Chronic localized dull-aching bony pain without any systemic illness needs urgent evaluation with X-ray and MRI for definitive diagnosis of Brodie’s abscess and may be successfully treated with thorough debridement and filling of bony void with antibiotic-impregnated calcium sulfate (AICS) beads.
Dr. Mridul Biswas, Department of Orthopaedic Surgery, AIIMS Kalyani, Kalyani, West Bengal, India. E-mail: drmbcmc@gmail.com
Introduction: Brodie’s abscess is one type of subacute osteomyelitis without any sequestrum or any systemic illness. Thorough debridement and removal of sclerotic rim are the mainstay of the treatment. Antibiotic-impregnated calcium sulfate (AICS) beads act as osteoconductive and at the same time, it maintains high antibiotic concentration locally.
Case Report: Three cases are presented with unusual sites of Brodie’s abscess without any history of injury, puncture wound, swelling, or fever. All the patients were presented with dull-aching localized deep bony pain. With X-ray and magnetic resonance imaging (MRI) typical findings, it was diagnosed as Brodie’s abscess. All patients went through surgical procedure and AICS beads insertion inside the bony cavity. All the patients were cured of the disease without any discharge or recurrence of pain with well consolidation of the bony void.
Conclusion: In chronic localized bony dull-aching pain with normal blood parameters without any systemic illness, investigations such as X-ray and MRI should be done. Meticulous surgical debridement and AICS beads insertion without bone graft may be considered as definitive treatment of Brodie’s abscess.
Keywords: Brodie’s abscess, chronic osteomyelitis, antibiotic-impregnated calcium sulfate, calcium sulfate.
Brodie’s abscess is a type of subacute osteomyelitis that has pus or granulation tissue-filled cavity with no sequestra [1]. Sir Benjamin Brodie first described the disease in 1832 [2]. Atraumatic chronic pain to a localized area of the limb without any systemic illness is the characteristic presentation in Brodie’s abscess. The mainstay of managing Brodie’s abscess is surgery, which consists of thorough debridement of the lesions and removal of the peripheral sclerotic rim of bone. Antibiotic-impregnated calcium sulfate (AICS) beads have the properties such as biocompatible, biodegradable, osteoconductive, and elution of 100% antibiotic in a controlled manner and can be used successfully in osteomyelitis [3]. In our cases, we have filled the post-debridement bony cavity with AICS, which acted like a filler along with the local antibiotic delivery system that might have helped for early consolidation of the cavity for its osteoconductive property. Brodie’s abscess should be differentiated from osteoid osteoma, eosinophilic granuloma/Langerhans cell histiocytosis, chondrosarcoma, and tuberculosis, as the similar type of symptoms and age of onset correlate with each other [4-8]. Detailed clinical examination, preoperative radiological investigations, and intraoperative tissue samples for histopathology and culture sensitivity may help to rule out the other differentials, to get a proper diagnosis, and to achieve better clinical outcomes. This case series aims to describe the unusual locations of abscesses, clinical features, diagnosis, and treatment outcomes with AICS beads.
Case 1
A 35-year-old female presented with mild pain over her right leg for the past 4 years and was getting aggravated after walking. There was no history of trauma, fever, or any open or penetrating injury. The patient was primarily treated with analgesics. There was deep tenderness over the medial aspect of the distal part of the right leg with an intact range of movement of the ankle without any associated neurovascular deficit. Blood parameters such as erythrocyte sedimentation rate, C-reactive protein (CRP), and complete blood count (CBC) were within the normal limits (Fig. 1-5).
A full-length radiograph of the right leg AP and lateral view was obtained, which showed an oval to serpentine-shaped lucency with a well-circumscribed sclerotic margin in the distal tibial metaphysis. Magnetic resonance imaging (MRI) shows features suggestive of Brodie’s abscess, like penumbra sign. As the size of the lesion is small (<3 cm) and the typical findings of X-ray and MRI which suggestive of brodie’s abscess, we have planned for excisional biopsy rather than core biopsy/Tru-cut biopsy. Debridement, curettage of the lesion, complete removal of the peripheral sclerotic rim till getting bleeding metaphyseal bone, and filling of the void with vancomycin and gentamicin-mixed calcium sulfate beads were done. No autogenic bone graft was used. The specimen was sent for culture sensitivity and histopathological examination. Post-operative immobilization was done with a below-knee back slab for 6 weeks. The patient was given intravenous antibiotic for 2 weeks. CBC and CRP were regularly checked. Culture sensitivity report came as no growth of organism. Histopathological features suggested chronic osteomyelitis. The patient was then discharged after 2 weeks of post-operative with oral clindamycin (300 mg tds) for 4 weeks. She was allowed for a range of movement exercises and toe touch weight bearing after the removal of slab for the next 4 weeks. Follow-up X-rays were done at 3 months, 6 months, 9 months, and at 1 year. At the end of 3 months, there was complete resorption of the AICS beads. At the end of 9 months, the bony cavity was completely ossified. There was no wound healing problem or residual pain at 1 year of follow-up.
Case 2
A 25-year-old male presented with dull-aching pain over the left distal thigh for the last 5 years, having no history of trauma, open injury, or fever. He had no systemic illness. The patient was taking analgesics as and when required (Fig. 6-9).
On clinical examination, no abnormality was detected except local tenderness. After doing an X-ray, MRI, and blood investigation, the patient was planned for debridement, curettage, and filling the void with antibiotic (vancomycin + gentamicin)-mixed calcium sulfate beads. Curettage was done by a window made through the medial cortex of the distal femur. Intraoperative, the lesion was found to have a sclerotic margin filled with cherry-colored tissue which was sent for culture sensitivity, Gram’s stain, Ziehl–Neelsen stain, cartridge-based nucleic acid amplification test, and histopathological examination. The sclerotic margin was removed till the metaphyseal bleeding bone was reached, and the post-debridement void was filled with 10 cc of AICS. As the typical features in X-ray and MRI suggested Brodie’s abscess and because of small size of the lesion, we had planned for excisional biopsy and culture of the lesion for definitive diagnosis of the lesion. Like the previous case, here also, no organism was detected in culture sensitivity. Histopathology showed the presence of granulation tissue without the presence of any giant cell or metaplasia suggestive of chronic osteomyelitis. The patient was allowed partial weight bearing for 6 weeks and after 2 weeks of intravenous antibiotics, the patient was discharged with oral clindamycin for 4 weeks.
Case 3
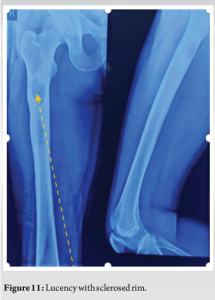
A 31-year-old male presented with right proximal thigh pain for the past 8 years. The pain was getting aggravated after the activity. No history of trauma, swelling, sinus, or fever was present. The patient’s X-ray and MRI revealed a well-circumscribed sclerotic margin with a fluid-filled cavity at the posteromedial cortex of the metaphyseal-diaphyseal junction of the proximal femur suggestive of Brodie’s abscess (Fig. 10-12).

The patient was then treated with debridement, curettage, intramedullary reaming, antibiotic-mixed calcium sulfate beads insertion into the intramedullary canal and intramuscularly in and around the lytic lesion. Prophylactic long proximal femoral nail was inserted. The patient was allowed to ambulate with full weight bearing in the post-operative period. Intra-operative debridement tissue’s Gram’s stain came negative, but the culture sensitivity test showed methicillin-sensitive Staphylococcus aureus (MSSA), which was sensitive to vancomycin, gentamicin, clindamycin, and linezolid. The patient was treated for 2 weeks with intravenous vancomycin and then discharged with oral linezolid and clindamycin for 4 weeks. All the patients’ follow-ups were regularly taken at 6 weeks, 3 months, 6 months, 9 months, and 1 year. All final X-rays showed consolidation of void. No complaints were present regarding pain, discharge, or fever.
Brodie’s abscess is primarily found in young men [9]. It is a hematogenous osteomyelitis, with minimal localized symptoms such as mild swelling, abscess, impetigo, or blisters [10,11]. All of our cases are in the age group of 20–40 years, and none of them had any previous history of trauma, fever, or local discharging sinus. All of them presented with localized pain in the affected body part without any systemic manifestations. In general, in microbiological study, no organism is found in 20–50% of cases [12,13]. The most common bacteria causing Brodie’s abscess are S. aureus. In our series, we had only one case, whose culture and sensitivity of the tissue samples from the cavity reported the growth of MSSA. Histopathology of the tissue samples sent from the lesion showed chronic osteomyelitis with granulation, including lymphocytes and plasma cells in all cases without granuloma or metaplasia. With very few or no constitutional symptoms and almost normal blood parameters, Brodie’s abscess is difficult to diagnose in the first place. Furthermore, it mimics some benign or malignant bone tumors. However, some characteristic radiological features such as serpentine sign on X-ray and the penumbra sign on MRI help in the diagnosis of the disease [9,10]. The early and correct diagnosis of Brodie’s abscess leads to a 100% cure rate [9]. Treatment is mainly surgical, which includes thorough debridement and curettage of the lesion. Only antibiotic treatment has a high recurrence rate and the length of antibiotic treatment is not defined [11]. The most crucial factor for successful treatment of Brodie’s abscess is removing all around the sclerotic rim of bone at the periphery of the lesion and getting a healthy bleeding cavity wall. Management of the post-debridement bony void is also vital, as the hematoma formed in the void may serve as a safe nidus for the growth and proliferation of the organism. Different options to fill the void are bone graft, polymethyl methacrylate, calcium sulfate, calcium phosphate, or bioactive glass [14]. All the options have their advantages and disadvantages. From the recent literature, it is clear that AICS has a lower recurrence of infection rate than PMMA [3]. AICS beads get dissolved fully to deliver 100% antibiotic locally for an extended period of around 6–8 weeks [3]. The concentration of local antibiotic is much higher than the minimum inhibitory concentration of the particular bacteria. Furthermore, antibiotics have low systemic toxicity, as they are used locally. In AICS, heat-sensitive antibiotics can be used, as AICS beads are made at cool room temperature in a non-exothermic process [15]. Furthermore, the second surgery is not required to remove the beads [16]. In our study, we filled the post-debridement bony cavity with AICS beads, which acted like the local antibiotic delivery system and its osteoconductive property, which has helped in the early consolidation of the bony cavity. There was no recurrence of infection, no delayed wound healing, or discharge from the surgical site. We also did not encounter any problem related to heterotrophic ossification or hypercalcemia. Vancomycin and gentamycin-mixed beads were used in this study, which have comparable results with the study by Ferguson et al. [17] and McNally et al. [18]. AICS beads promote new bone formation because of osteoconductive property. AICS also induces vascularized membrane and corticalization which promotes bone formation [19]. It does not induce any inflammatory cells in the bone regeneration processes. It is a reasonable alternative to autogenous bone graft in bone defects with infection to fill the dead space or bony void [20].
This study shows that chronic mild, dull-aching pain in a limb with deep localized tenderness without systemic illness should be evaluated with diagnostic tools such as X-ray and MRI. Meticulous surgical debridement and filling the void with AICS beads without any bone graft can be considered a definitive treatment for Brodie’s abscess.
Long-standing dull-aching bone pain without any systemic illness should be evaluated urgently with X-ray and MRI. Brodie’s abscess can be successfully treated with thorough debridement and AICS bead insertion without any recurrence.
References
- 1.Harris NH, Kirkaldy WH. Primary subacute pyogenic osteomyelitis. J Bone Joint Surg Br 1965;47:526-32. [Google Scholar]
- 2.Brodie BC. An account of some cases of chronic abscess of the tibia. Med Chir Trans 1832;17:239-49. [Google Scholar]
- 3.Thahir A, Lim JA, West C, Krkovic M. The use of calcium sulphate beads in the management of osteomyelitis of femur and tibia: A systematic review. Arch Bone Jt Surg 2022;10:320-7. [Google Scholar]
- 4.Schlur C, Bachy M, Wajfisz A, Ducou le Pointe H, Josset P, Vialle R. Osteoid osteoma mimicking Brodie’s abscess in a 13-year-old girl. Pediatr Int 2013;55:e29-31. [Google Scholar]
- 5.Chang WF, Hsu YC, Wu YD, Kuo CL, Huang GS. Localized Langerhans cell histiocytosis masquerading as Brodie’s abscess in a 2-year-old child: A case report. EXCLI J 2016;15:33-7. [Google Scholar]
- 6.Datir A, Lidder S, Pollock R, Tirabosco R, Saifuddin A. High-grade chondrosarcoma mimicking Brodie’s abscess. Clin Radiol 2009;64:944-7. [Google Scholar]
- 7.Siddiqui MS, Javed S, Razak A, Zubairy A, Khan SH. Brodie’s abscess with tuberculous osteomyelitis of the foot. JBR BTR 2014;97:168-9. [Google Scholar]
- 8.Yoshikawa M, Sugawara Y, Kikuchi T, Nakata S, Mochizuki T, Ikezoe J, et al. Two cases of pediatric bone disease (eosinophilic granuloma and Brodie’s abscess) showing similar scintigraphic and radiographic findings. Clin Nucl Med 2000;25:986-90. [Google Scholar]
- 9.Kornaat PR, Camerlinck M, Vanhoenacker FM, De Praeter G, Kroon HM. Brodie’s abscess revisited. JBR BTR 2010;93:81-6. [Google Scholar]
- 10.Wright WF. “Penumbra sign” of Brodie’s abscess. Braz J Infect Dis 2020;24:264-5. [Google Scholar]
- 11.van der Naald N, Smeeing DP, Houwert RM, Hietbrink F, Govaert GA, van der Velde D. Brodie’s abscess: A systematic review of reported cases. J Bone Jt Infect 2019;4:33-9. [Google Scholar]
- 12.Vishwakarma N, Chauhan S, Binyala SS, Singh SK. Brodie’s abscess of the proximal humerus metaphysis: A case report. J Orthop Case Rep 2021;11:38-42. [Google Scholar]
- 13.Shih HN, Shih LY, Wong YC. Diagnosis and treatment of subacute osteomyelitis. J Trauma 2005;58:83-7. [Google Scholar]
- 14.Ferrando A, Part J, Baeza J. Treatment of cavitary bone defects in chronic osteomyelitis: Biogactive glass S53P4 vs. Calcium sulphate antibiotic beads. J Bone Jt Infect 2017;2:194-201. [Google Scholar]
- 15.Wahl P, Guidi M, Benninger E, Rönn K, Gautier E, Buclin T, et al. The levels of vancomycin in the blood and the wound after the local treatment of bone and soft-tissue infection with antibiotic-loaded calcium sulphate as carrier material. Bone Joint J 2017;99-B:1537-44. [Google Scholar]
- 16.Mereddy P, Nallamilli SR, Gowda VP, Kasha S, Godey SK, Nallamilli RR, et al. The use of Stimulan in bone and joint infections. Bone Jt Open 2023;4:516-22. [Google Scholar]
- 17.Ferguson JY, Dudareva M, Riley ND, Stubbs D, Atkins BL, McNally MA. The use of a biodegradable antibiotic-loaded calcium sulphate carrier containing tobramycin for the treatment of chronic osteomyelitis: A series of 195 cases. Bone Joint J 2014;96-B:829-36. [Google Scholar]
- 18.McNally MA, Ferguson JY, Lau AC, Diefenbeck M, Scarborough M, Ramsden AJ, et al. Single-stage treatment of chronic osteomyelitis with a new absorbable, gentamicin-loaded, calcium sulphate/hydroxyapatite biocomposite: A prospective series of 100 cases. Bone Joint J 2016;98-B:1289-96. [Google Scholar]
- 19.Ma YF, Jiang N, Zhang X, Qin CH, Wang L, Hu YJ, et al. Calcium sulfate induced versus PMMA-induced membrane in a critical-sized femoral defect in a rat model. Sci Rep 2018;8:637. [Google Scholar]
- 20.Orsini G, Ricci J, Scarano A, Pecora G, Petrone G, Iezzi G, et al. Bone-defect healing with calcium-sulfate particles and cement: An experimental study in rabbit. J Biomed Mater Res B Appl Biomater 2004;68:199-208. [Google Scholar]