Our case underscores the critical need for vigilant monitoring and immediate intervention in sever transfusion reactions post-total knee arthroplasty, emphasizing the multifocal nature of such complications and the importance of comprehensive patient care strategies.
Dr. Niranjan Sunil Ghag, Department of Orthopedics, Grant Government Medical College and Sir JJ Group of Hospitals, Mumbai, Maharashtra, India. E-mail: niranjanghag95@gmail.com
Introduction: Blood transfusions are essential for managing blood loss in surgical patients but can lead to life-threatening reactions. This report presents a severe transfusion reaction in a post-operative total knee arthroplasty (TKA) patient, emphasizing the need for vigilant monitoring and timely intervention.
Case Report: A 70-year-old male with a history of bilateral knee pain underwent right-sided TKA. Pre-operative evaluations were normal. Post-surgery, significant blood loss led to a one-pint-packed red blood cell transfusion. The patient developed fever, chills, palpitations, and rapid breathing, indicating a transfusion reaction. Despite immediate treatment, the patient’s condition deteriorated, requiring intensive care unit admission. Complications included acute kidney injury, metabolic acidosis, thrombocytopenia, pleural effusion, and aspiration pneumonitis. Multiple organ dysfunction syndrome developed, necessitating hemodialysis. Despite comprehensive care, the patient passed away.
Conclusion: This case highlights the critical need for rigorous pre-transfusion screening, vigilant monitoring, and immediate intervention in managing severe transfusion reactions in post-operative TKA patients. Comprehensive patient care strategies are essential to mitigate the multifocal complications associated with transfusion reactions. Additional research is needed to understand and prevent such life-threatening reactions.
Keywords: Total knee arthroplasty, transfusion reaction, acute kidney injury, multiple organ dysfunction syndrome, patient monitoring.
Blood transfusion is an essential therapeutic measure for managing intraoperative and post-operative blood loss in surgical patients [1]. Although transfusion reactions are infrequent, they can be life-threatening [2]. While many reactions are mild and delayed, we present a first and unique case in which a post-operative knee arthroplasty patient experienced a severe transfusion reaction, leading to acute kidney injury (AKI) and multiple organ dysfunction syndrome (MODS). The report offers valuable insights into the intricacies of transfusion-related complications and their multifaceted impact on post-operative patients. This report seeks to find out the potential consequences of severe transfusion reactions, emphasizing the importance of screening for risk factors and preventive measures in total knee arthroplasty (TKA) patients, vigilant monitoring, and timely intervention in transfusion therapy.
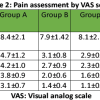
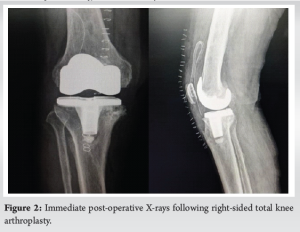
A 70-year-old male with 6-year bilateral knee pain presented primarily affecting the right knee (Fig. 1). Following a thorough evaluation, including tests for infection markers (erythrocyte sedimentation rate, C-reactive protein, and white blood cell count [WBC] count all within normal limits) and a pre-operative hemoglobin level of 13.2 mg/dL, the decision was made to proceed with right-sided TKA (Fig. 2). The surgery resulted in an estimated blood loss of 350 mL and a surgical drain. The patient’s recovery was unremarkable. The drain output during the first 3 days was 700 mL, 200 mL, and 100 mL, respectively, and the post-operative hemoglobin level decreased to 9.8 mg/dL after 3 days. To address the significant blood loss, a one-pint-packed red blood cell transfusion was initiated after blood grouping (B positive) and cross-matching. However, the patient developed fever, chills, palpitations, and rapid breathing symptoms. The transfusion was halted, and the patient received intravenous injections of pheniramine maleate and hydrocortisone. The patient’s condition did not improve, leading to their prompt transfer to the emergency department. Subsequent evaluation confirmed a blood transfusion reaction.

In the emergency department, a comprehensive workup was conducted, including repeat blood tests, chest X-ray (Fig. 3a), electrocardiogram (ECG), and a 2D echocardiography. The ECG indicated sinus tachycardia with a heart rate of 144 bpm, while the 2D echo revealed normal findings. The patient’s blood pressure was elevated at 180/100 mm Hg, but the chest radiograph showed no abnormalities (Fig. 3b) and the chest was clear on auscultation without any adventitious breath sounds.
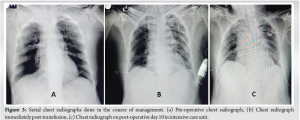
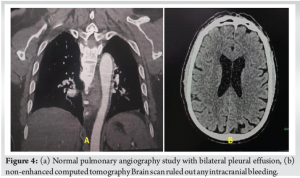
The patient’s blood pressure and heart rate were stabilized, and he was subsequently transferred to the intensive care unit (ICU) for further monitoring. However, the patient’s creatinine levels began to rise, reaching 2.8 mg/dL initially and eventually reaching 5–6 mg/dL, accompanied by metabolic acidosis, thrombocytopenia, and an increased WBC. His neurological status deteriorated, and he exhibited altered mental status and decreased oxygen saturation. A chest X-ray showed pleural effusion in the left lung (Fig. 3c) and elevated D-dimer levels, prompting a computed tomography (CT) pulmonary angiography (normal pulmonary angiography findings with bilateral pleural effusion) (Fig. 4a). The CT scan of the brain showed age-related degenerative changes without significant findings (Fig. 4b). Central line placement was performed for fluid management, and hemodialysis was recommended. Although the creatinine levels improved slightly, the patient’s overall condition did not significantly improve.
A patient was diagnosed with post-contrast AKI due to a blood transfusion reaction, hyperuricemia encephalopathy, and potential sepsis. He was transferred to the nephrology department for further care and management in the ICU. He underwent renal function testing, urine output monitoring, and hydration. He received multiple sessions of hemodialysis over a week, and although creatinine levels remained within 6–8 mg/dL for several days, urine output improved, and he regained orientation. He was transferred back to the general ward with stabilized vital signs and suture removal proceeded without complications on post-operative day 14. However, before full recovery, the patient experienced aspiration pneumonitis and passed away within a day.
Modern TKA offers great clinical outcomes, but surgeons are constantly seeking ways to improve efficiency, patient safety, and health-care costs. Factors that predict perioperative blood transfusion include American Society of Anesthesiologists (ASA) class, age, pre-operative and post-operative hemoglobin, change in hemoglobin, and adherence to transfusion triggers [3,4]. Blood transfusion reactions, although rare, can result in life-threatening complications due to an immune response triggered by the recipient’s exposure to red blood cell antigens during transfusion [1]. Most transfusion reactions are mild or delayed in onset, often occurring long after the causative transfusion [2]. Owens et al. found that 3.0% of 48,055 TKA patients required transfusion, with higher body mass index, older patients, greater comorbidities, and ASA class 3–4 [5]. Patients who were transfused showed a notably elevated incidence of sequelae, including septic shock, pneumonia, deep vein thrombosis, urinary tract infection, renal failure, cardiac arrest, myocardial infarction, reoperation, and unplanned readmission mortality [5]. Post-operative TKA patients may be more susceptible to severe transfusion reactions due to several factors: Systemic inflammation [6], surgical trauma [7], pre-operative health status [8], and age [9]. Systemic inflammation [6] can amplify the immune response to transfused blood products, while surgical trauma [7] can release proinflammatory substances into the bloodstream, increasing the risk of adverse reactions. The case of AKI highlights the importance of vigilant monitoring of renal function post-transfusion [10]. Severe transfusion reactions can lead to MODS, a serious consequence of these reactions. The relationship between transfusion reactions and MODS is still under investigation, and further research is needed to understand the contributing factors [11]. Sepsis, a complication of transfusion reactions, can lead to sepsis-related kidney injury, and timely recognition and intervention are crucial [12]. The patient’s aspiration pneumonitis further complicates the clinical course, emphasizing the need for stringent post-operative care. Prevention measures include rigorous pre-transfusion screening [13], close monitoring during transfusions [14], adhering to blood transfusion safety guidelines (e.g., leukoreduction filters, etc.) [15], and developing a risk assessment model for transfusion reactions [16]. A straightforward risk assessment model [16] can be created to determine which patients require post-operative hemoglobin monitoring and transfusion risk assessment, which should be prepared perioperatively through multidisciplinary approaches and blood management strategies to decrease intraoperative blood loss.
This case report highlights the multifactorial nature of severe transfusion reactions in post-operative TKA patients and the importance of vigilant monitoring, immediate recognition, and timely intervention. The results of this case are crucial when dealing with TKA patients who have identified risk factors for transfusion. These patients should undergo pre-operative preparation using blood management measures and interdisciplinary approaches to minimize blood loss during surgery. Additional research is needed to comprehend the mechanisms behind these reactions and to create more efficient preventative and management tactics.
This case underscores the critical importance of vigilant monitoring and immediate intervention in severe transfusion reactions post-TKA. It emphasizes the multifocal nature of such complications and the necessity of a comprehensive patient care strategy, including rigorous pre-transfusion screening and adherence to blood transfusion safety guidelines. Health-care providers must be prepared to address severe transfusion reactions effectively, recognizing the unpredictable and potentially life-threatening nature of these events.
References
- 1.Kleinman S, Caulfield T, Chan P, Davenport R, McFarland J, McPhedran S, et al. Toward an understanding of transfusion-related acute lung injury: Statement of a consensus panel. Transfusion 2004;44:1774-89. [Google Scholar | PubMed]
- 2.Rohde JM, Dimcheff DE, Blumberg N, Saint S, Langa KM, Kuhn L, et al. Health care-associated infection after red blood cell transfusion: A systematic review and meta-analysis. JAMA 2014;311:1317-26. [Google Scholar | PubMed]
- 3.Aderinto J, Brenkel IJ. Pre-operative predictors of the requirement for blood transfusion following total hip replacement. J Bone Joint Surg Br 2004;86:970-3. [Google Scholar | PubMed]
- 4.Parvizi J, Huang R, Rezapoor M, Bagheri B, Maltenfort MG. Individualized risk model for venous thromboembolism after total joint arthroplasty. J Arthroplasty 2016;31:180-6. [Google Scholar | PubMed]
- 5.Owens J, Otero JE, Noiseux NO, Springer BD, Martin JR. Risk factors for post-operative blood transfusion following total knee arthroplasty. Iowa Orthop J 2020;40:69-73. [Google Scholar | PubMed]
- 6.Hofmann E, Faller N, Limacher A, Méan M, Tritschler T, Rodondi N, et al. Educational level, anticoagulation quality, and clinical outcomes in elderly patients with acute venous thromboembolism: A prospective cohort study. PLoS One 2016;11:e0162108. [Google Scholar | PubMed]
- 7.Kulshrestha V, Sood M, Kumar S, Sood N, Kumar P, Padhi PP. Does risk mitigation reduce 90-day complications in patients undergoing total knee arthroplasty?: A cohort study. Clin Orthop Surg 2022;14:56-68. [Google Scholar | PubMed]
- 8.Cappellini MD, Fiorelli G. Glucose-6-phosphate dehydrogenase deficiency. Lancet 2008;371:64-74. [Google Scholar | PubMed]
- 9.Cheung BM, Li C. Diabetes and hypertension: Is there a common metabolic pathway? Curr Atheroscler Rep 2012;14:160-6. [Google Scholar | PubMed]
- 10.Kellum JA, Lameire N, KDIGO AKI Guideline Work Group. Diagnosis, evaluation, and management of acute kidney injury: A KDIGO summary (Part 1). Crit Care 2013;17:204. [Google Scholar | PubMed]
- 11.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The Third International consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 2016;315:801-10. [Google Scholar | PubMed]
- 12.Zuercher P, Moret CS, Dziewas R, Schefold JC. Dysphagia in the intensive care unit: Epidemiology, mechanisms, and clinical management. Crit Care 2019;23:103. [Google Scholar | PubMed]
- 13.Carson JL, Grossman BJ, Kleinman S, Tinmouth AT, Marques MB, Fung MK, et al. Red blood cell transfusion: A clinical practice guideline from the AABB*. Ann Intern Med 2012;157:49-58. [Google Scholar | PubMed]
- 14.Linden JV, Wagner K, Voytovich AE, Sheehan J. Transfusion errors in New York State: An analysis of 10 years’ experience. Transfusion 2000;40:1207-13. [Google Scholar | PubMed]
- 15.Popovsky MA, Moore SB. Diagnostic and pathogenetic considerations in transfusion-related acute lung injury. Transfusion 1985;25:573-7. [Google Scholar | PubMed]
- 16.Acuña AJ, Grits D, Samuel LT, Emara AK, Kamath AF. Perioperative blood transfusions are associated with a higher incidence of thromboembolic events after TKA: An analysis of 333,463 TKAs. Clin Orthop Relat Res 2021;479:589-600. [Google Scholar | PubMed]