Charcot’s arthropathy of the wrist though rare and a diagnosis of exclusion should always be suspected in painless arthropathy of the wrist.
Dr. Sai Krishna M L V, Consultant, Department of Orthopaedics, Aayush Hospitals, Eluru, India. E-mail: krishna.mlv.sai@gmail.com
Introduction: Charcot arthropathy is a myriad of osseous degenerative changes that can affect theoretically any joint of the body. The pathophysiology of this condition is based on microtrauma, leading to the deterioration of articular nerves. The most common cause in the upper extremity is syringomyelia.
Case Report: A 64-year-old male patient presented with painless right wrist swelling and deformity. His radiographs showed degenerative changes in radiocarpal and intercarpal joints. Magnetic resonance imaging of the brain and cervical spine demonstrated Type II Chiari malformation and syringomyelia, and neurological evaluation revealed myelopathy.
Conclusion: Charcot arthropathy of the wrist, an exceedingly rare condition, is a diagnosis of exclusion. The common causes of arthritis of the wrist such as Rheumatoid arthritis and tuberculosis must be ruled out. When a patient presents with wrist Charcot arthropathy thorough neurological examination must be done. Diabetes mellitus, tabes dorsalis, and leprosy are the other frequently cited causes that must be looked for.
Keywords: Charcot arthropathy, wrist, syringomyelia.
Charcot’s joint arthropathy is often misdiagnosed pathology commonly affecting major weight-bearing joints. Mitchell et al. in 1831 described the first Charcot’s arthropathy, later Jean Marie Charcot described the clinical features in patients with tabes dorsalis. Jordan et al. demonstrated diabetic peripheral neuropathy as one of the etiology for Charcot’s joint [1,2]. Apart from diabetic peripheral neuropathy, the other common causes include syringomyelia and tabes dorsalis, hereditary sensory motor neuropathy, leprosy, peripheral nerve injuries or spinal cord injuries, spinal dysraphism, congenital insensitivity to pain, and multiple sclerosis. The other rare causes include alcoholism, pernicious anemia, amyloidosis, familial dysautonomia, and congenital thalidomide syndrome [3,4]. The most acceptable theories of pathogenesis are neurotraumatic and neurovascular theories [5]. The hallmarks of Charcot’s joint are painless joint swelling and deformity with local signs of inflammation. Because of painless deformity, the diagnosis is often delayed, which might lead to repetitive microtrauma that proceeds to joint destruction, later to ulceration and superadded infection [5]. Upper extremity joint involvement is exceedingly rare to encounter in clinical practice. In this case report, we present a patient who developed Charcot’s wrist arthropathy due to syringomyelia.
A 64-year-old male patient presented to our hand unit with complaints of progressive painless right wrist swelling and deformity (Fig. 1). The patient reported that the deformity has developed gradually over the past 2 years and denied any previous history of infection or trauma. He had discomfort and pain in the neck and shoulder with a restricted neck range of motion over the last 3 years. He also noted a gradual loss of hand dexterity. On clinical examination, he had diminished sensation of pain and temperature bilaterally in the upper and lower extremities in all dermatomes. The patient had demonstrated reduced strength in all major muscle groups in the bilateral upper and lower extremities along with hyperreflexia bilaterally in the upper and lower extremities. Inverted radial reflex and positive Hoffman sign were elicited. The Babinski test result was neutral (mute). He had a broad-based gait but denied the use of a walker for doing regular household activities. The patient’s past medical history included dyslipidemia and hypertension. He stated no known history of sexually transmitted infection, diabetes mellitus, stroke, rheumatoid arthritis, or any other autoimmune arthropathy. He was managed conservatively with a wrist splint, Philadelphia collar, and physical therapy under regular follow-up. He was lost to follow-up for 18 months because of the COVID-19 pandemic. During that period, he presented to a local hospital for right wrist deformity and swelling and underwent a right wrist synovial biopsy. The report of histopathological examination showed synovial hyperplasia with occasional giant cells. He was started on antitubercular medication for the same which he discontinued after 4 months. He noted that since the onset, the deformity had gradually increased despite a trial of anti-tubercular medication, non-steroidal anti-inflammatory medication, and activity modification. Examination revealed an obvious swelling and deformity of the right wrist (Fig. 1). The carpus appeared to be translated dorsal and ulnar to the distal radius. The skin over the wrist was normal but with no signs of inflammation. There was a painless motion of the wrist in flexion, extension, and radial and ulnar deviation with restriction of the terminal range of motion. There was palpable crepitus in all directions.
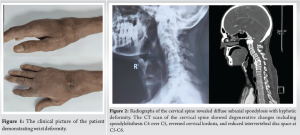
The patient’s total leucocyte counts were within normal limits. The patient’s renal and liver function tests were within normal limits. The patient’s erythrocyte sedimentation rate (ESR) was 18 mm/hr, C-reactive protein (CRP) was 1.0 mg/L, and his serum procalcitonin was 0.4 ng/mL. His HbA1c was 6.0, rheumatoid factor (RF), and anti-CCP test results were negative. On the cervical spine radiograph and CT, there were degenerative changes with kyphosis and spondylolisthesis of C4 over C5 and decreased disc space at C5-C6 (Fig. 2), and an MRI was done which was suggestive of Chiari malformation with the extension of syrinx from C2 to D2 (Fig. 3).

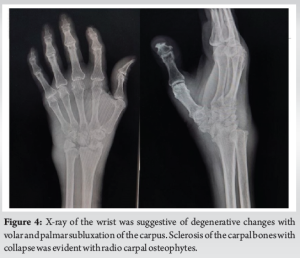
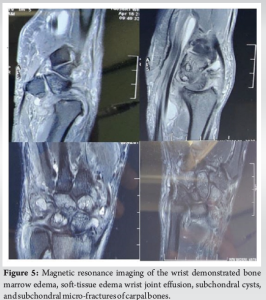
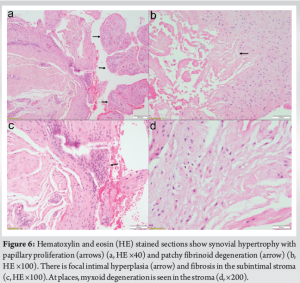
Radiographs of the wrist showed sclerosis and collapse of carpal bones with fragmentation with advanced destructive changes in the radiocarpal and intercarpal joints (Fig. 4 and 5). Histopathological workup demonstrated synovial hypertrophy and fibrinogen degeneration with the absence of plasma cell deposition or bone necrosis. Synovial biopsy for ZN staining, GENE XPERT, and PCR for mycobacterium tuberculosis were negative. The case was discussed in a radio conference with the orthopedic teaching staff at our institution. The most common etiologies (tuberculosis and rheumatoid arthritis) were inconsistent with the typical presentation of painless joint destruction. As per the advice from the rheumatology and radiology departments, we performed a wrist synovial biopsy under local anesthesia. Histopathological examination demonstrated features suggestive of Charcot arthropathy and ruled out the possibility of osteomyelitis or tuberculosis (Fig. 6). Synovial biopsy specimens were subjected to ZN staining for acid-fast bacilli, GENE XPERT, and PCR for Mycobacterium tuberculosis. The test results were negative for tuberculosis. The markers suggestive of a seropositive joint arthropathy (rheumatoid factor and anti-CCP) were negative and the inflammatory workup for septic arthropathy and osteomyelitis was negative. According to the neurological examination and the presence of syrinx in the subaxial spine, the most likely etiology was syringomyelia.
The patient had painless restriction of active range of motion with loss of fine grasp. His upper extremity and hand functions were not severely restricted. There was a minimal functional limitation of the wrist joint. There were no symptoms of carpal tunnel syndrome. His wrist deformity was treated with a removable wrist splint and functional therapy. Wrist radiographs demonstrate osseous lesions of stage 2 Eichenholtz. We deferred the surgical intervention at the present clinical-radiological stage due to the risk of progression of joint destruction. During the last 6-month follow-up period, the patient had a progression of his myelopathy symptoms. He was later referred to neurosurgery and was advised to undergo foremen magnum decompression with or without cervical fixation, and the patient was counseled for the same. The management of cervical myelopathy as the primary etiology in our case might delay the further progression of joint destruction. The symptoms of the wrist were stable at present with one recent episode of trivial trauma that led to pain and aggravation of swelling. Swelling and pain were subsided with NSAIDs, physical therapy, and a wrist splint. We explained the poor prognosis to the patient, the possibility of progressive degenerative wrist arthropathy, and the need for wrist fusion at a later date. The patient was kept under regular follow-up at 3 monthly intervals for monitoring of functional scores and radiological progression of disease (stage 3 Eichenholtz).
Charcot’s arthropathy of the wrist is frequently caused by syringomyelia rather than diabetes mellitus. Very few case reports of Charcot’s arthropathy in non-weight-bearing joints have been described in the current literature. Although rare, Charcot’s wrist arthropathy is a potential cause of functional disability. Jackson et al. [6] described a case report of right wrist Charcot’s in a patient, in his early 70s, with cervical spondylotic myelopathy which was managed non-surgically. Worster et al. [7] presented a patient with bilateral wrist Charcot’s due to cervical tabes dorsalis. Deng et al. [8] presented a series of 12 patients with Charcot’s arthropathy of the upper extremity. MRI showed syrinx in all patients with Chiari malformation and tethered spinal cord. They postulated that the elbow followed by the shoulder was most involved in syringomyelia. The patients who underwent a neurosurgical procedure had improvement in their neurological dysfunction with no further deterioration of joint destruction. Our patient also the cause for Charcot’s arthropathy was syringomyelia and only the wrist joint on the side was affected. Parker et al. [9] presented a patient in which both lower limbs were involved sequentially followed by upper limbs in a patient with congenital insensitivity to pain. Following above knee amputation for both lower limbs, the patient started using the upper extremity for load bearing, which led to joint destruction. Wrobel et al. [10] presented a patient with wrist Charcot’s arthropathy post-diabetic peripheral neuropathy. Nagano et al. [11] have published their radiological screening study on wrist joint arthropathy in patients with long-standing peripheral nerve palsy due to Leprosy. Patel et al. [12] have published a case of poly articular Charcot’s arthropathy of the upper limb including the small joints of the wrist, elbow, and bilateral shoulder in a patient with a syrinx and Chiari malformation. Caglayan et al. [13] have reported a case of a diabetic female patient, in her late 50s, with acute Charcot arthropathy of the wrist which was misdiagnosed as complex regional pain syndrome earlier. Non-surgical management was advised with an off-loading brace and good glycemic control. Parker et al. [9] reported a case subtype of congenital indifference to pain in which the patient originally developed poly articular Charcot arthropathy of bilateral lower limbs necessitating bilateral above-knee amputation. Later because of the usage of the upper extremities for mobilization, the patient ultimately developed Charcot’s arthropathy of bilateral wrist and hand. Xu et al. [14] have described a case of misdiagnosed wrist Charcot’s arthropathy as synovitis and radiocarpal arthritis. The patient was initially managed by performing a synovectomy and four-corner arthrodesis to decrease the symptoms and preservation of function. The patient presented with gross inflammation of the wrist about 2 months after the surgery. Later, a cervical MRI was done to evaluate the cause of allodynia which revealed syringomyelia with Chiari malformation. The wrist joint fused spontaneously over 2 months with conservative management. They proposed that due to wrong diagnosis and mismanagement of Charcot’s arthropathy in stage 2 Eichenholtz with incomplete fusion ultimately resulted in aggravation of joint destruction and the early total fusion of the joint compromising the residual joint mobility. In our patient, as the wrist joint is painless and there was progressive myelopathy in the cervical spine, he was planned for initial surgical management of the cervical spine and conservative treatment for wrist deformity with functional therapy and a wrist splint. There was no specific pharmacological management to prevent joint destruction. Non-surgical management is preferred in the initial stages of the disease (Eichenholtz stages 1 and 2). The most essential step is offloading the affected joint to delay the progression and management of the underlying etiology. Surgical management is reserved for advanced (Eichenholtz stage 3) and resistant cases with instability in the form of fusion.
Charcot arthropathy of the wrist, an exceedingly rare condition, is a diagnosis of exclusion. The common causes of arthritis of the wrist such as rheumatoid arthritis and tuberculosis must be ruled out. When a patient presents with wrist Charcot arthropathy thorough neurological examination must be done. Diabetes mellitus, tabes dorsalis, and leprosy are the other frequently cited causes that must be looked for. In our patient, it was found to be due to syringomyelia.
Charcot’s arthropathy of the wrist though rare and a diagnosis of exclusion should always be suspected in painless arthropathy of the wrist.
References
- 1.Shah MK, Hugghins SY. Charcot’s joint: An overlooked diagnosis. J La State Med Soc 2002;154:246-50. [Google Scholar | PubMed]
- 2.Pinzur MS. Charcot’s foot. Foot Ankle Clin 2000;5:897-912. [Google Scholar | PubMed]
- 3.Christensen TM, Yderstraede K, Ejskjaer N, Jakobsen PE, Kjaer IL, Levin S, et al. Den diabetiske Charcots fod (Charcot’s arthropathy). Ugeskr Laeger 2008;170:2440-5. [Google Scholar | PubMed]
- 4.Farsetti P, Caterini R. Idiopathic Charcot’s arthropathy. Report of one case. Arch Orthop Trauma Surg 1992;111:282-3. [Google Scholar | PubMed]
- 5.Bayne O, Lu EJ. Diabetic Charcot’s arthropathy of the wrist. Case report and literature review. Clin Orthop Relat Res 1998;357:122-6. [Google Scholar | PubMed]
- 6.Jackson K, Ramadorai U, Abell B, Devine J. Charcot arthropathy of the wrist associated with cervical spondylotic myelopathy. Global Spine J 2012;2:227-30. [Google Scholar | PubMed]
- 7.Worster-Drought C. Charcot’s arthropathy of wrists. Proc R Soc Med 1927;20:192. [Google Scholar | PubMed]
- 8.Deng X, Wu L, Yang C, Xu Y. Neuropathic arthropathy caused by syringomyelia. Neurosurg Spine 2013;18:303-9. [Google Scholar | PubMed]
- 9.Parker RD, Froimson AI. Neurogenic arthropathy of the hand and wrist. J Hand Surg 1986;11:706-10. [Google Scholar | PubMed]
- 10.Wrobel M, Szymborska-Kajanek A, Skiba M, Karasek D, Górska J, Wittek A, et al. Charcot’s joint of the wrist in type 2 diabetes mellitus. Exp Clin Endocrinol Diabetes 2007;115:55-7. [Google Scholar | PubMed]
- 11.Nagano J, Tada K, Masatomi T, Horibe S. Arthropathy of the wrist in leprosy--What changes are caused by long-standing peripheral nerve palsy. Arch Orthop Trauma Surg 1989;108:210-17. [Google Scholar | PubMed]
- 12.Patel JH, Chaturvedi V, Bhandari GS, Gupta M. Polyarticular Charcot: A rare case report and a literature review in Indian context. J Clin Rhematol Immunol 2020; 8:R1. [Google Scholar | PubMed]
- 13.Çaglayan G, Kilic E, Ozcakar L. Acute charcot arthropathy of the wrist in a diabetic patient. Rheumatol Int 2013;33:2959-60. [Google Scholar | PubMed]
- 14.Xu K, Wu G, Zhang W, Yu W, Cui S, Zhang Z. Rapid spontaneous total fusion of neuropathic arthropathy of the wrist after limited intercarpal arthrodesis: A Case report and brief literature review. Front Surg 2022;9:771896. [Google Scholar | PubMed]