Pneumothorax is a rare complication of clavicle fractures. Adequate and prompt assessment with chest radiographs is recommended for prompt treatment of this potentially life-threatening complication.
Dr. Hasjmy Mohamad, Department of Orthopaedic Surgery, Changi General Hospital, Singapore. E-mail: mohamad.hasjmy@mohh.com.sg
Background: Clavicle fractures are the fourth most common fracture. These fractures are either managed conservatively or surgically. Pneumothorax is a rare complication of clavicle fractures and potentially can be missed if this rare complication is not known.
Case Report: A 76-year-old female presents with a 2-day history of pain and bruising over the right clavicular prominence following a fall from a standing height. Subsequent radiographs show the development of pneumothorax, despite having no respiratory symptoms.
Discussion: Pneumothorax as a complication of isolated clavicle fractures is rare, with no case reports of hydropneumothorax in the literature. We hypothesize that the posterior displacement of the clavicle fragment penetrated the lung pleura resulting in the pneumothorax. We propose routine chest radiographs for patients presenting with clavicle fractures to rule out pneumothorax for the three reasons below. (1) Clinical features of pneumothorax might not be present upon patient’s initial presentation, especially if they are relatively healthy individuals(2) Adequate pre-operative management if the patient is for surgical intervention (3) Assessment of surgical complications if the patient is for surgical intervention as iatrogenic pneumothorax is a potential complication of surgical fixation.
Conclusion: Thorough clinical examination and radiological evaluation should be performed with the diagnosis of pneumothorax in mind when a patient presents with a clavicle fracture to ensure early diagnosis and treatment of this life-threatening complication.
Keywords: Clavicle fracture, pneumothorax, hydropneumothorax.
Clavicular fractures represent 2.6% of all fractures [1] and it is the fourth most common fracture [2]. About 69–82% of all clavicular fractures occur in the midshaft [3]. Pneumothorax is a known rare complication of clavicle fractures [4]. Pneumothorax is defined as the presence of air in the pleural space. This can be further subclassified as traumatic pneumothorax where the pleura is pierced, most commonly by rib fractures in the context of thoracic trauma [5]. Pneumothoraxes can be potentially fatal as it might develop into tension pneumothorax regardless of the size, hence, prompt diagnosis, close monitoring, and adequate management should be performed for the patient [6]. We report a case of a hydropneumothorax secondary to a clavicular fracture, which required chest drain insertion for treatment.
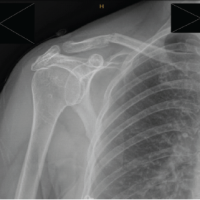
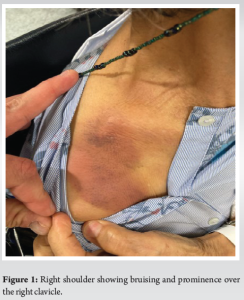
A 78-year-old female presented to the emergency department 2 days after she slipped on a wet toilet floor due to persistent pain and bruising over the right clavicular prominence. She presented to a general practitioner who advised her to present to the emergency department for further evaluation. She has a background of osteoporosis on denosumab and recently recovered from COVID which she self-isolated upon a positive COVID-19 Antigen Rapid Test 1 week before the presentation. Upon review in the emergency department, the patient was slightly hypertensive but otherwise stable and saturating well on room air. Prominence of the right clavicle as compared to the contralateral side was noted, with surrounding bruising (Fig. 1). Prominence was reduced upon placing the arm in an arm sling. No neurovascular deficits were noted.
Upon admission, X-rays of the right clavicle, anteroposterior, and axial views were performed (Fig. 2 and 3), noting a displaced, comminuted right clavicle midshaft fracture. A repeat set of X-rays above was performed to assess the displacement after the application of the arm sling. In addition to the repeat X-rays, a chest X-ray was performed of which a right pneumothorax of 3.8 cm apicopleural distance was noted (Fig. 4).

 Retrospectively, the pleural line was noted on the right clavicle X-rays initially performed. As the patient remained hemodynamically stable with no objective desaturation, the patient was initially managed conservatively with interval chest X-rays and oxygen supplementation of 2 L/min on nasal prongs. A computed tomography scan of the chest was performed on the 2nd day of admission to evaluate for potential causes of secondary pneumothorax, which revealed the following pertinent findings (Fig. 5).
Retrospectively, the pleural line was noted on the right clavicle X-rays initially performed. As the patient remained hemodynamically stable with no objective desaturation, the patient was initially managed conservatively with interval chest X-rays and oxygen supplementation of 2 L/min on nasal prongs. A computed tomography scan of the chest was performed on the 2nd day of admission to evaluate for potential causes of secondary pneumothorax, which revealed the following pertinent findings (Fig. 5).
- A moderate right-sided hydropneumothorax with a maximum interpleural distance of 2.6 cm and no mediastinal shift
- Segmental atelectasis/collapse in the right lung base
- Stable 0.5 cm nodules in the left upper lobe apicoposterior segment. Biapical pleural thickening is seen
- No suspicious pulmonary mass or consolidation.
Surgical intervention for the clavicle fracture was offered and accepted to which open reduction and internal fixation of the right clavicle was performed. A 20F chest tube was inserted above the right fifth rib on passive drainage before induction of general anesthesia, which drained serous fluid. This was performed under general anesthesia in a beach chair position. An anterior approach was used with a longitudinal incision. Intraoperative imaging was performed with a C-arm. The fracture was washed and debrided, reduced, and held in place with a Kirschner wire. A Synthes 6-hole LCP superior anterior clavicle plate was used with six locking screws on the lateral fragment and three screws over the medial fragment. 0.5cc of Synthes demineralized bone matrix was applied to the bone loss over the anterior aspect of the fracture site. Closure included platysma closed over the plate and subsequently closed in layers. Postoperatively, patient was rehabilitated with a clavicle open reduction and internal fixation protocol. Post-operative radiographs were performed as shown in Figs. 6 and 7. The chest tube was subsequently removed on the 5th day of admission and was discharged well without further significant events.

In our literature review, pneumothorax as a complication to clavicle fractures is rare. A search on PubMed Central reveals only 12 case reports of isolated clavicle fractures resulting in pneumothorax. There have been no case reports of hydropneumothorax secondary to clavicle fracture. From the initial X-ray on arrival to the Emergency Department (Fig. 1), it is plausible that the posterior displacement of the lateral fragment penetrated the lung pleura, resulting in the pneumothorax. Current standard practice does not advocate for routine Chest X-ray when presented with a clavicle fracture unless a pneumothorax is clinically suspected. This includes signs and symptoms such as tachypnea, dyspnea, and reduced oxygen saturation. However, such signs and symptoms may not manifest in all patients with a pneumothorax. Rib fractures are a common cause of pneumothoraxes, and they are commonly associated with injuries. Chest radiographs are sufficient in the detection of rib fractures [7], and would confer the additional benefit of screening for concomitant rib fractures. There has been an increase in operative treatment for clavicle fractures over the recent years [8,9]. Indications for surgical intervention are described below:
- Displacement (shortening of more than 20mm on the frontal plane, more than 15mm in younger and higher demand patients), due to increased risk of non-union, malunion, and reduced functional outcome [10]
- Emergency surgery if exploration is required for compromise of neurovascular structures, or open fractures.
A consideration in this case wound includes intrapleural penetration which might suggest interposed pleural or pulmonary tissue in the fracture site which would increase the risk of non-union if treated conservatively [11]. In clavicle fractures that are managed surgically, it would also be prudent to assess pre-operatively with a chest radiograph for two main reasons.
- Adequate pre-operative management
An undiagnosed pneumothorax might develop into tension pneumothorax during intubation and induction of general anesthesia [12]. Early detection would allow for the appropriate subsequent management of the patient which would include oxygen supplementation [13], and insertion of a chest tube before induction of general anesthesia with some considerations as positive pressure ventilations and nitrous oxide may exacerbate the pneumothorax or cause a tension pneumothorax [14].
- Assessment of surgical complications
Iatrogenic pneumothorax is a known complication of surgical fixation [15]. Subsequent management of the patient found to have a pneumothorax after the surgical fixation of the clavicle would possibly differ if it was a result of instrumentation as compared to if it was due to the initial injury.
Pneumothorax is a potentially life-threatening diagnosis that could be missed in the setting of clavicular fractures, regardless of the energy of trauma, especially in healthier patients where the symptoms are not significant. While the apex of the ipsilateral lung is usually visualized in a clavicular X-ray, subtle radiological changes to the lung fields may not be immediately discernible. Hence, we propose that a thorough clinical examination and chest radiograph be performed as part of the radiograph series for all clavicle fractures for early diagnosis and treatment of this potential complication.
Pneumothorax is a rare complication of clavicle fractures. Adequate and prompt assessment with chest radiographs is recommended for prompt treatment of this potentially life-threatening complication.
References
- 1.Postacchini F, Gumina S, De Santis P, Albo F. Epidemiology of clavicle fractures. J Shoulder Elbow Surg 2002;11:452-6. [Google Scholar | PubMed]
- 2.Karl JW, Olson PR, Rosenwasser MP. The epidemiology of upper extremity fractures in the United States, 2009. J Orthop Trauma 2015;29:e242-4. [Google Scholar | PubMed]
- 3.Kihlström C, Möller M, Lönn K, Wolf O. Clavicle fractures: epidemiology, classification and treatment of 2 422 fractures in the Swedish Fracture Register; an observational study. BMC Musculoskelet Disord 2017;18:82. [Google Scholar | PubMed]
- 4.Amer KM, Congiusta DV, Suri P, Choudhry A, Otero K, Adams M. Clavicle fractures: Associated trauma and morbidity. J Clin Orthop Trauma 2021;13:53-6. [Google Scholar | PubMed]
- 5.Zarogoulidis P, Kioumis I, Pitsiou G, Porpodis K, Lampaki S, Papaiwannou A, et al. Pneumothorax: From definition to diagnosis and treatment. J Thorac Dis 2014;6 Suppl 4:S372-6. [Google Scholar | PubMed]
- 6.Tran J, Haussner W, Shah K. Traumatic pneumothorax: A review of current diagnostic practices and evolving management. J Emerg Med 2021;61:517-28. [Google Scholar | PubMed]
- 7.Henry TS, Donnelly EF, Boiselle PM, Crabtree TD, Iannettoni MD, Johnson GB, et al. ACR appropriateness criteria® rib fractures. J Am Coll Radiol 2019;16:S227-34. [Google Scholar | PubMed]
- 8.Frima H, Van Heijl M, Michelitsch C, Van der Meijden O, Beeres FJ, Houwert RM, et al. Clavicle fractures in adults; current concepts. Eur J Trauma Emerg Surg 2020;46:519-29. [Google Scholar | PubMed]
- 9.Schneider P, Bransford R, Harvey E, Agel J. Operative treatment of displaced midshaft clavicle fractures: Has randomised control trial evidence changed practice patterns? BMJ Open 2019;9:e031118. [Google Scholar | PubMed]
- 10.Paladini P, Pellegrini A, Merolla G, Campi F, Porcellini G. Treatment of clavicle fractures. Transl Med UniSa 2012;2:47-58. [Google Scholar | PubMed]
- 11.DeAngelis RD, Graf KW Jr., Mashru RP. Intrapleural penetration of a clavicle fracture: An indication for operative fixation. J Orthop Case Rep 2017;7:17-20. [Google Scholar | PubMed]
- 12.Hsu CW. Iatrogenic pneumothorax related to mechanical ventilation. World J Crit Care Med 2014;3:8-14. [Google Scholar | PubMed]
- 13.Sharma A, Jindal P. Principles of diagnosis and management of traumatic pneumothorax. J Emerg Trauma Shock 2008;1:34-41. [Google Scholar | PubMed]
- 14.Paramasivam E, Bodenham A. Air leaks, pneumothorax, and chest drains. Contin Educ Anaesth Crit Care Pain 2008;8:204-9. [Google Scholar | PubMed]
- 15.Asadollahi S, Hau RC, Page RS, Richardson M, Edwards ER. Complications associated with operative fixation of acute midshaft clavicle fractures. Injury 2016;47:1248-52. [Google Scholar | PubMed]