En bloc excision and fibular grafting with plate fixation are preferred treatment options for giant cell tumors of metatarsal bones.
Dr. Nitish Kumar, Department of Orthopedics, All India Institute of Medical Sciences, Gorakhpur, Uttar Pradesh, India. E-mail: nitishaiims@gmail.com
Introduction: Giant cell tumor (GCT) is a benign locally aggressive tumor with features of frequent recurrence and metastatic potential. GCT of small bones of hand and feet is rare with high recurrence and potential to metastasis. This study aims to provide a case report of GCT of the first metatarsal treated with wide excision, autologous fibular grafting, and fixation with locking plate.
Case Report: An 18-year-old male patient presented with progressive swelling over the dorsomedial aspect of foot for 1 year. Upon clinical examination, the swelling was firm with local signs suggestive of a benign bony tumor arising from the base of first metatarsal of the left foot. Radiology reveals an expansile osteolytic lesion arising from the base of 1st metatarsal with coarse septations and features suggestive of a benign bone lesion. A core biopsy was obtained under local anesthesia and histopathology report suggested a GCT. Surgical intervention by en bloc excision and reconstruction by fibular autograft and stabilized with a locking plate was done. The patient was given a below-knee cast for 6 weeks postoperatively. Full weight bearing was started after 6 weeks. At 12 months of follow-up, the graft was well taken up and there were no signs of recurrence both clinically and radiologically.
Conclusion: GCT of 1st metatarsal is a rare entity with higher recurrence rate compared to conventional GCT. En bloc excision and autologous fibular graft with plate fixation are preferred treatment options.
Keywords: Giant cell tumor, first metatarsal, rare entity.
Giant cell tumor (GCT) is a common benign aggressive lytic lesion that accounts for 4–5% of primary bone tumors and almost 20% of benign bone tumors [1]. GCT has very high chances of local recurrence with occasional metastatic potential. It usually occurs in young adults of 16–35 years age. Mostly occurs in physeal region of long bones. Male-to-female ratio is 3:5 meaning that this tumor has slight female preponderance. Nearly, 85–90% of GCT are found in long bones, of which 50% occur around the knee, i.e., proximal tibia and distal femur. Other frequent sites are distal radius, proximal humerus, and fibula. 4% occur in the pelvic bone and spine. Involvement of small bones of the hand and foot is very rare with high recurrence and metastatic potential. We are presenting a case of GCT of 1st metatarsal of the left foot which is a rare site for this tumor. It was treated with en bloc excision and reconstruction by fibular autograft and stabilized with a locking plate.
An 18-year-old male patient presented with mild-to-moderate pain localized to the left foot and progressive swelling over the dorsomedial aspect of the foot for 1 year. Upon local examination, the swelling was arising from the first metatarsal bone of the left foot. The local temperature was normal and comparable with the contralateral foot. It was tender to touch and firm in consistency. The distal margin was palpable and delineated but the proximal margin of swelling was diffuse and not well appreciable. The overlying skin was free from underlying swelling with no surficial dilated veins. The local signs were suggestive of a benign bony tumor arising from the base of first metatarsal of the left foot. There was no history of trauma or similar swelling in other parts of the body.
Investigation
Plain X-ray anterioposterior and lateral view of the affected foot showed an expansile lytic lesion arising from the base of the first metatarsal with coarse internal septation. There was no cortical breach noted on the visualized part of the bone on X-ray film (Fig. 1).
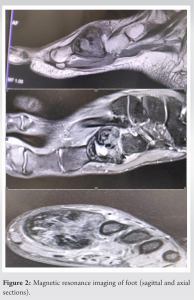
The plain magnetic resonance imaging of the foot showed a well-circumscribed, expansile lytic lesion with internal septation without any soft-tissue expansion arising from the left first metatarsal base suggestive of GCT (Fig. 2).
After radiological investigations, the core biopsy was obtained under local anesthesia. The patient lye supine with the knee flexed and the foot resting flat on the operation table. Foot cleaning and sterile draping were done as per standard protocol. 5 mL plain 2% lignocaine was infiltrated over the dorsal aspect of swelling till the level of periosteum. 11G Jamshidi biopsy needle was used to harvest biopsy from the distal margin of the swelling under fluoroscopy guidance. The histopathological report of the biopsy was consistent with the finding of GCT (Fig. 3).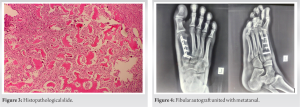
Surgical treatment
After clinic-radiological and histopathological confirmation, tumor excision was planned under spinal anesthesia. After tourniquet inflation, a midline incision was given over the dorsal aspect of the first metatarsal bone incorporating the previous biopsy scar. The extensor hallucis longus tendon was retracted and tumor was approached. Care was taken to avoid any injury to the dorsalis pedis artery at the lateral corner of the base of the first metatarsal bone. The tumor was excised leaving around 2 cm of the distal part of the metatarsal bone intact with metatarsophalangeal joint and sent for histopathological examination. The tissue from the margin of the leftover metatarsal bone was sent for a frozen section biopsy to confirm tumor free margin. The gap created after the excision of tumor tissue was reconstructed using an ipsilateral autologous fibular graft. The cartilage from the tarsometatarsal side of the medial cuneiform bone was shaved off to accept the fibular graft. The fibular graft was placed in the defect created after tumor excision and was fixed with 2.7 mm Locking compression plate [LCP] , the wound was closed in layers and the limb was placed in below-knee plaster slab till suture removal at 15 days. The partial weight bearing was started after suture removal at 2 weeks and the patient was put on below-knee cast for another 4 weeks. At 6 weeks, the cast was removed, ankle physiotherapy was started, and the patient was started on full weight bearing. Regular follow-up by clinical examination and X-ray was done. By 6 months, the patient was walking normally with full support on the operated limb with X-ray sowing complete uptake of the graft. The patient was further followed up for 1-year post-surgery and there were no signs of recurrence both clinically and radiologically (Fig. 4).
GCT of small bone of hand and feet is rare phenomenon but it carries a higher risk of local recurrence as compared to conventional GCT. The tendency of developing in younger individuals has been reported in various studies [2,3]. The main subjective symptoms are pain at the local site similar to conventional GCT, and radiologically cortical expansion is more in small bone GCT compared to conventional GCT, reason might be . It has also been reported in the literature that GCT of the hand adopts a more aggressive clinical course than that of GCTs occurring in more central locations [4]. In contrast, Malawer and Vance reported that GCT in the tarsal bones was not as aggressive and carried a good prognosis [5]. Surgical treatment options are curettage, curettage with adjuvants, and wide excision. The rate of recurrence of small bone GCT was at the higher end of range reported in the literature for long bone GCT which is 27–65% after curettage only, 12–34% after curettage with adjuvant, and up to 12% after resection [6-9]. Complete removal of GCT of small bones is technically difficult by both intralesional and wide excision. En bloc resection and ray amputation have been advocated in technically challenging cases, as they are believed to minimize the risk of recurrence [10,11]. In our case, a gap created after excision of tumor tissue was reconstructed using an ipsilateral autologous fibular graft and was fixed with 2.7 mm LCP. A few authors also advocate the use of k-wire for the fixation of fibular grafts [12]. After suture removal on day 15th, below-knee cast was applied for a further 4 weeks and the patient was allowed to walk with toe touching the ground putting partial weight on the affected limb. It is in contrast to authors who were using k-wire to fix the graft had to delay weight bearing for up to 3 months. In our case 6 weeks after surgery, plaster was removed, physiotherapy was started, and the patient was started with full weight bearing. We suggest that using low-profile LCP for fixation of autologous fibular graft has advantage of achieving compression at the host and graft site and early weight bearing promoting early graft incorporation. Complete functional recovery was noted at 6 months with a sign of the union of auto graft with host bone.
GCT of small bones of hand and feet is rare entity with a very high rate of recurrence after intralesional curettage and bone grafting. The treatment option varies from curettage to segmental resection to ray amputation depending upon the extent of disease progression and level of involvement.
The long bones of hand and foot are more commonly affected by tumors like enchondroma and incidence of GCT at these sites is very rare. The clinician treating any bony swelling of the foot should be aware of the rare occurrence of this condition and should obtain a biopsy to establish the diagnosis. They should judicially choose from various treatment options available to treat GCT of metatarsal to suit the clinical condition of the case treated by them.
References
- 1.Campanacci M, Baldini N, Boriani S, Sudanese A. Giant-cell tumor of bone. J Bone Joint Surg 1987;69:106-114. [Google Scholar | PubMed]
- 2.BiscagliaR, BacchiniP, Bertoni F. Giant cell tumor of the bones of the hand and foot. Cancer 2000;88:2022-32. [Google Scholar | PubMed]
- 3.Cavender RK, Sale WG 3rd. Giant cell tumor of the small bones of the hands and feet: Metatarsal giant cell tumor. W V Med J 1992;8:342-5. [Google Scholar | PubMed]
- 4.Okada K, Takahashi S, Nagasawa H, Suzuki N, Chiba S, Nishida J. Giant cell tumor in the cuboid. Upsala J Med Sci 2007;112:245-50. [Google Scholar | PubMed]
- 5.Malawer MM, Vance R. Giant cell tumor and aneurysmal bone cyst of the talus: Clinicopathological review and two case reports. Foot Ankle 1981;1:235-44. [Google Scholar | PubMed]
- 6.Balke M, Schremper L, Gebert C, Ahrens H, Streitbuerger A, Koehler G, et al. Giant cell tumor of bone: Treatment and outcome of 214 cases. J Cancer Res Clin Oncol 2008;134:969-78. [Google Scholar | PubMed]
- 7.Arbeitsgemeinschaft Knochentumoren, Becker WT, Dohle J, Bernd L, Braun A, Cserhati M, et al. Local recurrence of giant cell tumor of bone after intralesional treatment with and without adjuvant therapy. J Bone Joint Surg 2008;90:1060-7. [Google Scholar | PubMed]
- 8.Kivioja AH, Blomqvist C, Hietaniemi K, Trovik C, Walloe A, Bauer HC, et al. Cement is recommended in intralesional surgery of giant cell tumors: A scandinavian sarcoma group study of 294 patients followed for a median time of 5 years. Acta Orthop 2008;79:86-93. [Google Scholar | PubMed]
- 9.Errani C, Ruggieri P, Asenzio MA, Toscano A, Colangeli S, Rimondi E, et al. Giant cell tumor of the extremity: A review of 349 cases from a single institution. Cancer Treat Rev 2010;36:1-7. [Google Scholar | PubMed]
- 10.Picci P, Baldini N, Sudanese A, Boriani S, Campanacci M. Giant cell reparative granuloma and other giant cell lesions of the bones of the hands and feet. Skeletal Radiol 1986;15:415-21. [Google Scholar | PubMed]
- 11.Kamath S, Jane M, Reid R. Giant cell tumour around the foot and ankle. J Foot Ankle Surg 2006;12:99-102. [Google Scholar | PubMed]
- 12.Prashant K, Bhattacharyya TD, Frank H, Ram P. An unusual case of Giant cell tumor of first meatarsal: A rare case report and review of literature. J Orthop Case Rep 2016;6:3-6. [Google Scholar | PubMed]










