Remarkable correction can be achieved in severe rigid scoliosis by Extended posterior release, facetectomy, and posterior spinal fusion without life-threatening complications of anterior release
Dr. Kaman Kuity, Department of Orthopaedic Surgery, Dr. D.Y. Patil Medical College, Hospital and Research Centre, Pimpri, Pune - 411 018, Maharashtra, India. E-mail: kamaniimsar11@gmail.com
Introduction: Sever rigid scoliotic deformity (magnitude of the curve >80° and <25% correction on bending film) correction is a great challenge to spine surgeons. Severe scoliosis when untreated or not treated properly, may lead to severe complications due to curve progression. The aim of operative management is to achieve significant correction of sagittal, coronal, and rotational deformity to avoid neurodeficit, maintain sagittal balance, and improve cardiopulmonary function.
Materials and Methods: In this retrospective study, eight patients with severe rigid scoliosis who underwent through single-staged extended posterior release and spinal fusion between March 2022 and November 2023. The surgical procedures were the excision of the posterior ligament and spinous process, laminectomy, excision of ligament flavum, facetectomy, and posterior spinal fusion utilizing pedicle screws, rods, and sub-laminar wires. Patients were evaluated radiologically using posteroanterior and lateral X-rays of the whole spine and computed tomography scans. Demographic data, pre- and post-operative cobbs angle, osteotomized segment, instrumentation segments, blood loss, operation duration, follow-up duration, and complications were recorded.
Results: Pre-operative mean cobbs angle was 94.1° (range 83–110°) and post-operative mean cobbs angle was 33.3° (range 28–42°) with 64.6% scoliosis correction. The mean estimated blood loss was 517 mL (range 300–580 mL). The mean operation duration was 272.5 min (210–340 min). Mean spinal fixation fusion segments were 11.1 (range 8–14). No major complications were noted.
Conclusion: Our study concluded that extended posterior-only release, facetectomy, and posterior spinal fusion by utilizing pedicle screws and pre-contoured rods significantly corrected severe and rigid scoliosis with a high correction rate and avoid complications of anterior release. Hence, we can achieve remarkable correction in rigid scoliosis using the proper choice of levels, proper implant, and extended posterior release.
Keywords: Severe rigid scoliosis, extended posterior release, posterior spinal fusion.
Scoliosis is a three-dimensional deformity of the spine that occurs in the sagittal, frontal, and coronal plane with rotational deformity of the vertebral body. Adolescent idiopathic scoliosis (AIS) is the most common type among all idiopathic scoliosis (55–85%). It is a great challenge for spine surgeons to correct deformity in rigid and severe scoliosis (magnitude of the curve >80° and <25% correction on bending film) [1]. Severe rigid scoliosis when untreated or not treated properly, may lead to severe complications due to curve progression. The aim of operative management is to achieve significant correction of sagittal, coronal, and rotational deformity to avoid neurodeficit, and cosmetic hazards, maintain sagittal balance, improve cardiopulmonary function, and prevent curve progression. Several previous studies have reported good functional outcomes achieved in severe and rigid AIS by the combination of anterior release and posterior spinal fusion [2,3]. Corpectomies and discectomies are done anteriorly, and facectomies, laminectomies, and ligament release are done posteriorly. However, some life-threatening complications such as cardiopulmonary dysfunction and injury to the adjacent organs are reported in anterior release [4]. Recent reports have shown that posterior-only approaches utilizing pedicle screws are comparatively safer than combined approaches with significant correction of deformity [5]. Extended posterior release and spinal fusion utilizing pedicle screws, rods, and sub-laminar wire is one of the most effective techniques to correct severe rigid scoliosis with minimal complications. Pedicle screw fixation into the vertebral body through the posterior approach become popular due to it facilitates three-dimensional curve correction. The goal of the study was to assess the functional and radiological outcomes of the extended posterior release and instrumentation in AIS.
Study design
Retrospective study in a single teaching institution.
Study size
Eight cases of scoliosis.
Study period
The duration of the study period was March 2022–November 2023.
Patients were part of the study as per the inclusion and exclusion criteria.
Inclusion criteria
The following criteria were included in the study:
-
- AIS and congenital rigid scoliosis who underwent thorough single-staged extended posterior release procedure, facetectomy, and instrumentation
- Sever rigid scoliosis (magnitude of the curve >80° and <25% correction on bending film)
- Primary cases (no previous surgery and no pre-operative treatment).
Exclusion criteria
The following criteria were excluded from the study:
- Patients with flexion deformity
- Patients underwent through vertebral column resection
- Adult idiopathic scoliosis.
Age and sex distribution
Eight scoliosis patients who underwent extended posterior release were between 10 and 18 years old. Among eight patients five were female and three were male.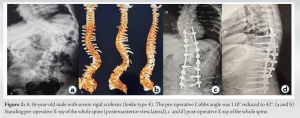
Pre-operative assessment
Preoperatively, all patients were evaluated clinically and radiologically. Bilateral upper and lower limb power was Medical Research Council grade 5 and sensation was intact in all patients. Computed tomography (CT) scan and magnetic resonance imaging are done to determine the exact site of deformity, neurological involvement, and associated other anomalies. Pre-operative Cobbs angle and Lenke classification were done by X-rays and CT scan. Thorough cardiological and respiratory evaluation was done to rule out any cardio-respiratory impairment. All routine laboratory investigations are performed for pre-operative assessment and pre-anesthetic check-ups.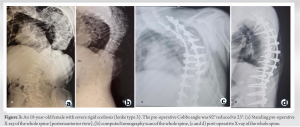
Surgical technique
Patients were placed in the prone position with the arm abducted at 90° and the elbow in 90° flexion. Hips in extension to maintain lumber lordosis and knees were slightly flexed. All pressure points are well-padded.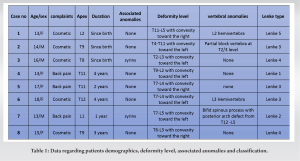
After proper antiseptic scrubbing and painting a straight midline incision from one vertebra above to proposed fusion area to one vertebra below it. Expose spinous process and facet joints subperiosteally with the help of Cobbs retractor and electrocautery. Caudal to cephalad dissection is easier due to the oblique attachment of muscle.
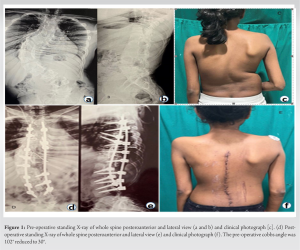
The inferior articular facet of the superior vertebra was removed using osteotome and superior articular facet cartilage of inferior vertebra curettage to provide fusion which was augmented by local bone graft hervas from spinous process and facet joint. Laminectomy and excision of ligamentum flavum was done. Bilateral pedicle screws were inserted by free hand technique and screw trajectories were checked and confirmed by fluoroscopy in both views (anteroposterior [AP] and lateral). Pedicle screws were fixed by bilateral pre-contured rods and correction was achieved by compression, translation, and distraction which were confirmed in coronal and sagittal view using fluoroscopy. We used sub-laminar wires in severe deformities to augment pedicle screw fixation and to correct the deformities. Injection cefuroxime was administered 30–60 min before skin incision for pre-operative antibiotics prophylaxis and continued for 3 days. Tranexamic acid was given intra-operatively to reduce blood loss and mean arterial pressure was maintained between 70 and 90 mmHg to achieve a bloodless field. Patients were mobilized within 1 week of the surgery and started and gradually started daily living activity (Fig. 1).
There were 3 male (37.5%) and 5 female (62.5%) patients. The mean age at the surgery was 14.8 years (range 13–18 years). According to the age three patients were classified as congenital idiopathic scoliosis (37.5%) and five patients were AIS (62.5%). Out of the eight patients, three patients presented with back pain, and five patients presented with cosmetic problems. Vertebral anomalies were seen in 4 (50%) cases (hemivertebra-2; bifid spinous process-1, partial block vertebra-1) and syrinx was shown in 2 (25%) cases.
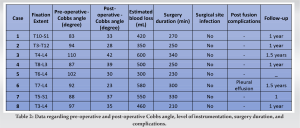
Preoperatively, all patients were classified based on lenke classification (Table 1).
- Lenke 1 – 1 (12.5%)
- Lenke 2 – 1 (25%)
- Lenke 3 – 3 (37.5%)
- Lenke 4 – 2 (25%)
- Lenke 5 – 1 (12.5%).
Facetectomy was performed in all cases and each level was fixed with bilateral pedical screws and pre-contoured rods. Rod and screw material used were titanium. Rod diameter was 5.5 in all cases. Mean level of spinal fixation was 11.1 (range 8–14). As shown in Table 2, pre-operative mean Cobbs angle was 94.1 (range 83–110°) and the post-operative mean Cobbs angle was 33.3 (range 28–42°) with 64.6% scoliosis correction (Fig. 2 and 3). The mean estimated blood loss was 517 mL (range 300–580 mL). The mean operation duration was 272.5 min (210–340 min). Minor post-fusion complications (pleural effusion) were noted in only one patient.
Complications
Intraoperative complications such as a significant episode of hypotension were seen in one patient, and no significant intraoperative neuromonitoring signal changes were seen in patients during facetectomy and instrumentation. No significant post-operative neurological complications in any patient. One patient developed post-operative pleural effusion and needed high-flow oxygen (8–10 L), none of them developed superior mesenteric artery syndrome. There were no surgical site infections. We noted no cases of pseudoarthrosis and instrumentation-related complications.
Scoliosis is a disease of a thoracolumbar spine in which the vertical axis of the spine deviates laterally. The exact etiological factor of AIS is unknown but several factors are proposed such as genetic, neurological disorder, hormonal dysfunction, environmental, and lifestyle factors. Sever rigid scoliosis is defined as curve flexibility <30° and Cobbs angle >80° by many studies [1], >90° by few studies [6,7], and even >100° [2] by another few studies. We are taking Cobbs angle >80° and curve flexibility <30° as an acceptable criterion. Combined anterior release and posterior spinal fusion is one of the most effective techniques to correct three-dimensional curve deformity in severe rigid scoliosis with life-threatening complications such as cardiopulmonary compromise, adjacent organ damage, increased hospital stay, and risk of anesthesia due to two major operative procedures [4,8,9]. The major problem of the combined anterior and posterior approach is the risk of pulmonary dysfunction [4,10,11]. To overcome such complications, we avoided anterior surgery and preferred extended posterior release, facetectomy, and posterior spinal fusion. Several previous studies showed despite many complications and risks, the success rate of anterior release and posterior spinal fusion was significantly good (Kandwal et al. [2]: 77.2%, Bullmann et al. [3]: 67%). Few recent studies reported acceptable correction could be achieved by the posterior-only approach in severe rigid scoliosis. Chang [12] reported 67% deformity correction achieved in severe rigid scoliosis patients with mean Cobbs angle 98° (ranging 75–133°) and Kuklo et al. [13] reported 68% correction in idiopathic scoliosis over 90° by posterior-only approach. Luhman et al. [14] compare between anterior release and posterior spinal fusion with posterior-only fusion in 84 patients for a minimum 2-year follow-up. They reported no significant difference in coronal correction (anterior release and posterior spinal fusion: 48.3 and posterior spinal fusion: 47.5°) with a correction rate of 58.3%. Dobbs et al. [15] conducted a comparative study between AP spinal fusion and posterior spinal fusion utilizing pedical screws in >90° rigid scoliosis showed both groups had similar correction rates (44%). Both studies had no complications such as neurological complications, implant failure, or re-operation. Shi et al. [16] reported no significant difference in the correction rate of severe rigid scoliosis managed by the posterior-only approach and anterioposterior spinal fusion. Our study reported 59.5° of mean correction in severe rigid scoliosis with 62.5% correction rate and minimal complication. Limitations of this study are the small sample size, the nature of the study (retrospective), and the absence of control group. Hence, a randomized controlled trial with a large sample size is required to evaluate the functional outcome of extended posterior release and instrumentation in the future. Despite all the limitations, the current study shows satisfactory functional outcomes in extended posterior release and instrumentation with no major complication in the case of severe rigid scoliosis.
Our study concluded that extended posterior-only release, facetectomy, and posterior spinal fusion by utilizing pedicle screws and pre-contoured rods were significantly corrected severe and rigid scoliosis with a high correction rate and avoided complications of anterior release. Hence, we can achieve remarkable correction in rigid scoliosis using the proper choice of levels, proper implant, and extended posterior release.
Remarkable correction can be achieved in severe rigid scoliotic deformity by proper choice of levels, proper implant, and extended posterior release.
References
- 1.Yamin S, Li L, Xing W, Tianjun G, Yupeng Z. Staged surgical treatment for severe and rigid scoliosis. J Orthop Surg Res 2008;3:26. [Google Scholar | PubMed]
- 2.Kandwal P, Goswami A, Vijayaraghavan G, Subhash KR, Jaryal A, Upendra BN, et al. Staged anterior release and posterior instrumentation in correction of severe rigid scoliosis (Cobb Angle >100 Degrees). Spine Deform 2016;4:296-303. [Google Scholar | PubMed]
- 3.Bullmann V, Halm HF, Schulte T, Lerner T, Weber TP, Liljenqvist UR. Combined anterior and posterior instrumentation in severe and rigid idiopathic scoliosis. Eur Spine J 2006;15:440-8. [Google Scholar | PubMed]
- 4.Kim YJ, Lenke LG, Bridwell KH, Kim KL, Steger-May K. Pulmonary function in adolescent idiopathic scoliosis relative to the surgical procedure. J Bone Joint Surg 2005;87:1534-41. [Google Scholar | PubMed]
- 5.Mirzashahi B, Moosavi M, Rostami M. Outcome of posterior-only approach for severe rigid scoliosis: A retrospective report. Int J Spine Surg 2020;14:232-8. [Google Scholar | PubMed]
- 6.Zhou C, Liu L, Song Y, Liu H, Li T, Gong Q, et al. Anterior release internal distraction and posterior spinal fusion for severe and rigid scoliosis. Spine (Phila Pa 1976) 2013;38:E1411-7. [Google Scholar | PubMed]
- 7.Shen J, Qiu G, Wang Y, Zhang Z, Zhao Y. Comparison of 1-stage versus 2-stage anterior and posterior spinal fusion for severe and rigid idiopathic scoliosis--a randomized prospective study. Spine (Phila Pa 1976) 2006;31:2525-8. [Google Scholar | PubMed]
- 8.Chen Z, Rong L. Comparison of combined anterior-posterior approach versus posterior-only approach in treating adolescent idiopathic scoliosis: A meta-analysis. Eur Spine J 2016;25:363-71. [Google Scholar | PubMed]
- 9.Zhang HQ, Wang YX, Guo CF, Tang MX, Chen LQ, Liu SH, et al. Posterior-only surgery with strong halo-femoral traction for the treatment of adolescent idiopathic scoliotic curves more than 100 degrees. Int Orthop 2011;35:1037-42. [Google Scholar | PubMed]
- 10.Vedantam R, Lenke LG, Bridwell KH, Haas J, Linville DA. A prospective evaluation of pulmonary function in patients with adolescent idiopathic scoliosis relative to the surgical approach used for spinal arthrodesis. Spine ((Phila Pa 1976) 2000;25:82-90. [Google Scholar | PubMed]
- 11.Lenke LG, Bridwell KH, Blanke K, Baldus C. Analysis of pulmonary function and chest cage dimension changes after thoracoplasty in idiopathic scoliosis. Spine (Phila Pa 1976) 1995;20:1343-50. [Google Scholar | PubMed]
- 12.Chang KW. Cantilever bending technique for treatment of large and rigid scoliosis. Spine (Phila Pa 1976) 2003;28:2452-8. [Google Scholar | PubMed]
- 13.Kuklo TR, Lenke LG, O’Brien MF, Lehman RA Jr., Polly DW Jr., Schroeder TM. Accuracy and efficacy of thoracic pedicle screws in curves more than 90 degrees. Spine (Phila Pa 1976) 2005;30:222-6. [Google Scholar | PubMed]
- 14.Luhmann SJ, Lenke LG, Kim YJ, Bridwell KH, Schootman M. Thoracic adolescent idiopathic scoliosis curves between 70 degrees and 100 degrees: Is anterior release necessary? Spine (Phila Pa 1976) 2005;30:2061-7. [Google Scholar | PubMed]
- 15.Dobbs MB, Lenke LG, Kim YJ, Luhmann SJ, Bridwell KH. Anterior/posterior spinal instrumentation versus posterior instrumentation alone for the treatment of adolescent idiopathic scoliotic curves more than 90 degrees. Spine (Phila Pa 1976) 2006;31:2386-91. [Google Scholar | PubMed]
- 16.Shi Z, Chen J, Wang C, Li M, Li Q, Zhang Y, et al. Comparison of thoracoscopic anterior release combined with posterior spinal fusion versus posterior-only approach with an all-pedicle screw construct in the treatment of rigid thoracic adolescent idiopathic scoliosis. J Spinal Disord Tech 2015;28:E454-9. [Google Scholar | PubMed]








