The case highlights the importance of early diagnosis and timely surgical intervention in spinal metastasis of renal cell carcinoma (RCC). Combining advanced anterior and posterior surgical techniques improves neurological outcomes, reduces pain, and enhances patient quality of life.
Dr. Hitesh Modi, Department of Spine Surgery, Zydus Hospitals and Healthcare Research Private Limited, Ahmedabad, Gujarat, India. E-mail: modispine@gmail.com
Introduction: Renal cell carcinoma (RCC) accounts for 2–3% of adult malignant tumors, often metastasizing to bones, especially the spine. Spinal metastasis has a poor prognosis, but solitary spinal tumors have better outcomes with targeted chemotherapy, radiotherapy, and newer surgical approaches. Due to RCC’s high vascularity and resistance to treatments, en bloc vertebrectomy with anterior and posterior fixation is the gold standard for solitary lesions. This case report discusses a young man with C-7 cervical vertebrae metastasis, causing right upper limb weakness and severe neck pain.
Case Report: A 43-year-old male presented with 4 weeks of neck pain (visual analogue scale score 7) radiating to the right upper limb, with tingling and numbness. Examination showed C7 tenderness, decreased power (4/5) in C7 and C8, and 50% reduced sensation. MRI revealed a metastatic hyperintense lesion at C7 causing collapse, anterior and posterior cortex bulging, anterior thecal sac indentation, and left neural foramen narrowing. He underwent anterior cervical thoracic exploration (C6-T1) with partial sternotomy, tumor excision, C7 corpectomy, cord decompression, MESH cage insertion, and anterior cervical plate fixation, followed by posterior C5–C6 lateral mass and T1–T2 pedicle screw fixation. Neurological power in C7–C8 improved from 4/5 to 5/5, and sensation reduction improved from 50% preoperatively to 10% at 12 weeks.
Conclusion: Advancements in primary disease treatment necessitate evolving strategies for cervicothoracic metastasis. Combining extensive anterior and posterior techniques is now standard, enhancing patient quality of life through effective support and stabilization. Early diagnosis and referral are essential for pain relief and preventing neurological deficits and cord compression. Total en bloc vertebrectomy, the gold standard for solitary spinal metastasis, should include pre-operative embolization to reduce intraoperative bleeding. Prognosis relies on timely diagnosis, histological grading, and a comprehensive approach incorporating both medical and surgical treatments.
Keywords: Renal cell carcinoma, spinal metastasis, en bloc, vertebrectomy, cervical vertebrae metastasis, anterior and posterior fixation.
Renal cell carcinoma (RCC) accounts for 2–3% of adult malignant tumors commonly occurring in the urinary system. Bone is the second most common site for metastasis after the lung and around 40% of this tumor occurs in the spine [1]. Metastatic lesions mainly localize most commonly at the thoracic spine in 68–80%, the lumbar spine in 16–22%, and the least common in the cervical spine in 8–15% [2]. Spinal metastasis has a poor prognosis; however, solitary spinal tumor has prolonged survival. New advancements in cancer treatment, targeted chemotherapy, radiotherapy to a specific location are associated with better outcomes and prolonged survival [3]. RCC metastasis is difficult to manage due to its high vascularity, highly destructive nature, and relatively resistance to chemotherapy and highly radioresistant, and embolization following angiography reduces intraoperative blood loss [4]. A skeletal biopsy is the gold standard treatment modality for diagnosis and treatment planning, However, metastasis to the spine in the cervical region can be planned for en bloc resection to decrease the local destruction and local disease progression [4]. RCC is notorious for causing destruction and collapse of vertebral body, it leads to neurological deficit and cord compression. The gold standard treatment of the solitary lesion from this tumor is en bloc vertebrectomy followed by anterior and posterior fixation procedures [5]. Patients presenting with pathological vertebral body fracture present with pain due to instability and neurological deficit due to cord compression. This requires anterior column reconstruction, only posterior fixation leads to fatigue of screws and rods; ultimately, the body will collapse after repetitive load. In this case report, we present the systemic approach to a young man presenting with C-7 cervical vertebrae metastasis with collapse leading to weakness in the right upper limb and severe neck pain with tingling and numbness.
A 43-year-old male presented with 4 weeks of neck pain (visual analogue scale [VAS] score 7) radiating to the right upper limb and associated with tingling and numbness of the same duration; on examination, tenderness was present at C7 spinous process with a decrease in power of 4/5 in C7 and C8 destribution and 50% reduction in sensation over same dermatomes.
Diagnostic studies
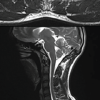
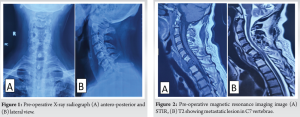
The plain cervical radiograph (Fig. 1) on antero-posterior and lateral view showed osteolytic lesion with wedging of C7 vertebral body (>50% of height loss). On MRI (Fig. 2), hypointense lesion (T1W sequences), hyperintense lesion (T2W and STIR sequences) of C7 vertebral body showing collapse and bulging anterior and posterior cortex. it also shows indentation over anterior thecal sac along with left posteriolateral extension of soft tissue causing narrowing of left neural foramen of C7-T1 compressing nerve root. MRI also suggests, anteriorly soft tissue component extending into pre and paravertebral space from C6 to D1-D2 disc space on right measuring 5×1.8×6 cm. On CT-angiography, pre and paravertebral soft tissue extending from C6 to D2 was noted without any obvious arterial feeder.
Pre-operative embolization
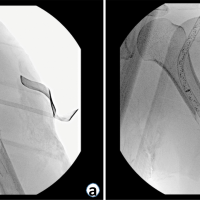
Metastasis from RCC is highly vascular tumor and pre-operative angiography was performed within 48 h before surgery for tumor embolization. However, no tumor feeding vessel was identified.
Surgery
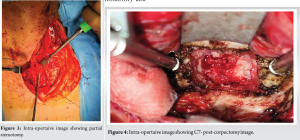
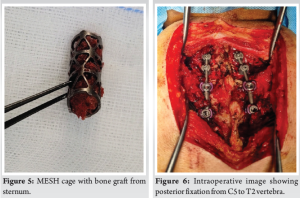
The patient underwent anterior cervical thoracic exploration C6-T1 with partial sternotomy (Fig. 3), tumor excision and biopsy, C7 corpectomy (Fig. 4), cord decompression, and MESH cage insertion with bone graft (Fig. 5) with anterior cervical plate fixation, followed by posteriorly C5-C6 lateral mass fixation and T1-T2 pedicle screw fixation (Fig. 6) under general anesthesia. The amount of intra-operative blood loss was around 300 ml. For exposure of the tumor anteriorly, an oblique incision parallel to the medial border of the sternocleidomastoid muscle was taken extending over the sternum. Partial manubrium resection was done to mobilize the carotid artery and internal jugular veins (Fig. 7), to expose the vertebrae anteriorly up to T4 with careful dissection. Extensive tumor excision, C7 corpectomy, and biopsy were done.
Pathology
On histopathology examination, it was found to be a metastatic clear cell renal carcinoma with sarcomatoid features. On immune-histo-chemistry examination, tumor cells were positive for PANCK, PAX 8, Vimentin, CD10, and focally for CK7. They were negative for EMA, AMACR, and CD117. INA-1 nuclear expression was retained.
Follow-up
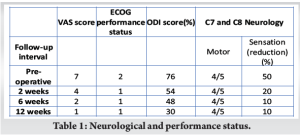
It is important to include both neurologic and performance status, when reviewing outcomes in cancer patients. For pain status, VAS severity score was used and for performance status, Eastern Cooperative Oncology Group (ECOG) was used ( 2-ambulatory but bedridden <50% of the time, 1-restricted strenuous activity but ambulatory and able to perform light work). VAS score was improved form 7 preoperatively to 4, 2, and 1 on 2 weeks, 6 weeks, and 12 weeks, respectively. ECOG performance status was improved from 2 preoperatively to 1 postoperatively. ODI score was improved 76 preoperatively to 54 postoperatively and 30 on 12 -week follow-up. Neurological status was improved, in terms of power over C7-C8, 4/5 to 5/5 postoperatively and sensation reduction of 50% preoperatively to 20% on 2 weeks and 10% on 12-week follow-up (Fig. 8 and Table 1).

RCC is the most common malignancy in the kidney with around 50% of them having bony metastasis. The average life expectancy after the malignancy is 12–24 months with the worst prognosis when it metastases to the axial spine [5]. It is difficult to treat malignancy because of, relatively resistant to chemotherapy and radiotherapy. RCC metastatic deposits weaken and destroy the vertebral body biomechanically, leading to instability. If not addressed, it leads to pathological fracture, causing neurological deficit and severe pain due to metastatic spinal compression in 5–14% of the patients [6]. The gold standard treatment for solitary spinal metastasis is en bloc vertebrectomy, followed by anterior and posterior stabilization. Only posterior stabilization is not recommended due to, an absence of anterior column support fails to address the pain and leads to metalwork fatigue and failure. It also reduces the need for complex revision surgery in the future. Following en bloc vertebrectomy, the anterior column can be reconstructed using a mesh cage with bone graft and anterior plate fixation. In the cervical spine, RCC mainly metastases to the vertebral body, and the surgical approach to C7-T1 can be challenging. Mesfin et al. have mentioned in their review about an anterior approach to C7-T1, by including the manubrium or clavicle splitting approach along with the Smith–Robinson approach [2]. When planning for resection, it is important to keep in mind the high vascularity and rapidly expansile nature of the tumor, which makes resection of this tumor sometimes hazardous. Considering the high risk for hemorrhage in these patients, pre-operative diagnostic angiography followed by embolization of the feeding vessel is recommended. Surgical intervention followed by embolization has to be done as soon as possible, due to the possibility of recanalization, 48 h post-embolization is recommended. This procedure has shown an advantage in literature by enabling surgeons a hassle-free resection, uncontrollable intraoperative bleeding, and resection of extensive metastatic tumor-causing cord compression [3,7]. For patients presenting with cervical metastatic lesions with a risk of pathological fracture, prophylactic stabilization should be considered, due to the risk of spinal instability and cord compression. Cement augmentation also has been recommended in these patients to stabilize the vertebral body, which will offer pain relief and anterior stabilization [5]. RCC is an aggressive, metastatic malignancy, with the least involvement of the cervical spine. Management of this malignancy has been challenging, they are often treated with a multimodality approach including radiosurgery, systemic cancer therapies, surgical decompression, and palliative care. The recent modalities of treatment such as tyrosine kinase inhibitors, mammalian target rapamycin (mTOR) inhibitors, and immune checkpoint inhibitors have shown better outcomes in the past decade [8]. The main goal of the treatment is to increase life span, quality of life, overall survival, pain relief, and neurological improvement. Goodwin et al. in their review of 807 patients, following surgery 70.7% of the patients had pain relief and neurological improvement. They have also mentioned the mean survival of the patients, who underwent medical treatment, surgical treatment, and surgical treatment with embolization was 8.3, 16.2, and 15.6 months, respectively [3]. Histological grade also plays an important role in the prognosis of the patient apart from the grading system described by Tokuhanshi et al. [9]. For cervical spine metastasis requiring C7-T1 exposure, anterior decompression with, augmentation with a cage with bone graft through extensive anterior approach including partial manubrium excision followed by posterior fusion is recommended, along with primary treatment of the RCC to relieve pain and neurological improvement aiding to overall survival of the patient [10]. The novelty of this approach lies in the fact that C7-T1 is a very difficult region to access anteriorly due to the presence of vital neurovascular structures. RCC is a highly vascular tumor, making its safe removal a challenging task. The approach we have described in the case report allows for a safer access to the tumor, enabling its removal with fewer complications. At our hospital, we follow a standard protocol that includes involving an onco-surgeon, a vascular surgeon, and a senior anesthetist as part of the team. Thorough pre-operative investigations and proper patient counseling are conducted beforehand. Postoperatively, the patient is kept in the Intensive Care Unit for monitoring of potential complications such as hematoma, breathing difficulties, and difficulty swallowing. We also place a Ryle’s tube in patients undergoing anterior cervical spine surgery.
As the advancement of the primary treatment of the primary disease has evolved, the secondary treatment for the challenging metastasis to the cervicothoracic area is also needed. Through extensive anterior approach combined with a posterior approach is safe and aids in the quality of life of the patient. It is also becoming the standard of care by providing anterior support and posterior stabilization, helping in palliation of the patient. With prompt diagnosis and early referral, helps patients with early pain relief and saves them from neurological deficits and cord compression complications. Total en bloc vertebrectomy being a gold standard treatment for solitary spinal metastasis, pre-operative embolization should be done, for safe removal and decreasing massive hemorrhage intraoperatively. The prognosis of the patient depends on the early diagnosis, histological grading, and medical treatment along with surgical treatment.
Advancements in primary disease treatment now include secondary management for cervicothoracic metastasis, with anterior and posterior approaches improving patient quality of life. Early diagnosis and referral, along with total en bloc vertebrectomy and pre-operative embolization, are essential for optimal outcomes.
References
- 1.Zhai J, Liu N, Wang H, Huang G and Man L. Clinical characteristics and prognosis of renal cell carcinoma with spinal bone metastases. Front Oncol 2021;11:659779. [Google Scholar | PubMed]
- 2.Mesfin A, Buchowski JM, Gokaslan ZL, Bird JE. Management of metastatic cervical spine tumors. J Am Acad Orthop Surg 2015;23:38-46. [Google Scholar | PubMed]
- 3.Goodwin CR, Ahmed AK, Boone C, Abu-Bonsrah N, Xu R, Germscheid N, et al. The challenges of renal cell carcinoma metastatic to the spine: A systematic review of survival and treatment. Glob Spine J 2018;8:517-26. [Google Scholar | PubMed]
- 4.Louie PK, Sayari AJ, Frank RM, An HS, Colman MW. Metastatic renal cell carcinoma to the spine and the extremities: Evaluation, diagnosis, and treatment. JBJS Rev 2019;7:e7. [Google Scholar | PubMed]
- 5.Langdon J, Way A, Heaton S, Bernard J, Molloy S. The management of spinal metastases from renal cell carcinoma. Ann R Coll Surg Engl 2009;91:649-52. [Google Scholar | PubMed]
- 6.Patchell RA, Tibbs PA, Regine WF, Payne R, Saris S, Kryscio RJ, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: A randomised trial. Lancet 2005;366:643-8. [Google Scholar | PubMed]
- 7.Hadgaonkar S, Zawar A, Sanghavi S, Kothari A, Sancheti P, Shyam A. Spinal metastases from renal cell carcinoma: Case note with an overview. Interdiscip Neurosurg 2021;23:100994. [Google Scholar | PubMed]
- 8.Shankar GM, Van Beaver LA, Choi BD, Hadzipasic M, Sivaganesan A, Karhade AV, et al. Survival after surgery for renal cell carcinoma metastatic to the spine: Impact of modern systemic therapies on outcomes. Neurosurgery 2020;87:1174-80. [Google Scholar | PubMed]
- 9.Tokuhashi Y, Uei H, Oshima M, Ajiro Y. Scoring system for prediction of metastatic spine tumor prognosis. World J Orthop 2014;5:262-71. [Google Scholar | PubMed]
- 10.Dürr HR, Maier M, Pfahler M, Baur A, Refior HJ. Surgical treatment of osseous metastases in patients with renal cell carcinoma. Clin Orthop Relat Res 1999;367:283-90. [Google Scholar | PubMed]