the SPECT-CT (Fig. 5 and 6).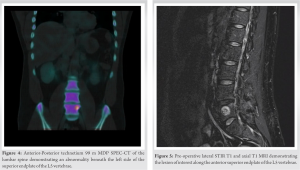
The patient was placed in the right lateral decubitus position. A one-inch oblique incision was made over the left flank, down to the external oblique fascia, which was divided. Blunt dissection through the internal oblique and transverse abdominus positioned an expandable tubular retractor anterior to the psoas muscle, exposing the L4-L5 vertebral bodies and disc space. The lesion was located below the L4-L5 disc space in the superior portion of the L5 vertebral body. Using a minimally invasive tubular retractor, we accessed the lesion around the lower part of the L4-L5 disc space, reaching the superior aspect of the L5 vertebral body for resection.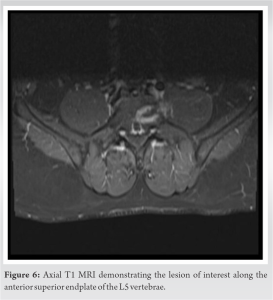
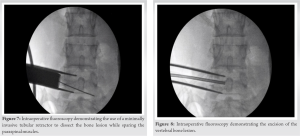
The retractor was carefully placed and docked on the lateral border of the L4-5 disc space to target the L5 lesion. Neurologic monitoring ensured safety during the procedure. Minimal facet and disc degeneration negated the need for spinal fusion. We carefully entered the lesion using a high-speed drill, osteotomes, and curettes, avoiding injury to the healthy disc. The excised lesion was sent for pathology, borders debrided, and the cavity was packed with cancellous allograft. The surgical site was closed, and the patient was discharged on the same day without complications (Fig. 7 and 8).
At the 2-week follow-up, the patient had mild discomfort at the surgical site. After 6 weeks, due to the muscle-sparing technique and no fusion requirement, he returned to full duty without immobilization. By the 3-month post-operative appointment, he engaged in regular exercise with minimal pain. During the 18-month follow-up, he reported sustained pain relief following the removal of the lesion. At the 2-year mark, he developed lower back and left lateral thigh pain. A repeat MRI showed worsening disc degeneration, but no lesion recurrence (Fig. 9 and 10). Lumbar spondylosis was identified as the cause, and he was referred for facet injections. The facet injections provided adequate relief, and the patient expressed overall satisfaction with the treatment outcome.
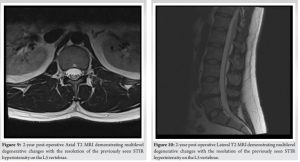
Osteoid osteomas, though benign, can lead to substantial symptoms. These lesions arise from excessive osteoblastic growth and are primarily found in long bones, and to a lesser extent the spine, where they occur 10% of the time and mostly in the posterior elements [2,5]. Osteoid osteomas form where osteoid is deposited at a faster rate than it can calcify, resulting in the formation of a central osteoid nidus. Surrounding this nidus is a reactive area of vascular tissue and fibrotic bone with increased expression of cyclooxygenase and prostaglandins, which contribute to pain and muscle spasms [10,11]. Osteoid osteomas are initially managed by imaging and biopsy to confirm their benign nature and locate them. In this case, imaging revealed degenerative changes at L4-L5 and a lytic growth on the posterior superior portion of the L5 vertebra, making osteoblastoma or aneurysmal cyst less likely. If the patient’s pain is well-controlled with NSAIDs and no complications arise, monitoring the tumor for growth is a viable approach [4]. In cases where vertebral osteoid osteomas lead to scoliosis or nerve impingement, or when non-invasive approaches prove ineffective, more invasive treatments become necessary [10]. Initially, radiofrequency ablation or cryoablation are preferred interventions. However, if ablation proves unsuccessful, the lesion is located near the skin or nerve or is causing painful scoliosis [5], surgical resection is considered the next option. In our case, the patient’s history of back pain and the lack of improvement with previous therapies, including ablation, led to the indication for surgical resection. Resecting vertebral osteoid osteomas presents challenges due to their proximity to neurovascular structures and the need for deep dissection. Traditionally, the preferred method has been open en-bloc resection through a posterior approach [10], but this can lead to complications like weight-bearing restrictions, muscle atrophy, post-operative kyphosis, discomfort, and bone weakening, and additional interventions such as bone grafting, internal fixations, or post-operative immobilization may be required [12-15]. However, the en bloc resection approach has fallen out of favor due to higher complication rates. The popularity of minimally invasive approaches has increased due to their demonstrated lower complication rates [16-18]. For our case, we opted for a minimally invasive technique using a Mast Quadrant tubular retractor for tumor resection. This approach, guided by imaging, offers the advantage of shorter recovery time, and causes less tissue damage, as supported by recent studies [19,20]. In addition, the use of the Mast Quadrant tubular retractor in the resection of an osteoid osteoma endoscopically has been described by Amendola et al. [21]. The available evidence on minimally invasive tubular retractors for spinal tumor removal is limited, but it indicates that these systems can offer sufficient exposure while causing minimal trauma to paraspinal structures, resulting in favorable patient outcomes compared to the open technique [20, 22-24]. Particularly in experienced hands, the Mast Quadrant retractor can specifically minimize disruption to spinal and paraspinal structures, thereby reducing alterations in spinal biomechanics [24]. In addition, when employed in minimally invasive transforaminal lumbar or cervical interbody fusion [22], the Mast Quadrant retractor has shown potential benefits, including shorter post-operative recovery times and improved muscle relaxation of the multifidus muscle. However, it may require a longer fluoroscopy time for successful implementation [20]. In our case, we used a minimally invasive lateral approach with a retractor to access the L4-L5 vertebral bodies, prioritizing paravertebral muscle preservation. The surgery resulted in minimal lower back pain and only a slight reduction in range of motion, showcasing a notable advantage of this lateral minimally invasive approach-minimal approach-related pain. Within 2 weeks, the patient regained complete range of motion, returned to full work duty in 6 weeks, and resumed regular exercise within 3 months. These recovery milestones align with projected recovery times reported in the literature for minimally invasive approaches using tubular retractors [17,19,22]. Two years have passed since the surgery, and during this period, there has been no recurrence of the lesion or pain, indicating the efficacy of the resection procedure. The diagnostic pathology also confirmed that the lesion was adequately removed, and the patient’s pre-operative symptoms have not resurfaced. It is worth noting that the patient had a known case of disc degeneration at L4-L5, which was partially managed with injections, NSAIDs, heating pads, and walking.
This report serves as a compelling demonstration to spine surgeons of the successful utilization of a minimally invasive lateral approach for tumor resection, which leads to notably reduced recovery times and favorable patient outcomes.
This report underscores the success of employing a minimally invasive approach, utilizing the Mast Quadrant tubular retractor, for spinal tumor resection, offering a compelling alternative to open resection. Traditional open surgery entails longer hospital stays, greater blood loss, extended recovery periods, and more tissue damage. While Mast Quadrant tubular retractors have found utility in spinal fusions and endoscopic procedures, their application in minimally invasive tumor resection has been relatively unexplored. This innovative approach and technique hold significant promise for reducing morbidity, hastening recovery, and enhancing patient outcomes.
References
- 1.Ren X, Yang L, Duan XJ. Three-dimensional printing in the surgical treatment of osteoid osteoma of the calcaneus: A case report. J Int Med Res 2017;45:372-80. [Google Scholar | PubMed]
- 2.Jaffe HL. Osteoid-osteoma: A benign osteoblastic tumor composed of osteoid and atypical bone. Arch Surg 1935;31:709-28. [Google Scholar | PubMed]
- 3.Gaike C, Lalwani K, Panat M. Osteoid osteoma of lumbar vertebra presenting as low back ache and scoliosis in a young child - A case report. J Orthop Case Rep 2022;12:95. [Google Scholar | PubMed]
- 4.Tepelenis K, Skandalakis GP, Papathanakos G, Kefala MA, Kitsouli A, Barbouti A, et al. Osteoid Osteoma: An updated review of epidemiology, pathogenesis, clinical presentation, radiological features, and treatment option. In vivo 2021;35:1929-38. [Google Scholar | PubMed]
- 5.Ghanem I. The management of osteoid osteoma: Updates and controversies. Curr Opin Pediatr 2006;18:36-41. [Google Scholar | PubMed]
- 6.Yokouchi M, Nagano S, Shimada H, Nakamura S, Setoguchi T, Kawamura I, et al. Early complete remission of osteoid osteoma with conservative medical management. Pediatric Rep 2014;6:5311. [Google Scholar | PubMed]
- 7.Akbarnia BA, Rooholamini SA. Scoliosis caused by benign osteoblastoma of the thoracic or lumbar spine. J Bone Joint Surg Am 1981;63:1146-55. [Google Scholar | PubMed]
- 8.Etemadifar MR, Hadi A. Clinical findings and results of surgical resection in 19 cases of spinal osteoid osteoma. Asian Spine J 2015;9:386-93. [Google Scholar | PubMed]
- 9.Picci P, Manfrini M, Donati DM, Gambarotti M, Righi A, Vanel D, et al. Osteoid osteoma. In: Diagnosis of Musculoskeletal Tumors and Tumor-like Conditions. 2nd ed. Switzerland, Cham: Springer; 2020. p. 89-92. [Google Scholar | PubMed]
- 10.Mallepally AR, Mahajan R, Pacha S, Rustagi T, Marathe N, Chhabra HS. Spinal osteoid osteoma: Surgical resection and review of literature. Surg Neurol Int 2020;11:308. [Google Scholar | PubMed]
- 11.Kan P, Schmidt MH. Osteoid Osteoma and Osteoblastoma of the Spine. Neurosurg Clin N Am 2008;19:65-70. [Google Scholar | PubMed]
- 12.Zhang H, Niu X, Wang B, He S, Hao D. Scoliosis secondary to lumbar osteoid osteoma A case report of delayed diagnosis and literature review. Medicine (Baltimore) 2016;95:e5362. [Google Scholar | PubMed]
- 13.Watanabe K, Hosoya T, Shiraishi T, Matsumoto M, Chiba K, Toyama Y. Lumbar spinous process-splitting laminectomy for lumbar canal stenosis. Technical note. J Neurosurg Spine 2005;3:405-8. [Google Scholar | PubMed]
- 14.Shiraishi T. Skip laminectomy--a new treatment for cervical spondylotic myelopathy, preserving bilateral muscular attachments to the spinous processes: A preliminary report. Spine J 2002;2:108-15. [Google Scholar | PubMed]
- 15.Lee DY, Lee SH. Spinous process splitting laminectomy for lumbar canal stenosis: A critical appraisal. Minim Invasive Neurosurg 2008;51:204-7. [Google Scholar | PubMed]
- 16.Phan K, Mobbs RJ. Minimally invasive versus open laminectomy for lumbar stenosis: A systematic review and meta-analysis. Spine (Phila Pa 1976) 2016;41:E91-100. [Google Scholar | PubMed]
- 17.Smith ZA, Fessler RG. Paradigm changes in spine surgery: Evolution of minimally invasive techniques. Nat Rev Neurol 2012;8:443-50. [Google Scholar | PubMed]
- 18.Fiori R, Forcina M, Di Donna C, D’Onofrio A, Spiritigliozzi L, Cavallo AU, et al. Cryotherapy of acetabular osteoid osteoma under fluoroscopic guidance using the XperGuide System. Radiol Case Rep 2019;14:989-92. [Google Scholar | PubMed]
- 19.Nzokou A, Weil AG, Shedid D. Minimally invasive removal of thoracic and lumbar spinal tumors using a nonexpandable tubular retractor. J Neurosurg Spine 2013;19:708-15. [Google Scholar | PubMed]
- 20.Wang HL, Lü FZ, Jiang JY, Ma X, Xia XL, Wang LX. Minimally invasive lumbar interbody fusion via MAST Quadrant retractor versus open surgery: A prospective randomized clinical trial. Chin Med J (Engl) 2011;124:3868-74. [Google Scholar | PubMed]
- 21.Amendola L, Cappuccio M, Boriani L, Gasbarrini A. Endoscopic excision of C2 Osteoid Osteoma: A technical case report. Eur Spine J 2013;22:S357-62. [Google Scholar | PubMed]
- 22.Gasbarrini A, Cappuccio M, Bandiera S, Amendola L, van Urk P, Boriani S. Osteoid osteoma of the mobile spine: Surgical outcomes in 81 patients. Spine (Phila Pa 1976) 2011;36:2089-93. [Google Scholar | PubMed]
- 23.Kwak YS, Kim KT, Cho DC, Kim YB. Minimally invasive removal of an intradural cervical tumor: Assessment of a combined split-spinous laminectomy and quadrant tube retractor. J Korean Neurosurg Soc 2012;52:427-31. [Google Scholar | PubMed]
- 24.Tredway TL, Santiago P, Hrubes MR, Song JK, Christie SD, Fessler RG. Minimally invasive resection of intradural-extramedullary spinal neoplasms. Neurosurgery 2006;58:ONS52-8. [Google Scholar | PubMed]