Prompt surgical irrigation and debridement for a clinical diagnosis of left upper extremity gas gangrene led to an overall positive outcome for the patient despite having to undergo a proximal trans-humeral amputation.
Dr. Mark LaGreca, Department of Orthopaedic Surgery, Philadelphia College of Osteopathic Medicine, Philadelphia, Pennsylvania. E-mail: ml194690@pcom.edu
Introduction: Gas gangrene is a rare, often lethal infection of soft tissue that is commonly associated with the Clostridial species due to penetrating injuries. Case reports of spontaneous atraumatic gas gangrene due to the Clostridium septicum species are exceedingly rare. Atraumatic C. septicum is notably related to bowel pathologies, immunodeficiencies, and individuals with vascular insufficiency. The rapid progression of Clostridium myonecrosis contributes to its high mortality rates.
Case Report: The authors report a case of a 71-year-old right-hand-dominant female who developed fulminant atraumatic left forearm pain and swelling. The patient was indicated for emergent irrigation and debridement (I&D) of the left upper extremity. She was later found to have C. septicum bacteremia and required multiple I&Ds including the left side of the neck and chest wall. Repeat post-operative examinations revealed no motor function or sensation distal to the elbow and she was subsequently indicated for a proximal trans-humeral amputation.
Conclusion: Although she had a prolonged hospital stay, she progressed well and was eventually discharged to a rehabilitation facility. This case report highlights the importance of early recognition of Clostridial myonecrosis as well as the need for emergent surgical intervention for the patient’s survival.
Keywords: Trans-humeral amputation, gas gangrene, Clostridium septicum infection.
“Gas gangrene” is most commonly associated with the Clostridial species, especially the Clostridium perfringens, Clostridium novyi, and Clostridium septicum species. The infection spreads quickly from the epidermis to the deep muscles and is accompanied by high rates of mortality, which have been reported as high as 56% [1]. Traumatic cases are most common and are associated with large penetrating injuries, such as gunshot wounds or blast injuries such as those sustained on the battlefield, which leads to rapid infection spread. Atraumatic cases are associated with C. septicum species. This etiology of gas gangrene is commonly associated with bowel pathologies, immunodeficiencies, and individuals with vascular insufficiency [2,3]. Given its high rates of mortality, surgeons must have a high level of suspicion, to identify and treat atraumatic C. septicum with emergent irrigation and debridement (I&D). The authors present a case of atraumatic C. septicum myonecrosis in a 71-year-old female who underwent extensive and emergent surgical fasciotomy, I&D, and subsequent proximal transhumeral amputation of the left upper extremity. She progressed well and was eventually discharged from the hospital after 30 days of stay at a rehabilitation facility.
A 71-year-old right-hand-dominant female with a past medical history of hypertension, type 2 diabetes mellitus (T2DM), and hyperlipidemia presented to the emergency department (ED) with acute onset of left forearm pain that awoke her from sleep. Her T2DM was relatively controlled, as her last HbA1c measured with her primary care physician 2 months before the ED presentation was 6.8%. She denied a family or personal history of bowel pathologies. Upon chart review, her only significant related gastrointestinal complaint was diarrhea 2 months before presentation that her primary care provider attributed to viral gastroenteritis.
Upon presentation in the ED, she denied fevers, chills, or recent trauma to her forearm. She also denied sensory changes or weakness in the left upper extremity. She reported that the pain was worse on palpation and with movement. Initial examination in the ED showed signs of discoloration along the volar aspect of the distal forearm but no obvious breaks in the skin or blister formation (Fig. 1a and b). The patient’s examination was significant for pain out of proportion on palpation to the dorsum of the forearm. Compartments of the left upper extremity were soft and compressible. At this time, she was noted to have a painless range of motion over her elbow, forearm, wrist, hand, and fingers.
Several hours later, on repeat examination, the patient developed marked swelling, hyperpigmentation of the skin, and bullae were observed from the wrist to just proximal to the antecubital fossa (Fig. 2a and b). The patient was subsequently started on broad-spectrum antibiotics in the ED, which included vancomycin, piperacillin-tazobactam, and clindamycin. The hand surgery team was consulted at this time. The patient was evaluated by the orthopedic resident on call who noted subcutaneous emphysema on palpation, and again pain out of proportion to palpation along the length of the forearm. Radiographs of the wrist and forearm were obtained and demonstrated subcutaneous gas in the left forearm and wrist (Fig. 3a, b, c, d). A diagnosis of gas gangrene was made at this time and the patient was immediately taken to the operating room (OR) for emergent fasciotomy, carpal tunnel release, and I&D of the left upper extremity. A clinical post-operative photograph of the extensive I&D is shown in Fig. 4.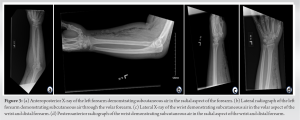
Operative intervention and clinical course
A modified flexor carpi radialis (FCR) approach was taken and a copious amount of exudate was identified with bubbles of air. Infected soft tissue, including part of the FCR, that appeared dusky and necrotic was debrided and excised. Tissue samples were obtained and sent for culture. Due to the extensive nature of the infection, the initial incision was then extended proximally toward the bicipital groove and subsequently to the medial epicondyle of the elbow. While the deep flexor tendons of the hand appeared to be intact, the median nerve was observed to be dusky. Next, attention was turned more proximally as the dissection was carried out from the medial epicondyle, proximally toward the axilla. Extensive skin flaps were made, and partial debridement of the biceps and triceps muscle bellies from necrotic tissue was performed. Upon confirming that the infection did not appear to have spread more proximally, a dorsal incision was then made along the hand between the first and second web space where inflammatory fluid and bubbles of air were noted along the abductor pollicis muscle. This area was debrided and irrigated. Next, a carpal tunnel release was performed through a 3 cm incision along the ulnar border of the 3rd digit. Following the carpal tunnel release, further debridement and irrigation with four liters of saline were performed. Sterile dressings were applied and the patient was taken to the surgical intensive care unit.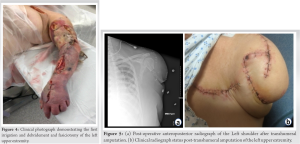
Due to concerns about source control following the initial surgery, a computed tomography scan was done on the patient’s chest and neck which demonstrated subcutaneous gas throughout the left chest wall and neck. The patient returned to the OR on the 2nd day of her hospitalization for extensive left chest wall, neck, and left axilla exploration by the general surgery team. On the 4th day of hospitalization, blood cultures revealed C. septicum infection. The bacteria’s susceptibilities resulted and the patient was started on ampicillin-sulbactam per infectious disease (ID) recommendations. The patient continued to improve clinically. However, continued physical examinations demonstrated that the left upper extremity from the elbow, distally, appeared to be cold and dusky without palpable radial and ulnar pulses. In addition, the patient reported loss of sensation and motor function distal to the elbow and it was deemed that a proximal transhumeral amputation would be required. This was performed on the 8th day of her hospitalization. The left arm was amputated 7.5 cm distal to the glenohumeral joint. A cuff of the deltoid and pectoralis major and minor muscles were left. The pectoralis major was tenodesed to the deltoid cuff and a final thorough debridement was performed on the remaining soft tissue and proximal humerus of the extremity at this time (Fig. 5a and b). The patient tolerated the procedure well and was placed on a course of amoxicillin-clavulanate for 6 days post-operatively per ID. She also was evaluated by the colorectal team who performed a colonoscopy and was found to have multiple polyps which were thought to be the origin of her C. septicum infection. The patient was then discharged to a rehabilitation facility after 30 days of hospitalization. She was unfortunately lost to surgical follow-up. Upon obtaining consent for the submission of this case report, the patient was asked multiple short questions and stated that she was feeling well without pain in the LUE. She was fitted for a mechanical prosthesis for the LUE and reports good functionality with her current prosthesis.
Epidemiology and prevalence
There are approximately 1000 reported cases of clostridial myonecrosis in the United States each year [4]. Of these cases, <10% are of atraumatic causes [5,6], which are most often attributed to C. septicum. A previous literature review of non-traumatic C. septicum myonecrosis in adults reports that the median age of infection was 67 years and 68% were reported to be men [7]. The survival rates for C. septicum myonecrosis are low, with mortality rates as high as 60% and if not acted upon quickly, many patients die in <24 h [7-9]. It is imperative that the patient is taken to the OR emergently to give the patient the best possible chance at survival and gain source control.
Pathophysiology of the toxin and atraumatic causes of C. septicum
The pathophysiology of C. septicum that causes gas gangrene is in its ability to form spores and its four exotoxins α, β, γ, and δ. The α toxin is reported to be responsible for tissue necrosis and hemolysis [8]. The atraumatic nature of Clostridial myonecrosis and its strong relation to bowel pathologies is explained by the bacteria’s favorable spore germination in hypoxic and acidic environments, such as those found in tumors [8]. From the initial bacterial infection in bowel pathologies, it is thought that the bacteria spread hematogenously to other areas of the body, namely the extremities. In addition, C. septicum is 300 times more aerotolerant when compared to C. perfringens, which contributes to why it is able to cause tissue destruction in healthy, non-traumatized tissues [10].
Initial presentation and rapid progression
The initial presentation of atraumatic C. septicum myonecrosis before the presentation of bullae or crepitus varies greatly between reported cases. Pain is the most commonly reported symptom, in 100% of patients, whereas only 56% of patients reported fever [7]. Important vital and physical signs to heighten suspicion of Clostridial myonecrosis include pain disproportionate to physical examination, tachycardia, and erythematous skin changes. This initial presentation can rapidly progress to shock, cardiovascular collapse, and death [9]. This is due to C. septicum’s short incubation period of 6 h to 3 days and the speed at which the infection migrates across fascial planes, at 2–3 cm/h [2,11].
Emergent evaluation and treatment
The comprehensive collection of the patient’s history repeated physical examinations, and a high index of suspicion by the orthopedic surgery resident resulted in the patient being appropriately treated emergently in the OR. Furthermore, surgical intervention was not delayed for confirmation of laboratory values, imaging, or cultures, which ultimately resulted in the patient surviving this rapidly progressing illness. It has been reported that aggressive surgical intervention improved rates of survival in patients with atraumatic clostridial myonecrosis, according to Hermsen et al. Fifty-seven percent of individuals survived if they had surgery compared to 26% survival in those who did not undergo operative intervention [9]. In addition, while a past medical history of diabetes mellitus or cancer diagnosis at the time of presentation did not influence survival rates, understanding that this patient population has an even higher risk of acquiring soft tissue infections should heighten clinical suspicion [9].
Proximal trans-humeral amputation
A proximal humerus amputation may seem dire in this situation, but knowing the speed in which the bacteria progresses and the high rates of mortality, aggressive surgical intervention becomes a necessity for survival. Despite the patient experiencing significant morbidity from this infection, her survival after Clostridial myonecrosis represents an overall positive outcome. This good outcome demonstrates the need for clinicians to have a high index of suspicion for frequent monitoring of symptoms after presentation, and for emergent surgical intervention to be performed once a clinical diagnosis is made. Things to consider when deciding to perform a transhumeral amputation include edema, residual limb pain, phantom limb pain, cosmetic appearances, contracture formation, neuroma, and skin breakdown [12]. It is also important to consider the length of the arm preserved in a transhumeral amputation. For a proper prosthesis to be fit, 5–7 cm of the humerus should be retained to ensure that adduction and abduction are preserved at the glenohumeral joint [12]. Maintaining maximal ROM at the shoulder post-amputation is predicated on keeping the insertions of the deltoid, pectoralis major, and latissimus dorsi intact. If the appropriate 5–7 cm of humerus is unable to be preserved, then a glenohumeral arthrodesis should be considered to prevent contracture [12]. While there are multiple prosthesis options for transhumeral amputations, hybrid models, which use body power for proximal movement and a myoelectric terminal device for distal extremity movement, tend to be preferred due to their improved myoelectric control with fewer electrodes [12]. Continued innovation and development of prosthesis technologies, such as osseointegration devices and targeted muscle reinnervation, can improve amputation outcomes [12].
This case report presents a 71-year-old female with rapidly progressive atraumatic left forearm pain, who was diagnosed with gas gangrene and was indicated for emergent I&D of the left upper extremity. She was found to have C. septicum bacteremia and was placed on appropriate antibiotics. Unfortunately, she lost neurologic function distal to the elbow joint and was later indicated for a proximal transhumeral amputation. Though she had a prolonged hospital stay, her clinical course stabilized and she was discharged to a rehabilitation facility. This case report highlights the importance of maintaining a high clinical suspicion and emergent treatment which ultimately led this patient to a positive outcome, survival, for such a deadly disease process.
Prompt surgical evaluation for C. septicum gas gangrene led to an overall positive outcome for this patient.
References
- 1.Larson CM, Bubrick MP, Jacobs DM, West MA. Malignancy, mortality, and medicosurgical management of Clostridium septicum infection. Surgery 1995;118:592-8. [Google Scholar | PubMed]
- 2.Schade VL, Roukis TS, Haque M. Clostridium septicum necrotizing fasciitis of the forefoot secondary to adenocarcinoma of the colon: Case report and review of the literature. J Foot Ankle Surg 2010;49:159.e1-8. [Google Scholar | PubMed]
- 3.Wiersema BM, Scheid KD, Psaradellis T. A rare trifocal presentation of Clostridium septicum myonecrosis. Orthopedics 2008;31:274. [Google Scholar | PubMed]
- 4.Chen LL, Tayban K, Caravanos C, Shaz D, Halpern NA. Necrotizing fasciitis associated with malignancy. J Am Assoc Nurse Pract 2020;32:109-12. [Google Scholar | PubMed]
- 5.Abella BS, Kuchinic P, Hiraoka T, Howes DS. Atraumatic clostridial myonecrosis: Case report and literature review. J Emerg Med 2003;24:401-5. [Google Scholar | PubMed]
- 6.Chipp E, Phillips C, Rubin P. Successful management of spontaneous Clostridium septicum myonecrosis. J Plast Reconstr Aesthet Surg 2009;62:e391-3. [Google Scholar | PubMed]
- 7.Forrester JD, Shkolyar E, Gregg D, Spain DA, Weiser TG. Nontraumatic Clostridium septicum myonecrosis in adults: Case report and a 15-year systematic literature review. Infect Dis Clin Pract 2016;24:318-23. [Google Scholar | PubMed]
- 8.Jessamy K, Ojevwe FO, Ubagharaji E, Sharma A, Anozie O, Gilman CA, et al. Clostridium septicum: An unusual link to a lower gastrointestinal bleed. Case Rep Gastroenterol 2016;10:489-93. [Google Scholar | PubMed]
- 9.Hermsen JL, Schurr MJ, Kudsk KA, Faucher LD. Phenotyping Clostridium septicum infection: A surgeon’s infectious disease. J Surg Res 2008;148:67-76. [Google Scholar | PubMed]
- 10.Gray KM, Padilla PL, Sparks B, Dziewulski P. Distant myonecrosis by atraumatic Clostridium septicum infection in a patient with metastatic breast cancer. IDCases 2020;20:e00784. [Google Scholar | PubMed]
- 11.Hechter S, Patel V, Bommu VJ, Patel P, Ao X, Alnabwani D, et al. Necrotizing fasciitis: A life-threatening infection due to Clostridium species. Cureus 2022;14:e22315. [Google Scholar | PubMed]
- 12.Fitzgibbons P, Medvedev G. Functional and clinical outcomes of upper extremity amputation. J Am Acad Orthop Surg 2015;23:751-60. [Google Scholar | PubMed]











