Wide excision of the Osteochondroma of the proximal femur combined with Total hip replacement with a REEF stem is a valid and reliable method to address both the tumor and symptoms caused by the resultant hip arthritis.
Dr. Raghul Siddharth, Department of Orthopedics, Sri Ramachandra Institute of Higher Education and Research, Porur, Chennai, Tamil Nadu, India. E-mail: raghulsiddharth@icloud.com
Introduction: Osteochondroma is a long bone benign tumor presenting at the metaphysis. Most of the occurrences are isolated lesions with very rare intra-articular extensions. Some occur as part of multiple hereditary exostoses. Isolated lesions are typically asymptomatic and diagnosed incidentally but, in some cases, present with bursa inflammation, pain, decreased range of motion and neurovascular deficit due to the mass effect of the tumor. Osteochondroma of the femur neck presents as an intra-articular pathology.
Case Report: A 41-year-old lady presented with right inguinal pain and swelling for 7 years, with an associated decreased range of movements of the right hip. Clinical examination revealed gross bony hard swelling, non-tender, and no local warmth. ROM was restricted, particularly internal rotation with additional abduction contracture and anterior joint line tenderness. A plain radiograph revealed a bony mass over metaphyseal-diaphyseal swelling over the medial aspect of the proximal femur with loss of femur head morphology and joint space narrowing. MRI confirmed the lesion as osteochondroma and a provisional diagnosis of Sessile solitary osteochondroma with probable sarcomatous with secondary degenerative osteoarthritis of the right hip was made. The patient underwent right total hip replacement with wide excision of the entire proximal femur using a REEF stem. The samples sent for histopathology confirmed the diagnosis as osteochondroma with no sarcomatous changes. Over a 10-year period of follow up, the patient showed no evidence of recurrence with improvement of hip movements assessed by Modified Harris Hip Score.
Conclusion: By planning and executing total hip replacement with REEF stem and wide excision of the tumor in a single sitting, both the progress of the tumor and the secondary degenerative arthritis were met with, in a single procedure.
Keywords: Osteochondroma, total hip replacement, chondrosarcoma, osteoarthritis.
Osteochondroma (OC) is defined as a hamartoma of the physeal cartilage, which grows and matures according to normal enchondral ossification with a male preponderance [1]. It is one of the most common benign tumors, accounting for more than one-third of all benign tumors. It occurs either as a solitary lesion or as hereditary multiple exostoses (HME), described as a hereditary neoplastic syndrome. The most common sites of occurrence are the metaphysis of long bones: Distal femur > proximal humerus > proximal tibia. The marrow space of the lesion is directly connected to that of the parent bone and ceases to grow on reaching skeletal maturity. The lesions are usually asymptomatic, and solitary lesions go undiagnosed. Still, they can cause pain, decreased range of motion, and other symptoms due to compression of adjacent neurovascular structures caused by the lesion’s mass effect. Usually, osteochondroma are extra-articular as they originate in the metaphysis, but osteochondroma of the femoral neck represent an intra-articular pathology [2].
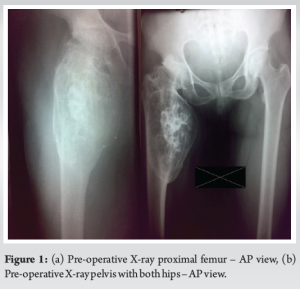
A 41-year-old lady presented to the OPD with complaints of swelling and progressive pain over the right inguinal region for the past 7 years. The swelling was initially small and gradually progressed to attain the present size. The swelling was associated with rest pain, and the pain was exacerbated during physical activity like walking or climbing stairs. No history of trauma to the region. There was no history of weight loss or loss of appetite. The patient was self-medicating with NSAIDs for pain relief. Clinical examination revealed a gross bony hard swelling over the right inguinal region. The swelling was non-tender. There were no sinuses or discharge. There was a restriction in the range of motion (ROM) at the hip joint with flexion of 20°, abduction was nil, internal rotation of 10°, external rotation of 20°, and extension of 10°. Further examination revealed an abduction contracture of 20° with anterior joint line tenderness. There were no similar swellings elsewhere in the body. The initial baseline investigations were within normal limits. The plain radiograph of the pelvis with both hip joints revealed a metaphyseal-diaphyseal swelling over the medial aspect of the right proximal femur adjacent to the lesser trochanter, with loss of sphericity of the femoral head, joint space narrowing, and osteophyte formation. The cortex appeared to be continuous with the femoral cortex, and the matrix was homogenous with patchy areas of mineralization (Fig. 1).
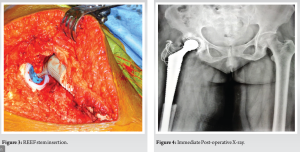
The magnetic resonance imaging (MRI) revealed an expansile lesion with no associated soft-tissue component. Pre-operative angiography was done to confirm perfusion of the deep branch of the medial femoral circumflex artery and to detect eventual alteration of its normal course cranial to the lesser trochanter and dorsal to the greater trochanter. The provisional diagnosis of sessile solitary osteochondroma with probable sarcomatous degeneration and secondary hip osteoarthritis (OA) was considered after radiographic evaluation. The patient was explained about the possibility of sarcomatous degeneration of the tumor, considering its longer duration of symptoms and the presence of rest pain. Under general anesthesia, the patient was placed in a left lateral position. Through the posterior approach, the proximal femur was exposed, retaining the short external rotators with a sleeve of cortical bone. The tumor was found to be involving the medial and posterior cortex of the proximal femur. The femoral head was dislocated posteriorly after performing a capsulotomy. Wide excision of the tumor by excision of the entire proximal femur was performed to remove the osseous base to avoid any chances of recurrence (Fig. 2). Diaphysis was reamed according to pre-operative templating. Serial reaming of the acetabulum was done, followed by the implantation of a cemented acetabular cup. A distally inter-locked modular Hydroxy apatite-coated femoral reconstruction prosthesis (REEFTM, Depuy) was used on the femoral side (Fig. 3). Intraoperative samples were sent for histopathological examination.

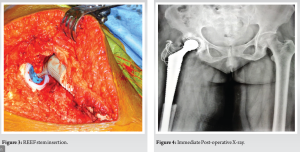
Histopathological examination: Sections showed a cartilaginous cap with underlying bone and areas of enchondral ossification. The cartilaginous cap was microscopically measured to be 2.2 mm mature hyaline cartilage overlying fibrous perichondrium. Bony trabeculae enclosing marrow noted trilineage hematopoiesis. No evidence of necrosis, pleomorphism, or sarcomatic changes was observed. The patient was mobilized with partial weight bearing for the initial 6 weeks, followed by full weight bearing mobilization. The patient has been under follow-up for the past 10 years, during which time she has exhibited good clinical outcomes. On follow-up radiographs, there were no signs of recurrence. The hip ROM was assessed with a Modified Harrison Hip Score (MMHS) and Visual Analog Score (VAS). MMHS improved from 35 at the 1st month follow-up to 60 at 1-year follow-up. At the 2-year follow-up, MMHS was 80. VAS improved from 4 at the first follow-up at 1 month to 0 at the on-year follow-up. The patient score was maintained for the subsequent follow-ups.
Siebenrock et al. in their series of cases of femoral neck osteochondroma, proposed the mechanism of development of OA in osteochondroma of femoral neck. Mechanical restriction of hip motion occurs by the direct contact of widened and enlarged femoral neck against the ischium and acetabular rim resulting in impingement leading to labral damage initiating OA. They used a versatile surgical approach that made the tumor’s visualization easy and allowed resection without endangering the deep branch of the medial circumflex femoral artery. They describe a posterolateral approach to the hip joint in which a trochanteric osteotomy is done and flipped anteriorly to visualize the capsule, followed by subluxation or dislocation of the femoral head to obtain a circumferential view of the neck [2]. Weiner et al. identified coxa valga and increased femoral anteversion in 25 patients with osteochondroma adjacent to the lesser trochanter, which they described as “Valgoversion.” They further theorized that involvement of the medial side of the femoral neck prevented the capital growth plate from aligning in a more vertical direction, with growth further exaggerating the valgus deformity. The lesser trochanter, being a traction epiphysis, contributes more to the shape of the medial and inferior base of the neck of the femur, and lesions in this region alter the shape, leading to valgoversion. The pre-operative radiograph in our patient also reveals altered proximal femur anatomy due to the presence of huge osteochondroma over the medial cortex [3]. Felix et al. describe a pediatric case of multiple hereditary exostoses with osteochondromata near the lesser trochanter, bilaterally with acetabular dysplasia. Acetabular dysplasia is less common and usually observed in cases with multiple hereditary exostoses. The child was treated with varus derotation osteotomy and pelvic osteotomy on both sides. The authors highlighted the importance of skeletal surveys in children with multiple hereditary exostoses to identify potential problems quickly [4]. Malignant transformation to a low-grade chondrosarcoma is a possibility in long-standing lesions. The incidence of sarcomatous degeneration is higher (36.3%) in patients with multiple exostoses when compared to patients with solitary osteochondroma. Ahmed et al. reported an incidence of sarcomatous degeneration in solitary osteochondroma of 7.6%. Malignant transformation is suspected when plain radiographs reveal irregularities in the tumor surface and inhomogeneous mineralization with areas of lucency and punctate calcifications. The permeative growth pattern was the clinching feature on histopathological examination to establish the diagnosis. There were no recurrences after wide excision, whereas recurrences were noted with marginal and intralesional excision [5]. Solitary osteochondroma of the proximal femur, which is symptomatic, is always treated surgically. In their series of six cases, Ramos-Pascual et al. report that marginal en bloc resection, including the osseous base of the tumor, provides excellent clinical results without recurrence. Our patient presented with symptomatic solitary osteochondroma along with hip OA. Considering the size and extent of the tumor, proximal femur resection retaining the attachment of short external rotators with a fragment of bone was planned along with joint arthroplasty to address the OA [6]. Hammad et al. published a case report where a 28-year-old male who had right-side gluteal pain and decreased hip movement. According to the report, the patient improved significantly after a 4-month follow-up. They asserted that femoral neck osteochondroma leads to mechanical block and pain. Hammad et al. explained about excising femur neck osteochondroma and fixing the femur neck prophylactically with cannulated cancellous screws. There were no recurrences, and with a 4-month follow-up, there was a significant improvement in hip ROM [7]. The use of hydroxyapatite-coated long stem has been key in treating this case. Mcauley et al. asserted that the local delivery system of hydroxyapatite helps in lesser proximal femur bone resorption with a density increase in the distal part of the femur, particularly in the anatomical medullary locking hip implant [8]. Rosenthall et al. demonstrated that hydroxyapatite significantly reduced mineral loss in Gruen zones 1 and 7 which surround porous coating [9]. These facts supported our decision to use a REEF stem, a modular hydroxyapatite-coated distally interlocked femoral component. Mesfin et al. reported a 61-year-old man with severe hip pain. Radiographs revealed large irregular osteochondroma in the left proximal femur. Examination revealed restriction of hip range of movements. The choice of implant is dictated by proximal femur deformity. He underwent total hip arthroplasty (THA) with uncemented modular femoral component due to widened metaphysis a fully coated system (VerSys Beaded full coat Zimmer that engaged diaphysis). A 27-month follow-up revealed pain relief and improved functionality [10]. As reconstruction requirements are best determined intraoperatively, a modular option helps in femoral component assembly. Moran et al. reported two cases where hip dysplasia due to HME progressed to symptomatic hip OA. They were treated with surgical excision and THA. The acetabular component was an uncemented hydroxyapatite-coated hemispherical ABG, or Trident shell (Stryker) that was implanted with screw augmentation. The proximal femur was reconstructed with GMRS, Stryker) with trochanteric claw (if trochanter is present) and cerclage cable. They asserted that THA is a valid option with HME of proximal femur with advanced OA while maintaining the concerns of using a proximal femur stem [11]. Kim et al. reported a 57-year-old female diagnosed with HME with severe right hip pain gradually progressing to difficulty in walking with a severe hip range of movements restriction and a limb length discrepancy of 2.4 cm (right longer than left). She underwent THA (cement-less Wagner cone prosthesis) of the right hip along with an all bone graft. A 2-year follow-up revealed improvement in Harris’s hip score apart from the immediate pain relief and improved functionality (Fig. 4). They asserted that the expansion of proximal femur metaphysis with exostoses of the medial aspect is closer to the neurovascular structures and requires adequate pre-operative planning and careful consideration of the choice of implant [12] (Fig. 5).

As evidenced by the review of the literature, it is safe to conclude how rare the osteochondroma presents over the neck of the femur, making it an intra-articular pathology leading to OA. This requires a detailed and meticulous evaluation and pre-operative workup to account for the choice of implant, the surgical approach, and limb length discrepancy (if any). This case report shows how the osteochondroma lesion and the inevitable resultant arthritis can be tackled through a single procedure. The follow-up reviews showed considerable improvement with no recurrence restrictions in daily activities.
The total hip replacement with the long REEF stem is a step in helping the patient achieve functionality comparable to that before the onset of the OC with secondary OA, relieving both pain and improved hip ROM, thereby improving the quality of life.
References
- 1.Campanacci M, Campanacci M. Bone and Soft Tissue Tumors: Clinical Features, Imaging, Pathology and Treatment. 2nd ed. Padova: Piccin Nuova Libraria; 1999. [Google Scholar]
- 2.Siebenrock KA, Ganz R. Osteochondroma of the femoral neck. Clin Orthop Relat Res 2002;394:211-8. [Google Scholar]
- 3.Weiner DS, Hoyt WA Jr. The development of the upper end of the femur in multiple hereditary exostosis. Clin Orthop Relat Res 1978;137:187-90. [Google Scholar]
- 4.Felix NA, Mazur JM, Loveless EA. Acetabular dysplasia associated with hereditary multiple exostoses: A case report. J Bone Joint Surg Br 2000;82:555-7. [Google Scholar]
- 5.Ahmed AR, Tan TS, Unni KK, Collins MS, Wenger DE, Sim FH. Secondary chondrosarcoma in osteochondroma: Report of 107 patients. Clin Orthop Relat Res 2003;411:193-206. [Google Scholar]
- 6.Ramos-Pascua LR, Sánchez-Herráez S, Alonso-Barrio JA, Alonso-León A. Solitary proximal end of femur osteochondroma: An indication and result of the en bloc resection without hip luxation. Rev Esp Cir Ortop Traumatol (Engl Ed) 2012;56:24-31. [Google Scholar]
- 7.Hammad Y, Saleh HA, Aburumman IF, Balasim M, Al-Hyari MI, Al-Ajlouni J. A rare case of intra-articular osteochondroma of the femoral neck: A case report. J Orthop Case Rep 2021;11:91-6. [Google Scholar]
- 8.McAuley JP, Sychterz CJ, Engh CA Sr. Influence of porous coating level on proximal femoral remodeling: A postmortem analysis. Clin Orthop Relat Res 2000;371:146-53. [Google Scholar]
- 9.Rosenthall L, Bobyn JD, Tanzer M. Bone densitometry: Influence of prosthetic design and hydroxyapatite coating on regional adaptive bone remodelling. Int Orthop 1999;23:325-9. [Google Scholar]
- 10.Mesfin A, Goddard MS, Tuakli-Wosornu YA, Khanuja HS. Total hip and knee arthroplasty in patients with hereditary multiple exostoses. Orthopedics 2012;35:e1807-10. [Google Scholar]
- 11.Moran M, Krieg AH, Boyle RA, Stalley PD. Bilateral total hip arthroplasty in severe hereditary multiple exostosis: A report of two cases. Hip Int 2009;19:279-82. [Google Scholar]
- 12.Kim WJ, Park JS, Won SH, Lee HS, Lee DW, Jang BW, et al. Total hip arthroplasty in hereditary multiple exostoses with secondary osteoarthritis: A case report. Medicine (Baltimore) 2019;98:e18175. [Google Scholar]