Os odontoideum is a rare condition with limited existing literature. Considering the significant risks involved if conservative management opts, like severe neurodeficit to sudden death on trivial trauma and the recent improvement of imaging tools helping to understand the pathology of the disease, surgery can be indicated even in an incidentally detected Os odontoideum. However, a case-by-case approach can be considered for stable asymptomatic patients depending on factors such as age, activity level, comorbidities, syndromic association, and radiographic findings.
Dr. Rajendra Sakhrekar, Department of Spine Surgery, Yonsei Okay Hospital, Seoul, South Korea. E-mail: raj.sakhrekar1@gmail.com
Introduction: Os odontoideum is a rare condition described radiographically and clinically as a congenital anomaly of the second cervical vertebra (axis). It is a smooth, independent ossicle of variable size and shape separated from the base of a shortened odontoid process by an obvious gap, with no osseous connection to the body of C2.
Material and Methods: This study reviewed the literature on OO to evaluate its etiology, clinical presentations, differential diagnosis, imaging modalities, and outcomes in the management of asymptomatic and symptomatic cases of Os odontoideum. Key articles from PubMed, EMBASE, Google Scholar, and Cochrane were searched.
Discussion: Considering etiology, the traumatic hypothesis is favored over the congenital hypothesis as per recent literature on OO. Clinical presentation varies from asymptomatic to mild neck pain to severe myelopathy and neurodeficit. Various C1-C2 instrumentation and fusion techniques such as wiring, transarticular screw, and laminar screws have been described with success rates.
Conclusion: Os odontoideum is a rare condition with limited existing literature. Considering the significant risks involved if conservative management opts, like severe neurodeficit to sudden death on trivial trauma and the recent improvement of imaging tools helping to understand the pathology of the disease, surgery can be indicated even in an incidentally detected os odontoideum. However, a case-by-case approach can be considered for stable asymptomatic patients depending on factors such as age, activity level, comorbidities, syndromic association, and radiographic findings.
Keywords: Os odontoideum, surgical management, etiology, atlantoaxial instability, complications.
Os odontoideum was first described by Giacomini in 1886 [1]. Bevan and Shepherd in 1863 and Cunningham in 1886 also described OO based on anatomical and autopsy studies [2]. The word os odontoideum is derived from Latin, meaning Os (bone) and Odontoideum (tooth-like). It is a rare condition, described radiographically and clinically as a congenital anomaly of the second cervical vertebra (axis). It is a smooth, independent ossicle of variable size and shape separated from the base of a shortened odontoid process by a noticeable gap, with no osseous connection to the body of C2. It is classified variously depending on anatomy, stability, etiology, and symptomatology. It is classified anatomically into two types, dystopic and orthotopic, according to Fielding and Griffin in 1980 [3,4]. In the dystopic type, OO is fused to the basion, while in the orthotopic, OO lies in the normal position on the odontoid process and moves with the atlas anterior arch. Based on the extent of excursion of the atlas from the axis on dynamic imaging, it is classified as stable or unstable. It is classified etiologically as congenital and post-traumatic. OO has been classified as asymptomatic or symptomatic depending on clinical presentation and an increasing risk of cervical-medullary compression [5-7]. This study tries to review and address the various controversies regarding the etiology and management options of os odontoideum.
We reviewed the literature on OO to evaluate its etiology, clinical presentations, differential diagnosis, imaging modalities, and outcomes in managing asymptomatic and symptomatic cases of Os odontoideum. PubMed, EMBASE, Google Scholar, and Cochrane key articles were searched. Keywords such as “Os Odontoideum,” “surgical management,” “etiology,” “Atlanto-axial instability,” and “complications” were used. Additional articles were identified by manually checking the references. Two independent reviewers reviewed the articles.
Pathophysiology
The etiology of the OO has always remained controversial since its description in the 19th century. The etiologies proposed are congenital or traumatic. However, the current evidence from the literature supports the traumatic over the congenital hypothesis more. The authors supporting the congenital hypothesis describe OO results from a failure of fusion of the dens with the body of the axis during embryonic development or failure of fusion of the secondary ossification center at the apex with its central part of the dens or the failure of proper caudal migration of the dens during development. The congenital OO etiology is further supported by its presence in identical twins and siblings and its association of OO with many congenital syndromes such as Down’s syndrome, Morquio’s disease, achondroplasia, Klippel–Feil syndrome, Larson syndrome, and other associated anomalies at the craniovertebral junction (CVJ) with no significant history of trauma. The congenital hypothesis was debated as the neurocentral synchondrosis is located below the level of the superior articulating facet. In contrast, the gap in OO is frequently located above the plane of the superior articulating facet [7-9]. Fielding and Griffin proposed the acquired/post-traumatic/vascular hypothesis in the 1980s, describing the formation of OO due to an unrecognized fracture of the odontoid after a trivial fall in childhood. The subsequent contraction of the apical and alar ligaments, the distraction of the fractured fragment, and then reducing or detaching the blood supply gave rise to the OO [3,4].
OO is more commonly seen among males in the second and third decades. The clinical presentation in OO patients is highly variable, ranging from incidental findings in asymptomatic patients to local symptoms such as neck pain, restriction of neck movements, shoulder pain, torticollis, and occipital headaches. There are also cervical myelopathic symptoms and signs such as weakness, paresthesia, ataxia, urinary complaints, and symptoms related to vertebra-basilar ischemia [10].
Differential diagnosis of OS
Based on clinical presentation, differential diagnosis of OO can vary from cervical spondylosis, mechanical neck pain, degenerative disc disease, or atlantoaxial subluxation as seen in rheumatoid arthritis. It could also be confused with acute fracture of dens. However, OO could be ruled out on the history itself by the absence of a significant history of falls or trauma and depending on radiological characteristics like the smooth surface of the ossicle and the below body of C2 and also the presence of sclerosis and hypertrophy of the anterior tubercle of the atlas [7,8].
Imaging and indicators of instability are shown in Figure 1.
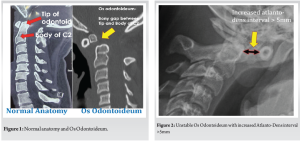
OO can be diagnosed on plain radiographs with the anteroposterior, lateral neutral, and dynamic views (flexion and extension) and open mouth view. In addition to plain lateral radiographs, computed tomography (CT) of the CVJ to understand bony anatomy and abnormalities, CT angiography to study the course of the vertebral artery, and magnetic resonance imaging (MRI) of the CVJ to look for cord and soft tissue compression and anomalies. Recently, using kinematic MRI to diagnose OO was advised by Hughes et al. [11]. A recent article by Goyal et al. described the criteria for atlantoaxial instability.
- Atlanto-dens interval of more than 5 mm [Fig. 2]
- Overriding of the anterior arch of the atlas over the odontoid
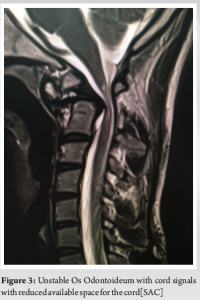
- Space available for the cord of <13 mm [Fig. 3]
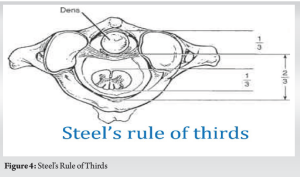
- Violation of the Steel’s rule of thirds (one-third cord, one-third odontoid, and one-third safe space) [Figure 4]
- Translation of the tip of the odontoid of more than 4 mm of the basion
Management
The American Association of Neurological Surgeons and the Congress of Neurological Surgeons provided evidence-based clinical recommendations for treating os odontoideum in 2001 [14,15].
- No clinical evidence was found supporting the recommendation of operative treatment standards or guidelines for os odontoideum.
- For asymptomatic patients, clinical and radiographic surveillance may be the appropriate management.
- Patients with neurological symptoms/signs and C1–2 instability are generally managed with posterior fixation and fusion.
- Other operative measures may be warranted in irreducible cervicomedullary compression and/or occipitocervical instability.
- The lack of high-quality studies was noted
Evidence-based clinical studies recommend surgical management in symptomatic OO patients (e.g., cervical myelopathy). Although, controversy still exists in the management of asymptomatic patients. In 1982, Spierings and Braakman [16] noted high mortality in OO patients who were treated with surgical management. Hence, the authors suggested conservative treatment in more than 60% of their cases, including asymptomatic patients. In 2000, Dai et al. [6]. suggested that five asymptomatic OO cases managed conservatively remained stable at follow-up. In 2008, Klimo et al. [8,9] contradictorily believed that stressful events can easily cause spinal cord injury. Regardless of the clinical presentation, Klimo et al. recommended surgical intervention in OO. Literature has suggested in asymptomatic stable OO patients, even a trivial trauma could lead to significant neurological deficit or death [17,18,19].
Surgical techniques
Various surgical techniques have been advised, like
- Occiput-cervical fusion is rarely used as it reduces the range of motion
- C1–C2 sublaminar wiring techniques
- C1–C2 Clamps, Hooks, and Claws
- C1–C2 transarticular screw
- C1 lateral mass—C2 pars screw with plates (Goel technique)
- C1 lateral mass—C2 lamina screw
- C1 lateral mass screw–C2 pedicle screw fixation with rods (Harms technique)
- With C2 intralaminar screw fixation
- C1–2 interfacet spacers with C1–2 fixation
C1–C2 wiring
Gallie et al. [20,21] 1939 described the C1–2 wiring technique elaborately. In this technique, wires are passed under the lamina of the C1 arch and hooked to the spinous process of C2. The tricortical iliac crest bone graft is compressed between C1 and C2 to achieve fusion. In 2002, Brookmeyer et al. recently used cables instead of wires for C1–C2 stabilization. The inability to correct rotatory forces, non-union, and gradual loss of reduction is significant drawbacks of this technique. Recently, a few authors described the use of hooks at the C1 posterior arch to improve the stability and strength of the construct.
C1–C2 trans articular screw instrumentation
Magerl et al. [22] in 1987 demonstrated C1–C2 transarticular screw technique. It provides a biomechanically solid and stable construct in comparison with C1–C2 wiring. Although a long learning curve, technically demanding precision and accuracy, and risk of neurovascular injuries like high riding vertebral artery injury, this technique has shown promising results over the years [23].
C1 lateral mass and C2 pars screw instrumentation
Goel and Laheri [24] 1994 described C1 lateral mass and C2 pars screw with plate instrumentation with good results. Harms and Melcher [25] modified this technique with the use of polyaxial screws and a rod system. This technique showed a relatively easy learning curve and good clinical and radiological outcomes. It is one of the safest, most reproducible, most accepted, and widely used procedures in the current literature.
C1 lateral mass-C2 lamina screw
In some instances, a high-riding vertebral artery increases the risk of injury. In such a scenario, the use of C2 laminar screws is well described with good outcomes.
Limitations
This study has a few limitations. This study is not a systematic review, so the evidence about each debatable issue is insufficient. However, this study will provide the current concept about etiology and current concepts in the management of os odontoideum. Furthermore, this study could not suggest specific guidelines because more highly qualified, relevant studies were needed.
Os odontoideum is a rare condition with limited existing literature. The etiology is debatable, but recent literature favors the acquired/post-traumatic/vascular hypothesis. OO could present with broad manifestations of symptoms; precise clinical and radiological diagnosis could help in OO treatment and prevent likely devastating complications. Considering the significant risks involved if conservative management opts like severe neurodeficit to sudden death on trivial trauma and the improvement of imaging tools helping to understand the pathology of the disease, the morphology of the nearby vital structure along with the relative safety of the current surgical procedures, surgery can be indicated even in an incidentally detected os odontoideum. However, a case-by-case approach can be considered for stable asymptomatic patients depending on factors such as age, activity level, comorbidities, syndromic association, and radiographic findings.
Os odontoideum is a rare congenital anomaly of the second cervical vertebra with the significant risks involved if conservative management is opted, a case-by-case approach can be considered for stable asymptomatic patients depending on factors such as age, activity level, comorbidities, syndromic association, and radiographic findings.
References
- 1.Giacomini C. Sull’esistenza dell’ “Os odontoideum” nell’uomo. Gior Accad Med Torino 1886;49:24-8. [Google Scholar | PubMed]
- 2.Bevan WL, Shepherd SW. A Dictionary of the Bible: Comprising its Antiquities, Biography, Geography, and Natural History. Boston, MA, USA: Houghton Mifflin and Company; 1863. p. 1268-70. [Google Scholar | PubMed]
- 3.Fielding JW, Griffin PP. Os odontoideum: An acquired lesion. J Bone Joint Surg Am 1974;56:187-90. [Google Scholar | PubMed]
- 4.Fielding JW, Hensinger R, Hawkins R. Os odontoideum. J Bone Joint Surg Am 1980;62:376-83. [Google Scholar | PubMed]
- 5.Ricciardi JE, Kaufer H, Louis DS. Acquired Os odontoideum following acute ligament injury. Report of a case. J Bone Joint Surg Am 1976;58:410-12. [Google Scholar | PubMed]
- 6.Dai L, Yuan W, Ni B, Jia L. Os odontoideum: Etiology, diagnosis, and management. Surg Neurol 2000;53:106-9. [Google Scholar | PubMed]
- 7.Jumah F, Alkhdour S, Mansour S, He P, Hroub A, Adeeb N, et al. Os odontoideum: A comprehensive clinical and surgical review. Cureus 2017;9:e1551. [Google Scholar | PubMed]
- 8.Klimo P Jr., Kan P, Rao G, Apfelbaum R, Brockmeyer D. Os odontoideum: Presentation, diagnosis, and treatment in a series of 78 patients. J Neurosurg Spine 2008;9:332-42. [Google Scholar | PubMed]
- 9.Klimo P Jr., Coon V, Brockmeyer D. Incidental Os odontoideum: Current management strategies. Neurosurg Focus 2011;31:E10. [Google Scholar | PubMed]
- 10.Goel A, Patil A, Shah A, Dandpat S, Rai S, Ranjan S. Os odontoideum: Analysis of 190 surgically treated cases. World Neurosurg 2020;134:e512-23. [Google Scholar | PubMed]
- 11.Hughes TB Jr., Richman JD, Rothfus WE. Diagnosis of Os odontoideum using kinematic magnetic resonance imaging. A case report. Spine (Phila Pa 1976) 1999;24:715-8. [Google Scholar | PubMed]
- 12.Goel A. Indicators of atlantoaxial instability. J Craniovertebr Junction Spine 2021;12:103-6. [Google Scholar | PubMed]
- 13.Lacy J, Bajaj J, Gillis CC. Atlantoaxial Instability. Treasure Island, FL: StatPearls Publishing; 2021. [Google Scholar | PubMed]
- 14.The Section on Disorders of the Spine and Peripheral Nerves of the American Association of Neurological Surgeons and the Congress of Neurological Surgeons Os Odontoideum; 2001. Available from: http://www.spineuniverse.com/pdf/traumaguide/19.pdf [Google Scholar | PubMed]
- 15.Wilson JR, Dettori JR, Vanalstyne EM, Fehlings MG. Addressing the challenges and controversies of managing Os odontoideum: Results of a systematic review. Evid Based Spine Care J 2010;1:67-74. [Google Scholar | PubMed]
- 16.Spierings EL, Braakman R. The management of Os odontoideum. Analysis of 37 cases. J Bone Joint Surg Br 1982;64:422-8. [Google Scholar | PubMed]
- 17.McGoldrick JM, Marx JA. Traumatic central cord syndrome in a patient with Os odontoideum. Ann Emerg Med 1989;18:1358-61. [Google Scholar | PubMed]
- 18.Dempster AG, Heap SW. Fatal high cervical spinal cord injury in an automobile accident complicating Os odontoideum. Am J Forensic Med Pathol 1990;11:252-6. [Google Scholar | PubMed]
- 19.Zhang Z, Zhou Y, Wang J, Chu T, Li C, Ren X, et al. Acute traumatic cervical cord injury in patients with Os odontoideum. J Clin Neurosci 2010;17:1289-93. [Google Scholar | PubMed]
- 20.Rahimizadeh A, Rahimizadeh A. Os odontoideum: Review article. Orthop Res Traumatol Open J 2016;1:33-55. [Google Scholar | PubMed]
- 21.Goyal N, Bali S, Ahuja K, Chaudhary S, Barik S, Kandwal P. Posterior arthrodesis of atlantoaxial joint in congenital atlantoaxial instability under 5 years of age: A systematic review. J Pediatr Neurosci 2021;16:97-105. [Google Scholar | PubMed]
- 22.Magerl F, Seemann PS. Stable posterior fusion of the atlas and axis by transarticular screw fixation. In: Cervical Spine I. New York: Springer; 1987. p. 322-7. [Google Scholar | PubMed]
- 23.Gluf WM, Brockmeyer D L. Atlantoaxial transarticular screw fixation: A review of surgical indications, fusion rate, complications, and lessons learned in 67 pediatric patients. J Neurosurg Spine 2005;2:164-9. [Google Scholar | PubMed]
- 24.Goel A, Laheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir (Wien) 1994;129:47-53. [Google Scholar | PubMed]
- 25.Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976) 2001;26:2467-71. [Google Scholar | PubMed]