In the context of tibial tubercle fractures, peroneal nerve and isolated EHL palsies can occur independent of compartment syndrome, and eventually resolve within 3–6 months with non-operative management. Surgical management may be considered if symptoms do not resolve during that period.
Dr. R. Jay Lee, Department of Orthopaedic Surgery, The Johns Hopkins Hospital, 1800 Orleans St, Baltimore, MD 21287, USA; E-mail: editorialservices@jhmi.edu, rlee74@jhmi.edu
Introduction: Nerve palsies are potential consequences of fractures that can result in temporary loss of muscular function. Nerve palsies have not been extensively described in the context of tibial tubercle fractures in the pediatric population. Although the symptoms accompanying nerve palsies concern patients, evidence suggests that non-operative management often results in full functional recovery over time. Our case contributes to the available literature to demonstrate this point, even when neurologic deficits seem abnormally prolonged.
Case Presentation: We describe a case of isolated left extensor hallucis longus (EHL) palsy in a 15-year-old African American male patient, who initially presented to our institution’s emergency department with a left knee injury. While playing basketball, he sustained a left proximal fibular shaft fracture with a displaced tibial tubercle. Open reduction and internal fixation were performed to stabilize the tibial fracture; however, he developed an EHL palsy that persisted for 3 months postoperatively. Nerve conduction studies found substantial left peroneal neuropathy. The patient received physical therapy throughout this time. With nothing other than non-operative management, he recovered full function 7 months after the initial injury with no further complications.
Conclusion: We are aware of only 3 other published reports of isolated EHL palsy, each with unique causes. Our report may be one of the first documented cases of a tibial tubercle fracture with peroneal nerve palsy resulting in an isolated EHL deficit. It is important for clinicians and patients to be aware that even prolonged nerve and muscular deficits can be expected to resolve with non-operative management.
Keywords: Extensor hallucis longus, peroneal nerve palsy, tibial tubercle fracture
Tibial tubercle fractures occur most often in boys aged 12–15 years as they approach skeletal maturity [1]. Such fractures are uncommon, representing 3% of all proximal tibia fractures and < 1% of all physical fractures in the adolescent population. However, they are increasing in frequency because of increased participation in youth sports [1-4]. These injuries often result from forceful contractions of the quadriceps muscle against resistance or from rapid knee flexion – movements most frequently performed during sports that involve running and jumping [4,5]. Common risk factors include Osgood-Schlatter disease, osteogenesis imperfecta, and body mass index values that are very low or very high [1]. Although complications from tibial tubercle fractures are infrequent, injury to the soft tissue surrounding the tibial tubercle may be more extensive than appreciated on physical examination [6]. Therefore, it is critical to thoroughly evaluate patients for concomitant conditions (e.g., compartment syndrome) [6]. Unlike compartment syndrome, nerve palsies associated with these fractures have not been discussed extensively in the literature. We are aware of only three published cases of isolated extensor hallucis longus (EHL) injuries that are independent of compartment syndrome and concomitant lower-extremity muscle injury [7-9], making prognostication of outcomes and recovery timelines difficult. We present the case of a pediatric patient who sustained a tibial tubercle fracture and a proximal fibular shaft fracture and who had concomitant peroneal nerve palsy and isolated EHL palsy. This issue was resolved 7 months later. Given the origin of the EHL being far distal to the tibial tubercle, direct muscle injuries are not typically expected with such tubercle fractures. Consequently, we anticipate this case is one of the few reported of its kind, where such a palsy was sustained after a tibial tubercle fracture and can help clinicians who encounter similar injuries differentiate them from acute compartment syndrome given our patient’s clinical vignette upon initial presentation. The patient involved in this case was informed that data concerning the case would be submitted for publication, and consent was provided.
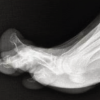
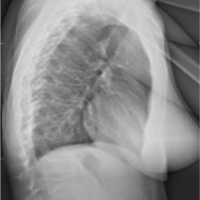
A 15-year-old boy with no relevant medical history presented to our hospital’s emergency department with a left knee injury. While jumping during a basketball game, he felt a “snap” in his knee upon landing, then withdrew from the game. Conventional radiographs taken in the emergency department revealed a left proximal tibia Ogden type-4 fracture and a transverse fibular shaft fracture. Pre-operative examination revealed intact sensation throughout the ankle and foot. Motor examination revealed 5/5 strength of the flexor hallucis longus, the tibialis anterior, and the gastrocnemius and soleus, but 0/5 strength of the EHL. The compartments were soft. Surgical treatment was planned because of the fracture’s displacement. After an unsuccessful attempt at closed reduction, open reduction was successfully performed. The fracture was stabilized with two screws. The leg remained well-perfused with soft compartments. A long-leg cast was applied, and the patient was monitored overnight before being discharged the next day. The patient followed up in 4 weeks and reported no acute changes. He had no issues with immobilization or the use of a walker, and he was able to bear weight through the cast. The cast was removed for examination, revealing mild edema of the lower leg but no evidence of subacute compartment syndrome. He still had an EHL deficit and now noted decreased sensation over the great toe. At 9 and 11 weeks postoperatively, the EHL deficit persisted. Electromyographic and nerve conduction studies were requested without a clear cause for the lack of EHL function. The nerve conduction study found substantial left peroneal neuropathy at 4 months postoperatively. Physical therapy continued throughout this time. At 6 months postoperatively, the patient presented to the clinic, stating that he was doing well and had returned to school. He had normal musculoskeletal and neurologic examinations. He had progressed to high-level agility and jumping and was cleared for full return to sport with instructions to follow up as needed. Pre-operative and intraoperative fluoroscopic radiographs of the fracture and repair are shown in Fig. 1.

We describe a patient with a tibial tubercle fracture with peroneal nerve palsy and subsequent EHL deficit, independent of compartment syndrome. A search of PubMed using the keywords “EHL palsy,” “peroneal nerve and EHL palsy,” “tibial tubercle fracture,” “isolated EHL palsy,” and “pediatric tibial tubercle fracture” identified only three published cases of isolated EHL deficits in the context of such injuries. Boyce and Prewitt [7] described a case of isolated EHL denervation that occurred in a 17-year-old male patient secondary to anterior cruciate ligament reconstruction, yet interestingly, the authors were unable to determine the mechanism of nerve injury. Eight weeks after the anterior cruciate ligament reconstruction, the patient continued to have a left toe drop. However, after 12 months of continued observation, he ultimately regained full toe extension. Estrella and Eufemio [8] reported a similar case of a patient who sustained isolated EHL denervation secondary to knee arthroscopy. The authors of this case treated the patient’s post-operative weakness surgically with a tendon transfer of the EHL to the extensor digitorum longus. Moorman and Pontious [9] reported a case of EHL dysfunction that they believed occurred secondary to peroneal nerve entrapment and subsequent compression. The final treatment plan included a customized hallux brace, physical therapy that focused on EHL strengthening, and periodic reevaluation. Three months later, the patient regained manual muscle strength of the EHL (rated as 1–2/5). The patient decided to continue using the brace and to follow up periodically until full recovery. Our patient’s deficit was ultimately resolved. The cases described herein can serve as guidance for appropriate management. Boyce and Prewitt [7] reported a patient who experienced full recovery at 12 months postoperatively with no additional interventions, whereas Moorman and Pontious [9] noted some recovery but did not describe whether their patient fully recovered. Regardless, they were able to help their patient regain function through physical therapy and bracing. Conversely, Estrella and Eufemio [8] saw no recovery of a dropped big toe in their patient at both 1- and 2-year follow-ups, with the patient ultimately undergoing a tendon transfer 2 years after the initial surgery. More broadly, published evidence supports our findings that peroneal nerve neuropathies can be managed initially with non-operative modalities, with surgical intervention indicated only for an open wound at initial presentation or a lack of functional recovery at more than 7 months after injury [10]. Given that our patient successfully regained EHL extension 6 months postoperatively, our case and the current literature suggest that non-operative management is appropriate.
Although rare, isolated paralysis of the EHL has been reported secondary to osteotomy, intramedullary nailing, and anterior cruciate ligament reconstruction. We report the case of a patient who developed isolated EHL palsy after a tibial tubercle fracture and who ultimately regained EHL strength 6 months postoperatively. Isolated instances of EHL deficit and peroneal nerve palsy may spontaneously or gradually resolve, as seen in our case. Although EHL tendon transfers have been used in previous unresolved cases of this deficit, evidence suggests that non-operative management can be the mainstay of treatment.
With limited published evidence of appropriate management for isolated and prolonged nerve deficits in the setting of pediatric lower-extremity fractures, our case report strengthens the case for initial non-operative management, despite how prolonged these deficits may be. We describe a patient whose EHL deficit is ultimately resolved with physical therapy.
References
- 1.Reyes CD, Wu W, Pandya NK. Adolescent tibial tubercle fracture: Review of outcomes and complications. Curr Rev Musculoskelet Med 2023;16:392-7. [Google Scholar | PubMed]
- 2.Yousef MA. Combined avulsion fracture of the tibial tubercle and patellar tendon rupture in pediatric population: Case series and review of literature. Eur J Orthop Surg Traumatol 2018;28:317-23. [Google Scholar | PubMed]
- 3.Hamilton SW, Gibson PH. Simultaneous bilateral avulsion fractures of the tibial tuberosity in adolescence: A case report and review of over 50 years of literature. Knee 2006;13:404-7. [Google Scholar | PubMed]
- 4.Shin YW, Kim DW, Park KB. Tibial tubercle avulsion fracture according to different mechanisms of injury in adolescents. Medicine (Baltimore) 2019;98:e16700. [Google Scholar | PubMed]
- 5.Pandya NK, Edmonds EW, Roocroft JH, Mubarak SJ. Tibial tubercle fractures: Complications, classification, and the need for intra-articular assessment. J Pediatr Orthop 2012;32:749-59. [Google Scholar | PubMed]
- 6.Pape JM, Goulet JA, Hensinger RN. Compartment syndrome complicating tibial tubercle avulsion. Clin Orthop Relat Res 1993;295:201-4. [Google Scholar | PubMed]
- 7.Boyce DA, Prewitt C. Great toe drop following knee ligament reconstruction: A case report. Physiother Theory Pract 2020;36:340-6. [Google Scholar | PubMed]
- 8.Estrella EP, Eufemio MT. Isolated extensor hallucis longus paralysis after knee arthroscopy: A case report. Foot Ankle Online J 2008;1:2. [Google Scholar | PubMed]
- 9.Moorman CD, Pontious J. Compression peroneal nerve palsy causing isolated extensor hallucis longus dysfunction. J Foot Ankle Surg 2009;48:466-8. [Google Scholar | PubMed]
- 10.Baima J, Krivickas L. Evaluation and treatment of peroneal neuropathy. Curr Rev Musculoskelet Med 2008;1:147-53. [Google Scholar | PubMed]