Evaluating atypical multiple myeloma manifestations in the appendicular skeleton requires comprehensive assessment and diagnostic procedures to influence outcomes and improve quality of life. Managing suspected pathological fractures involves detailed evaluation and surgical planning, highlighting the importance of collaboration among different specialties.
Dr. Tanmay Avhad, Department of Orthopaedics, TNMC and BYL Nair Charitable Hospital, Mumbai, Maharashtra, India. E-mail: tanmayavhad@gmail.com
Introduction: The increasing incidence of atraumatic neck of femur (NOF) fractures, often linked to age-related bone weakening, is a notable clinical trend. This case report highlights a 72-year-old male presenting with NOF and proximal humerus fractures post-trivial fall, revealing lytic lesions suggestive of multiple myeloma (MM). Despite inconclusive skeletal and metabolic evaluations, a comprehensive surgical approach confirmed MM, emphasizing the importance of thorough diagnostic and therapeutic management in complex cases.
Case Report: A 72-year-old male presented with a trivial fall resulting in hip and shoulder trauma, revealing right transcervical NOF and proximal humerus fractures on X-rays, alongside multiple lytic lesions suggesting MM. Despite inconclusive metabolic evaluations, conservative management was pursued for the humerus fracture, while a complex surgical approach involving curettage and cemented bipolar hemiarthroplasty was undertaken for the femur fracture, confirming MM on histopathology.
Conclusion: Evaluating atypical MM manifestations in the appendicular skeleton requires comprehensive assessment and diagnostic procedures to influence outcomes and improve quality of life. Managing suspected pathological fractures involves detailed evaluation and surgical planning, highlighting the importance of collaboration among different specialties.
Keywords: Multiple myeloma, hematology, femur fracture, humerus fracture, pathological fracture.
The occurrence of neck of femur (NOF) fractures tends to rise as individuals age. In clinical settings, atraumatic NOF fractures are becoming more common and are typically characterized by fractures resulting from low-energy injuries. These fractures can be attributed to various factors such as stress, bone insufficiency, fatigue, as well as atypical and pathological conditions. Such factors can contribute to bone weakening or impair the healing process, ultimately diminishing bone integrity and strength [1]. Multiple myeloma (MM) is a cancerous condition characterized by the abnormal growth of plasma cells within the bone marrow [2,3]. The majority of patients diagnosed with MM exhibit skeletal abnormalities, which commonly include osteolytic lesions, osteopenia/osteoporosis, and fractures as manifestations of bone disease [4]. Despite advancements in diagnostic and treatment approaches [5], the life expectancy for individuals with MM remains relatively low. Therefore, it is crucial to prioritize the maintenance of a good quality of life for patients following diagnosis. This entails implementing prophylactic fixation for bones impacted by the disease and promptly addressing any pathological fractures that may occur [6,7]. In this case report, we describe the atypical case of a patient suffering from NOF fracture along with proximal humerus fracture as a primary manifestation of MM and its subsequent diagnosis.
A 72-year-old male came with a history of trivial fall at home leading to trauma to the right hip and right shoulder associated with pain and inability to move the limb. The patient was apparently alright before the fall and had a sedentary lifestyle, the patient was stabilized medically, and radiographs were obtained for the same (Fig. 1 and 2). X-ray of the pelvis with both hips was suggestive of right transcervical NOF # with left inferior pubic rami fracture. Right shoulder radiograph showed proximal humerus fracture. A striking finding on both the X-rays was multiple lytic punched-out lesions present over the pelvis, femur shaft, and humerus increasing the suspicion of MM or a metabolic affection. Skeletal screening was done for the patient of the spine skull, and remaining appendicular skeleton, but did not show any findings (Fig. 3). Metabolic survey was done to rule out MM such as B2 macroglobulin levels, Sr calcium, ALP, LDH, Bence–Jones proteinuria, renal function tests, and hemoglobin but was inconclusive.
Conservative management was chosen for the proximal humerus fracture, involving immobilization with a cuff and collar. However, the right transcervical NOF fracture necessitated a multifaceted approach due to the presence of lytic lesions in the shaft and proximal femur. A plan was made for a cemented bipolar hemiarthroplasty, involving the removal of intramedullary lesions through curettage followed by cementing helping the prosthesis, and chemical cauterization of the lesions. During surgery, islands of bony spicules were discovered, obstructing the medullary canal, requiring reaming with flexible femur reamers to ensure canal patency (Fig. 4).
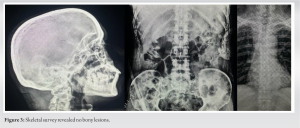
The lytic areas were curetted, and the tissue was sent for histopathology analysis. The surgery proceeded smoothly, and the patient recovered well. The histopathology report indicated the presence of round plasma cells with eccentric nuclei, prominent nucleoli, and chromatin arranged in a clock-face pattern. In addition, a characteristic clear area, known as the Hoffa clear zone, next to the nucleus suggested the involvement of the prominent Golgi apparatus in immunoglobulin production. These findings were indicative of MM, leading to the patient’s referral to medical oncology for further management. The patient had good restoration of mobility and showed good radiological union (Fig. 5).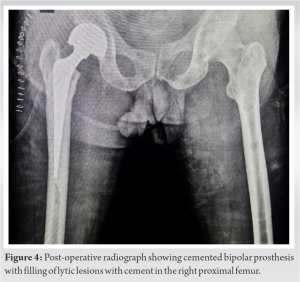
MM is a condition involving the unchecked growth of plasma cells and their accumulation in the bone marrow. This disease can lead to various symptoms such as anemia, susceptibility to infections, lytic bone lesions, and renal dysfunction. Interestingly, MM can also present asymptomatically, and its diagnosis might occur incidentally during medical evaluation [8]. To diagnose MM, health-care providers typically look for specific criteria, CRAB criteria, these include the presence of a monoclonal component in the serum or urine, a bone marrow with over 10% plasma cell infiltration, and at least one indicator of active disease.
These indicators may include elevated levels of serum calcium (>11 mg/dL), high creatinine levels (>2 mg/dL), hemoglobin levels lower than 2 g above normal values, a free light chain ratio exceeding 100, and the presence of one or more osteolytic lesions as detected by imaging techniques such as X-ray, computed tomography scan, or magnetic resonance imaging [3,9]. Many neoplastic disorders, including MM and other plasma cell dyscrasias, often necessitate frequent skeletal surveys and may require prophylactic bone fixation when deemed necessary. This proactive approach not only enhances the quality of life for individuals affected by these diseases but also serves to reduce associated morbidity. While numerous studies have documented pathological fractures linked to MM, a significant portion of these fractures tends to involve vertebrae [10,11]. Sheshagiri et al. documented a case involving MM with a pathological subtrochanteric femur fracture and a humerus shaft fracture. These fractures were effectively managed using single-stage intramedullary nailing, resulting in improved quality of life for the patient. This case underscores the significance of osteosynthesis and comprehensive management of pathological fractures in individuals with MM [12]. Fozzato et al. outlined the instance of a young individual encountering bilateral femur shaft fractures following a trivial fall. After thorough assessment, the patient received a diagnosis of MM was made and further management encompassed osteosynthesis interventions and coordination with hemat-oncology experts to halt disease advancement and proficiently address the malignancy [13]. Resection of tumor lesions and insertion of a prosthetic femoral head are recommended for managing pathological fractures of the femoral neck. In cases involving femoral trochanteric fractures and bone destruction, preventing pathological fractures is crucial through appropriate bed rest and timely surgery. Initially, pathological fractures of the lower limb long bones should be temporarily fixed with a plaster cast or traction, followed by prompt surgical fixation. Similar principles apply to upper extremity pathological fractures, although the upper limbs bear no weight. Internal fixation procedures are preferred over external fixation because they allow for tumor resection and restoration of bone continuity. It is important to note that chemotherapy and radiation are not effective treatments for pathological fractures in the long bones of limbs [14,15]. Determining the appropriate fixation system and surgical approach relies on several factors, including the patient’s overall health and life expectancy, previous response to chemotherapy, the location of the fracture (such as femoral neck, sub‐trochanteric, inter‐trochanteric), the number, size, and position of lesions, as well as the degree of bone invasion [16]. Our case presented an uncommon scenario, initially manifesting as a NOF fracture and a proximal humerus fracture due to low-energy trauma, serving as the sole indicators of underlying disease. Unlike typical MM patients, this individual did not exhibit common symptoms such as low back pain, weight loss, recurrent infections, or asthenia. Notably, their inflammatory indices, serum calcium levels, renal function, and blood hemoglobin were all within normal ranges despite the presence of multiple bone lesions. The diagnosis was further supported by significant bone loss observed at the fracture sites, which did not align well with the expected pattern of low-energy trauma, particularly considering the diffuse osteolytic lesions identified on skeletal survey. Subsequent laboratory investigations failed to reveal any monoclonal component in serum protein electrophoresis or kappa light chains in the urine. Management initially focused on addressing the femur fracture, with conservative management of the proximal humerus fracture to minimize potential complications. Histopathological evaluation of bone and soft-tissue sampled during the cemented hemi arthroplasty ultimately confirmed the diagnosis of MM.
Atypical presentation of MM involving the appendicular skeleton is rare and necessitate thorough evaluation, including comprehensive clinical assessments, metabolic profiling, imaging studies, and tissue diagnosis. This approach is crucial for influencing clinical outcomes, averting complications, and enhancing quality of life. Managing patients with suspected pathological fractures is intricate, demanding thorough diagnostic evaluation, meticulous pre-operative preparation, and establishment of a definitive surgical strategy, underscoring the need for collaboration among radiologists, hemato-oncologists, and orthopedic surgeons.
Evaluating atypical multiple myeloma manifestations in the appendicular skeleton requires comprehensive assessment and diagnostic procedures to influence outcomes and improve quality of life. Managing suspected pathological fractures involves detailed evaluation and surgical planning, highlighting the importance of collaboration among different specialties.
References
- 1.Hedge G, Thaker S, Botchu R, Fawcett R, Gupta H. Atraumatic fractures of the femur. Br J Radiol 2021;94:20201457. [Google Scholar | PubMed]
- 2.Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al. WHO classification of tumours of haematopoietic and lymphoid tissues. 4th ed., Vol. 2. Lyon, France: IARC; 2016. [Google Scholar | PubMed]
- 3.Rajkumar SV, Dimopoulos MA, Palumbo A, Blade J, Merlini G, Mateos MV, et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol 2014;15:e538-48. [Google Scholar | PubMed]
- 4.Kyle RA, Gertz MA, Witzig TE, Lust JA, Lacy MQ, Dispenzieri A, et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc 2003;78:21-33. [Google Scholar | PubMed]
- 5.Kehrer M, Koob S, Strauss A, Wirtz D, Schmolders J. Multiples Myelom - aktuelle standards in diagnostik und therapie. Z Orthop Unfall 2017;155:575-86. [Google Scholar | PubMed]
- 6.Small T, Fox K, Edge L, Harker J. Total hip arthroplasty with prophylactic fixation of greater trochanter and distal femur in a patient with a history of multiple myeloma and breast cancer. Cureus 2023;15:e37971. [Google Scholar | PubMed]
- 7.Panaroni C, Yee AJ, Raje NS. Myeloma and bone disease. Curr Osteoporos Rep 2017;15:483-98. [Google Scholar | PubMed]
- 8.Rajkumar SV, Kumar S. Multiple myeloma: Diagnosis and treatment. Mayo Clin Proc 2016;91:101-19. [Google Scholar | PubMed]
- 9.Signorini L, Dolci M, Favi E, Colico C, Ferraresso M, Ticozzi R, et al. Viral genomic characterization and replication pattern of human polyomaviruses in kidney transplant recipients. Viruses 2020;12:1280. [Google Scholar | PubMed]
- 10.Wernecke G, Namduri S, DiCarlo EF, Schneider R, Lane J. Case report of spontaneous, nonspinal fractures in a multiple myeloma patient on long-term pamidronate and zoledronic acid. HSS J 2008;4:123-7. [Google Scholar | PubMed]
- 11.Thorsteinsdottir S, Gislason G, Aspelund T, Sverrisdottir I, Landgren O, Turesson I, et al. Fractures and survival in multiple myeloma: Results from a population-based study. Haematologica 2020;105:1067-73. [Google Scholar | PubMed]
- 12.Sheshagiri V, Siddhartha A, Kumar S, Boopathy M, Vidya CS. Multiple myeloma with subtrochanteric femur fracture and shaft of humerus fracturetreated with single stage IMIL nailing: A case report. J Adv Zool 2023;44:153-6. [Google Scholar | PubMed]
- 13.Fozzato S, Bianco Prevot L, Amadei F, Gallina M, Ciccarelli A, Accetta R, et al. Bilateral femur fracture as the first manifestation of multiple myeloma: A case report. Clin Ter 2023;174:211-4. [Google Scholar | PubMed]
- 14.Papagelopoulos PJ, Galanis EC, Greipp PR, Sim FH. Prosthetic hip replacement for pathologic or impending pathologic fractures in myeloma. Clin Orthop Relat Res 1997;341:192-205. [Google Scholar | PubMed]
- 15.Issack PS, Barker J, Barker M, Kotwal SY, Lane JM. Surgical management of metastatic disease of the proximal part of the femur. J Bone Joint Surg Am 2014;96:2091-8. [Google Scholar | PubMed]
- 16.Kivioja AH, Karaharju EO, Elomaa I, Böhling TO. Surgical treatment of myeloma of bone. Eur J Cancer 1992;28A:1865-9. [Google Scholar | PubMed]







