How to manage periprosthetic femoral fractures with fracture of the femoral stem component with satisfactory results.
Dr. Abhilash P Sangtani, Department of Orthopaedics, Government Medical College and Hospital, Nagpur, Maharashtra, India. E-mail: abhilashsangtani92@gmail.com
Introduction: The incidence of periprosthetic fractures (PPF) around a total hip arthroplasty continues to increase with the rise in number of arthroplasties performed. However, fracture of the femoral stem has become very rare since the development of modern prosthetic designs. We present a rare case of an 80-year-old man who sustained a periprosthetic femur fracture with a fracture of the femoral stem component around a bipolar hemiarthroplasty.
Case Report: This man sustained a Vancouver type B1 periprosthetic femur fracture with a fracture of the femoral stem component around a fully cemented bipolar hemiarthroplasty done 10 years back. This patient was treated with removal of the broken femoral stem and osteosynthesis with a plate and cerclage wire plus revision to a longer stem prosthesis.
Conclusion: PPF with a fracture of the femoral stem around a hemiarthroplasty is a rare and uncommon occurrence. A combination of osteosynthesis with revision arthroplasty with a longer stem proved to be a suitable treatment with satisfactory results. However, regular follow-ups post-arthroplasties are advocated to identify complications at an earlier stage.
Keywords: Periprosthetic fracture, broken femoral stem, revision hemiarthroplasty.
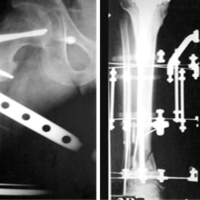
Since the first reported periprosthetic femur fracture around a hip arthroplasty in 1954 [1], the prevalence of periprosthetic fracture (PPF) continues to rise with the increasing rate of arthroplasties worldwide [2]. Operative management of PPF has been shown to result in the early mobilization and reduced hospital stay. It also affords a reduction in systemic and local complications such as malunion and non-union [3]. The Vancouver classification by Duncan and Masri is the most commonly used PPF classification and it facilitates treatment decision [4,5]. The majority of PPFs are located around the stem and classified as Vancouver type B (VTB) with either a well-fixed VTB1 or loose stem (VTB2) with poor bone stock (VTB3). The treatment choice for VTB1 is open reduction internal fixation, while the recommended management plan for a VTB2 is revision arthroplasty with a long stem bypassing the fracture site [6-8]. Although PPF is common, PPF with a fracture of the femoral stem is a very rare scenario. We present a rare case of an 80-year-old man who sustained a periprosthetic femur fracture with a fracture of the femoral stem component around a bipolar hemiarthroplasty. He had a cemented bipolar hemiarthroplasty done 10 years back for a fractured neck femur (Fig. 1).
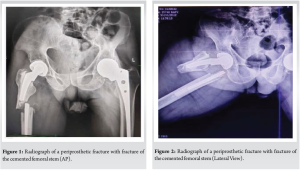
This was an 80-year-old man who had a primary cemented bipolar hemiarthroplasty done for a fractured neck femur. He was doing well until 10 years postoperatively when he had a domestic fall (Fig. 2). He sustained a periprosthetic VTB2 fracture with no obvious evidence of loosening at the cement bone interface with a fracture of the femoral stem. A proper history was obtained, and the patient did not have any previous thigh or groin pain to indicate any potential issues such as infection or loosening. Pre-injury radiographs were not available to confirm the same. The patient was not on any bisphosphonate therapy. Radiographs of the pelvis with both hips were done to assess the stem stability and bone quality. After thorough assessment and discussion, the patient was planned for removal of the broken prosthesis with osteosynthesis of the PPF with the help of a plate and cerclage wires and revision to a longer stem prosthesis. The patient was positioned in the lateral decubitus and the leg was prepped and draped for surgery. Through the previous surgical scar, the hip joint was opened through the posterior approach. The incision was extended down along the femur using a subvastus approach. The bipolar head was dislocated first. The implant was found relatively well-fixed. Osteotomes were used to chisel the bone cement in the proximal femur and to loosen the proximal part of the broken prosthesis after which the proximal femoral component was removed (Fig. 3 and 4).

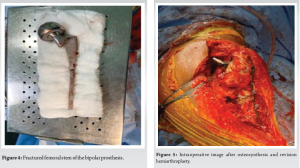
Subsequently, the distal fracture was exposed. Even here the distal broken femoral stem was found to be well-fixed. Osteotomes were used to break the cement implant interface and the broken implant was removed. The fracture site was exposed, debrided, and washed again with evidence of bleeding bone post-debridement. The fracture was then reduced and fixed with a l0 hole plate which was fixed proximally with three cerclage wires and distally with three locking screws. Once the PPF had been stabilized, revision hemiarthroplasty with a longer stem was performed. The reduction was found to be satisfactory. Subsequently, a couple of unicortical screws were inserted in the proximal fragment through the plate missing the bipolar prosthesis. The wound was thoroughly irrigated and hemostasis was achieved and closure was done in layers (Fig. 5 and 6).

Postoperatively, appropriate antibiotics and venous thromboembolism prophylaxis were administered as per routine departmental protocols. Immediate rehabilitation was with non-weight-bearing mobilization with walker support for 6 weeks. After clinical and radiological review at 6 weeks, the patient was progressed to full-weight-bearing. Clinical and radiological union were evident at the 6-month stage and with no post-operative complications (Fig. 7).

At the 1-year follow-up, this patient was independently mobile, back to walking 3000 steps a day, and performing all routine activities comfortably. He reported excellent patient-reported outcome at 1 year with an Oxford Hip Score of 40/48 and reported no issues with his bipolar hemi arthroplasty.
Femoral stem fractures associated with hip arthroplasty are a serious clinical problem [9]. Fortunately, fracture of a femoral prosthesis is not a frequent occurrence. The design of the prosthesis, type of surgery, body mass index, and activity level of the patient are important factors affecting the risk of stem fractures. In their case reporting femoral stem fracture after cemented total hip arthroplasty (THA), Jarvi and Kerry [10] addressed poor proximal support leading to cantilever-bending stresses on the middle part of the femoral stem as a main factor causing the fracture. In a report of ten cases, Woolson et al. [11] concluded that proximal debonding at the cement-prosthesis interface combined with a stem well-fixed distally was a cause of femoral stem fractures after cemented THA. If the patient is physically active, femoral stem fracture associated with poor proximal support becomes a matter of concern [12,13]. Garg et al. [13] highlighted that active patients carrying risk factors for implant failure after hip arthroplasty should be recommended to limit their activity. At present, internal fixation and revision THA are viewed as the gold standard, being utilized depending on implant stability, bone rigidity, and type of fracture. The careful evaluation of these factors is crucial within the process of deciding on the individually most efficient surgical procedure. Many cases simply show a non-adequate minor trauma, which might be resulting from prior implant loosening. Existing data document up to 70% of loose implants at the occurrence of periprosthetic femoral fractures, which is often a result of poor or missing follow-up visits. Elderly patients, frequently living in retirement homes, simply lack high-quality follow-up programs to screen for possible implant loosening before fracturing. In the present case, the pre-operative X-ray revealed that the cemented femoral stem was relatively well-fixed in the distal part when compared to the proximal part. Our patient underwent cemented hemiarthroplasty when he was 70 years old. He was a very healthy man leading a relatively active lifestyle even 10 years after the surgery.
PPF with a fracture of the femoral stem around a hemiarthroplasty is a rare and uncommon occurrence. A combination of osteosynthesis with revision arthroplasty with a longer stem proved to be a suitable treatment with satisfactory results. However, regular follow-ups post-arthroplasties are advocated to identify complications at an earlier stage.
Regular follow-ups post-arthroplasty with radiological assessment are essential to pick up complications at an early stage.
References
- 1.Horwitz IB, Lenobel MI. Artificial hip prosthesis in acute and nonunion fractures of the femoral neck: Follow-up study of seventy cases. J Am Med Assoc 1954;155:564-7. [Google Scholar]
- 2.Marsland D, Mears SC. A review of periprosthetic femoral fractures associated with total hip arthroplasty. Geriatr Orthop Surg Rehabil 2012;3:107-20. [Google Scholar]
- 3.Rayan F, Konan S, Haddad FS. Uncemented revision hip arthroplasty in B2 and B3 periprosthetic femoral fractures- a prospective analysis. HIP Int 2010;20:38-42. [Google Scholar]
- 4.Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect 1995;44:293-304. [Google Scholar]
- 5.Brady OH, Garbuz DS, Masri BA, Duncan CP. Classification of the hip. Orthop Clin North Am 1999;30:215-20. [Google Scholar]
- 6.Dargan D, Jenkinson MJ, Acton JD. A retrospective review of the Dall-Miles plate for periprosthetic femoral fractures: Twenty-seven cases and a review of the literature. Injury 2014;45:1958-63. [Google Scholar]
- 7.Lochab J, Carrothers A, Wong E, McLachlin S, Aldebeyan W, Jenkinson R, et al. Do transcortical screws in a locking plate construct improve the stiffness in the fixation of Vancouver B1 periprosthetic femur fractures? A biomechanical analysis of 2 different plating constructs. J Orthop Trauma 2017;31:15-20. [Google Scholar]
- 8.Lenz M, Stoffel K, Kielstein H, Mayo K, Hofmann GO, Gueorguiev B. Plate fixation in periprosthetic femur fractures Vancouver type B1-trochanteric hook plate or subtrochanterical bicortical locking? Injury 2016;47:2800-4. [Google Scholar]
- 9.Magnissalis EA, Zinelis S, Karachalios T, Hartofilakidis G. Failure analysis of two Ti-alloy total hip arthroplasty femoral stems fractured in vivo. J Biomed Mater Res B Appl Biomater 2003;66:299-305. [Google Scholar]
- 10.Jarvi K, Kerry RM. Segmental stem fracture of a cemented femoral prosthesis. J Arthroplasty 2007;22:612-6. [Google Scholar]
- 11.Woolson ST, Milbauer JP, Bobyn JD, Yue S, Maloney WJ. Fatigue fracture of a forged cobalt-chromium-molybdenum femoral component inserted with cement. A report of ten cases. J Bone Joint Surg Am 1997;79:1842-8. [Google Scholar]
- 12.Garg B, Mittal R, Rastogi S. Femoral prosthesis neck fracture following total hip arthroplasty: A case report. Acta Orthop Belg. 2011;77:406-9. [Google Scholar]
- 13.Huot Carlson JC, Van Citters DW, Currier JH, Bryant AM, Mayor MB, Collier JP. Femoral stem fracture and in vivo corrosion of retrieved modular femoral hips. J Arthroplasty 2012;27:1389-96. [Google Scholar]