The article emphasizes the necessity of a multidisciplinary approach and innovative surgical techniques in managing aseptic ulnar diaphyseal non-union in patients with concurrent seizure disorders.
Dr. Ashu Malhotra, Orthopaedic Registrar, Department of Orthopaedic Surgery, Maa Ram Pyari Ortho Centre, Ranchi - 834 001, Jharkhand, India. E-mail: ashu.malhotra0079@gmail.com
Introduction: Aseptic ulnar diaphyseal non-union presents a complex challenge in orthopedic practice, particularly when compounded by concurrent seizure disorders. This case report highlights the unique considerations and innovative approaches in managing such cases, emphasizing the importance of interdisciplinary collaboration and tailored treatment strategies.
Case Report: We present the case of a 35-year-old male with a history of recurrent ulnar fractures and generalized tonic-clonic seizures. Through a multidisciplinary approach involving orthopedics, neurology, and rehabilitation services, we successfully managed aseptic ulnar diaphyseal non-union while addressing the patient’s seizure disorder. Implant removal, fibula grafting, elastic nailing, and bridging fixation with a locking compression plate were employed, leading to favorable outcomes at the final follow-up.
Conclusion: The management of aseptic ulnar diaphyseal non-union in patients with concurrent seizure disorders requires a nuanced and multidisciplinary approach. This case underscores the importance of individualized treatment strategies, interdisciplinary collaboration, and innovative surgical techniques in achieving successful outcomes. Sharing our experience aims to contribute to the existing literature and inform clinical practice in addressing similar challenging scenarios.
Keywords: Aseptic non-union, ulnar fracture, seizure disorder, elastic nail, fibula grafting.
Aseptic ulnar diaphyseal non-union poses a significant challenge in orthopedics practice, often requiring complex treatment strategies to achieve successful outcomes. When coupled with comorbidities such as seizure disorders, the management becomes even more intricate due to the potential complications and limitations imposed by the underlying condition [1]. In this case report, we present a compelling instance of aseptic ulnar diaphyseal non-union in a patient with concurrent seizure disorder, highlighting the unique consideration and innovative approach employed to achieve a successful union. Patients with seizure disorders are prone to musculoskeletal injuries, often resulting from seizure-related falls or trauma, which may lead to fractures and subsequent complications such as non-union [1]. Furthermore, the management of fractures and non-unions in these patients is complicated by the potential interactions between antiepileptic medications and orthopedic interventions, as well as the risk of perioperative seizures and delayed healing [1,2]. Despite the growing recognition of the interplay between seizure disorders and orthopedic conditions, there remains a paucity of literature addressing the optimal management of aseptic ulnar diaphyseal non-union in this unique patient population. By presenting this case, we aim to contribute to the existing knowledge base and provide insights into the challenges encountered and strategies employed in managing such complex scenarios. Through a multidisciplinary approach involving orthopedics surgery, neurology, and rehabilitation services, we successfully navigated the intricacies of treating aseptic ulnar diaphyseal non-union in the context of seizure disorder, ultimately achieving favorable outcomes for the patient. In the subsequent sections of this report, we will detail the clinical presentation, diagnostic evaluation, therapeutic interventions, and outcomes of our case, elucidating the nuances of managing aseptic ulnar diaphyseal non-union in the setting of a concurrent seizure disorder. We believe that this case adds valuable insights to the existing literature and informs clinical practice in addressing similar scenarios.
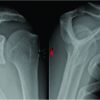
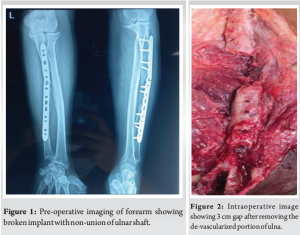
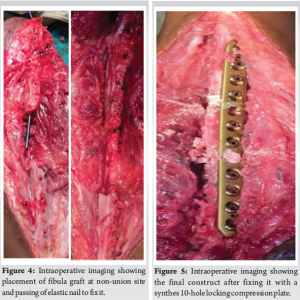
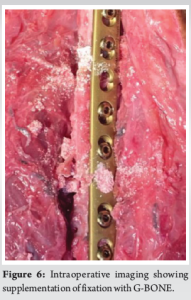
A 35-year-old male, daily wage labor belonging to low socioeconomic status, came with complaints of swelling and pain in his left forearm persisting for the past 5 months following an episode of generalized tonic-clonic seizure. His medical history was suggestive of generalized tonic-clonic seizure for which he was taking combined doses of lamotrigine and valproate as prescribed by his neurologist. Family medical history was significant for parents with similar seizure disorders. The patient had a history of recurrent ulnar fractures having experienced three previous surgeries. In previous instances, the patient underwent operative management with open reduction and internal fixation using a locking compression plate (LCP). He reported that he was working at a construction site where he had an episode of seizure and he fell down. His coworkers took him to the neurologist who intervened promptly and his seizure subsided. He was splinted with a plaster of Paris slab and had follow-up arrangement with the orthopedic surgeon. Instead, the patient’s father had previous surgical treatment with the corresponding author and scheduled follow-up 5 months after the injury. On physical examination, the patient was a 5’10”, 172 lb male with a healthy appearance. The left forearm was noted to have a swelling at the ulnar border of the middle forearm. The skin was intact. The patient had a sharp palpable gap at the mid-forearm region along with local tenderness. There was a notable decrease in pronation and supination compared to the unaffected limb. Neurovascular status was within normal limits. Radiograph of the forearm in anteroposterior and lateral views was performed which revealed a broken LCP with evidence of non-union at fracture site (Fig. 1). Basic blood investigations along with erythrocyte sedimentation rate and C-reactive protein were done. Given the diagnosis of aseptic ulnar diaphyseal non-union with implant failure, the treatment plan involved implant removal and re-fixation of the fracture site. The patient was admitted and after undergoing a thorough pre-operative workup by the anesthetist, he was posted for implant removal and re-fixation with LCP and bone grafting under interscalene block. The patient had a tourniquet applied to the left arm and inflated to 230 mmHg post-exsanguination using an eschmarch bandage during the procedure. We took a standard subcutaneous approach to the ulnar shaft using a straight incision across the non-union site. The plane was made between extensor carpi ulnaris and flexor carpi ulnaris. The implant and fracture site were exposed thoroughly. Implant was removed and the fracture site was assessed for vascularity. To our surprise, 3 cm of non-union site had no vascularity when assessed with drill holes for local signs of bleeding and so this part of ulnar shaft was removed (Fig. 2). We harvested non-vascularized fibula graft from ipsilateral lower limb (Fig. 3), placed it at the fracture site, and passed an elastic nail of 3 mm from olecranon passing through the graft and ulnar shaft (Fig. 4). Finally, a synthes long 10-hole 3.5 mm LCP plate was used and fixed in bridging mode using locking screws across the non-union site (Fig. 5). Four screws were put in proximal shaft, two in the graft site and four in the distal shaft of ulna. The fixation was supplemented with hydroxyapatite granules (G-Bone) (Fig. 6). The patient was kept under observation for 1 day post-surgery and discharged comfortably. The patient received first-generation IV cephalosporin antibiotic for 24 h. Postoperatively, during his stay at the hospital. Postoperatively, arm was protected in an arm pouch and physiotherapy in the form of gentle range of motion exercises was done for 3 weeks. Meanwhile, the patient continued his antiepileptic medications as prescribed by the neurologist. Regular follow-up at 1 month, 3 months, 6 months, and 1 year post-surgery was done. X-ray at final follow-up after 1 year revealed complete union at the fracture site (Fig. 7) with an acceptable range of motion as compared to the unaffected limb (Fig. 8).


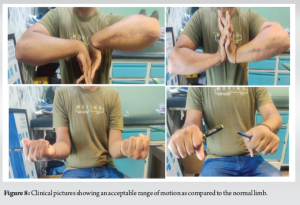
The management of aseptic ulnar diaphyseal non-union in patients with concurrent seizure disorders presents a multifaceted clinical challenge. The incidence of non-union in diaphyseal forearm fractures is 2–10% [3]. The incidence in epileptic patients could not be elicited even after a thorough literature review. Aseptic non-union of the ulnar diaphysis is inherently complex, often requiring a tailored treatment approach to achieve successful outcomes [4]. Our case exemplifies the challenges encountered and the innovative strategies employed to address both fracture healing and seizure control simultaneously. Seizure disorders predispose individuals to musculoskeletal injuries, including fractures, which can lead to non-union if left untreated [5]. The recurrence of ulnar fractures in our patient underscores the impact of seizure-related falls on skeletal integrity. Moreover, the use of antiepileptic medications introduces additional considerations, including potential drug interactions and the risk of perioperative seizures, which can complicate fracture management and healing. Enzyme (cytochrome p450 system) inducing AEDs such as phenobarbital, carbamazepine, and phenytoin has been associated with adverse effects on bone mineralization and calcium metabolism. These drugs upregulate enzymes responsible for Vitamin D metabolism, leading to reduced calcium absorption and secondary hyperparathyroidism. This may impact fracture healing and ultimately lead to non-union in the long run [6]. The decision to proceed with implant removal and re-fixation, supplemented by fibula grafting, reflects the adaptability of surgical techniques to address compromised vascularity and promote osseous healing. Despite the avascularity observed in the non-union site, the fibula graft served as a viable solution, demonstrating the importance of innovative approaches in challenging cases. Both elastic nailing and LCP were employed in a bridging mode to promote secondary enchondral ossification in our case. No advantage was found for the use of plaster after internal fixation, unlike De Buren’s findings (1962) [7]. The bridging fixation with a LCP provided essential biomechanical stability, facilitating union while minimizing the risk of implant failure. In a paper by Brakenbury et al., they used 6-hole AO, 6-hole Sherman and Silver bone graft to fix isolated ulnar diaphyseal non-union [8]. After the initial procedure for non-union, 11 out of 15 fractures successfully united, indicating a union rate of 73.3% [8]. Treatment using either plating alone or internal fixation combined with grafting resulted in a union rate of 92%, a figure similar to that documented by Boyd and Lipinski in 1960 [9]. Following a subsequent operation, one fracture achieved union. We propose that rigid fixation, either alone as suggested by Hicks in 1977, or in conjunction with bone grafting, represents the most effective treatment modalities [10]. Boyd and Lipinski’s 1960 study emphasized infection as the primary cause of persistent non-union, although it is uncommon in ulnar fractures, manifesting in only two cases. One of these cases achieved a successful union, while the other remained in persistent non-union. The attainment of union is paramount as non-union leads to significant disability in the affected arm. Regular follow-up evaluations allowed for the assessment of union progression and facilitated timely interventions as needed. The successful union observed at the final follow-up underscores the efficacy of the multidisciplinary approach employed in our patient’s care. Furthermore, the insights gained from this case contribute to the evolving understanding of managing complex orthopedic conditions in patients with seizure disorders. The management of aseptic ulnar diaphyseal non-union in patients with concurrent seizure disorders requires a nuanced approach, encompassing meticulous pre-operative planning, interdisciplinary collaboration, and innovative surgical techniques. This case contributes to the evolving understanding of managing complex orthopedic conditions in the context of neurological comorbidities and emphasizes the importance of individualized treatment strategies tailored to patient-specific needs.
Managing aseptic ulnar diaphyseal non-union in patients with concurrent seizure disorders demands a nuanced, multidisciplinary approach. Our case study involving a 35-year-old male demonstrated success using a fibula graft and elastic nail alongside a plate, offering a promising solution. Sharing our experience aims to enrich literature and guide clinical practice in similar complex cases.
Managing aseptic ulnar diaphyseal non-union in seizure patients requires tailored treatment strategies and interdisciplinary collaboration to optimize the outcomes.
References
- 1.Vestergaard P, Tigaran S, Rejnmark L, Tigaran C, Dam M, Mosekilde L. Fracture risk is increased in epilepsy. Acta Neurol Scand 1999;99:269-75. [Google Scholar | PubMed]
- 2.Yen WW, Cloud GW, Wasserburg JR, Penny GS, Day LM, Pascal SC, et al. A systematic review of the management of upper extremity orthopaedic injuries in epileptic patients. Arch Bone Jt Surg 2022;10:301-10. [Google Scholar | PubMed]
- 3.Dimartino S, Pavone V, Carnazza M, Cuffaro ER, Sergi F, Testa G. Forearm fracture nonunion with and without bone loss: An overview of adult and child populations. J Clin Med 2022;11:4106. [Google Scholar | PubMed]
- 4.Kloen P, Wiggers JK, Buijze GA. Treatment of diaphyseal non-unions of the ulna and radius. Arch Orthop Trauma Surg 2010;130:1439-45. [Google Scholar | PubMed]
- 5.Yen WW, Falik N, Passfall LG, Krol O, Sanchez TE, Penny GS, et al. Management of lower extremity orthopaedic injuries in epileptic patients: A systematic review. J Orthop 2021;25:278-82. [Google Scholar | PubMed]
- 6.Meier C, Kraenzlin ME. Antiepileptics and bone health. Ther Adv Musculoskelet Dis 2011;3:235-43. [Google Scholar | PubMed]
- 7.De Buren N. Causes and treatment of nonunion in fractures of the radius and ulna. J Bone Joint Surg 1962;44B:614-25. [Google Scholar | PubMed]
- 8.Brakenbury PH, Corea JR, Blakemore ME. Non-union of the isolated fracture of the ulnar shaft in adults. Injury 1981;12:371-5. [Google Scholar | PubMed]
- 9.Boyd HB, Lipinski SW. Causes and treatment of non-union of the shafts of the long bones with a review of 74 I patients. Instr Course Lect 1960;17:165. [Google Scholar | PubMed]
- 10.Hicks JH. Rigid fixation as a treatment for hypertrophic non-union. Injury 1977;8:199. [Google Scholar | PubMed]