PFN A2 provides good functional outcome and significantly less blood loss, surgical duration, and union time with better biomechanical stability than PFN in all types of inter trochanteric fracture.
Dr. Kaman Kuity, Department of Orthopaedic Surgery, Dr. D. Y. Patil Medical College, Hospital and Research Centre, Pune, Maharashtra, India. E-mail: Kamaniimsar11@gmail.com.
Introduction: Intertrochanteric fractures are one of the most common fractures around the pelvis and hip joint. Intrerotrochanteric fracture commonly occurs in elderly adult as a result of a simple domestic fall or slippage due to osteoporosis and young adult due to high-energy trauma. In 1990, 26% of all intertrochanteric fractures were reported in Asia, this figure is estimated to 32% in 2025 and 38% in 2050. The main purpose of our study to differentiate functional, radiological, and clinical outcomes of intertrochanteric fracture treated with Proximal Femoral Nail Anti-rotation and Proximal Femoral Nail Anti-rotation Asian.
Materials and Methods: This was a randomized prospective study of 68 intertrochanteric fracture patients (34 cases in the PFN group and 34 cases in the PFN A2 group) from February 2022 to April 2024. Data were collected based on the Harris Hip Score questionnaire at 6 weeks, 3 months, and 6 months and data were entered into Microsoft Excel. Demographic data, surgical duration, intraoperative blood loss, union rates, and complications were recorded and compared between both groups. Statistical analysis was done using Statistical Package for the Social Science software version 26.
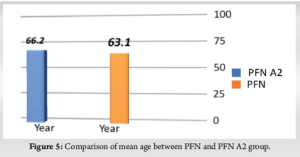
Results: The mean age was 66.2 ± 15.8 in PFNA2 group whereas 63.1 ± 16 years in PFN group. Majority of the patients were male (63.2%) in both groups whereas female constituting 36.8%. Surgical duration and intraoperative blood loss were significantly less in the PFN A2 group, but functional outcome at 6 weeks, 3 months, and 6 months; complications were not significantly different in both groups. Screw cutout noticed in PFN A2 whereas reverse Z effect observed in PFN follow-up cases
Conclusion: Our study infer that PFN A2 has significant advantages when compare to conventional PFN like statistically significant less surgical duration and intraoperative blood loss with faster union time with smaller incision. Implant-related complications are lesser in PFN A2 that indicate biomechanical dominance of helical blade device over conventional dual screw system.
Keywords: Intertrochanteric fracture, PFN, PFN A2.
Intertrochanteric fractures are one of the most common fractures around the pelvis and hip joint which spanning from extracapsular basilar neck region to lesser trochanter. Intrerotrochanteric fracture commonly occurs in elderly adult as a result of simple domestic fall or slippage due to osteoporosis and young adult due to high-energy trauma [1]. In upcoming years, annual incidence and health-care cost are anticipated to remarkably high because of aging and life expectancy. In 1990, 26% of all intertrochanteric fracture were reported in Asia; this figure is estimated to 32% in 2025 and 38% in 2050 [2,3].
The goal of treatment is to provide a pain-free, mobile, and steady hip with normal abductor lever arm function and return to pre-fracture activity level [4]. Early surgical treatment is essential is necessary in such fractures to achieve acceptable reduction and early rehabilitation of the patients. Implant failure was the most dreaded post-operative complication in the case of intertrochanteric fracture fixation which leads to poor functional outcome. Therefore, an ideal implant is required for appropriate fracture fixation and to get a good functional outcome.
Biomechanically intramedullary implants allow posteromedial cortex support and inhibit the collapse at fracture area leads to a high union rate with minimal soft tissue injury. Patient allows an early movement, thus reducing morbidity [5]. Fixation of unstable fracture using intramedullary nail and femoral head/neck stabilization with helical blade is now considered as an ideal method [6].
Various nail designs were incorporated for intertrochanteric fracture like a single blade or compression screw with anti-rotation screw (PFN). PFN includes an intramedullary nail through which two screws are introduced into femoral head and neck. One is lag screw that is stabilize fracture and allowing some amount of collapse. Another one is anti-rotation screw provide rotatory stability to fracture. Studies proven PFN was always better when compare with extra medullary implants, especially in unstable intertrochanteric fracture shown significantly high complications (31%) such as screw cutout, z effect, reverse z effect, varus collapse, and rotational instability [7].
PFN A2 was introduced in 2004 which utilizes a single helical blade, alternative of the conventional two screws [8]. The helical blade allows compression, rotational control as well as magnificent stability of fracture fixation by increasing bone implant interface and cancellous bone compaction. Biomechanical studies have shown that PFN A2 provides better resistance against rotation and varus collapse due to consolidation of cancellous bone. Hence, there is a less chance of implant failure in PFN A2 [9,10].
The main purpose of our study to differentiate functional, radiological, and clinical outcomes of intertrochanteric fracture treated with Proximal Femoral Nail Anti-rotation and Proximal Femoral Nail Anti-rotation Asian.
This was a randomized prospective study of 68 inter trochanteric fracture patients (34 cases in PFN group and 34 cases in PFN A2 group) from February 2022 to April 2024. With 95% confidence interval, 80% power taking a large effect size (0.7) among two groups and G × power 31.9.2 version the sample size come out 68, 34 in each group. All odd serial number patients who come to OPD/emergency department was treated with PFNA2 and even number patients was treated with PFNA. The study was conducted in the Department of Orthopaedics of D.Y.Patil medical college after getting approval from Thesis and Ethical Committee. Our study included all types of closed intertrochanteric fracture with a history of trauma less than 3 weeks, patients aged 18–90 years of both sexes, occurred due to any mode of injury. Pathological fracture, compound fracture, skeletally immature individuals, medically unfit patients, osteoarthritis, and neurovascular injury of hip were excluded from the study.
Data were collected based on Harris Hip Score (HHS) questionnaire at 6 weeks, 3 months, and 6 months and data entered into Microsoft Excel. Statistical analysis was done by using Statistical Package for the Social Science software version 26. Descriptive statistical analysis was done by mean, proportion, and SD. Interferential statistics was done using Chi-square test and t-test. 0.05 or less was set as a statistical significance. Demographic data, surgical duration, intraoperative blood loss, union rates, and complications were recorded and compared between both groups.
Pre-operative assessment
Preoperatively, all cases were analyzed clinicoradiologically to rule out any associated injury. Local examination was done to rule out any open wound. X-ray PBH (anteroposterior and cross table lateral view) were obtained in all cases to see the extended of deformity, classification, and pre-operative planning.
Routine investigation such as complete hemogram, liver and renal function test, viral screening, chest X ray, and echocardiogram were done in all cases. Ankle traction with 4–5 kg weight were applied in every patient until fracture fixation. All patients were posted for surgery after securing proper consents. Most of the patients were elderly and associated with comorbidities. Hence, cardiologist and general physician opinion taken before surgery.
Surgical technique
All patients were positioned supine on fracture table under suitable anesthesia. Affected leg positioned in traction boot and fracture site was aligned by traction and internal rotation under fluoroscopy guidance. Operated limb is in traction, internally rotated and adducted around traction post and flex the trunk laterally to make it possible to enter proximal femur through lateral aspect of buttock with unaffected limb was flexed and abducted to provide adequate space for C-arm.
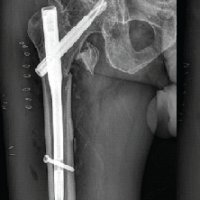
A 4–5 cm incision made 5 cm proximal to the greater trochanter after proper antiseptic draping and incision deepened to split subcutaneous tissue, fascia lata, and gluteus muscle. Entry was made with a cannulated awl over tip of greater trochanter in AP view and junction of anterior two-third and posterior one-third in lateral view along anatomical axis of femur. Then, insert a guidewire into medullary canal through entry hole. Check guide wire position on AP and lateral view with image intensifier (Fig. 1).
Proximal canal reamed by fair force from 5 cm of proximal femur and insert appropriate size of PFN/PFNA2 with the help of locking zig. In some cases, reduction was achieved by manipulation with a steinmann pin before incision was made.
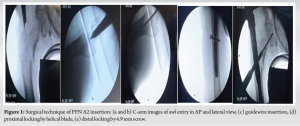
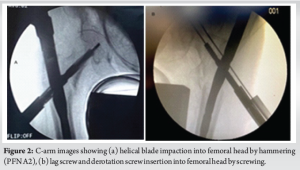
Basic difference in PFN and PFN A2 is a single helical blade used in PFNA2 whereas one derotation screw (6.3 mm) and one lag screw (8 mm) used in PFN. Guidewires inserted through sleeves and zig for proximal screw/ blade fixation under C arm guidance. Proximal 5 cm canal reamed by fair force. Another same-length guidewire used to determine screws/blade length. Appropriate size neck screws fixed with screw driver after drilling lateral cortex (Derotation screw length was usually 15mm less than lag screw)in PFN whereas single helical blade fixed by hammering in PFNA2 and confirmed under fluoroscopy (Fig. 2). Hence, incision length for proximal locking was smaller in PFN A2 (Fig. 3). Distal locking was done by 4.9 mm screws. Close fascia lata and skin by subcuticular sutures and apply pressure dressing.
Post-operative rehabilitation
Physiotherapy plays a significant role to regain hip range of motion and improving functional outcome of hip. When fixation is steady, we can start early rehabilitation. Significant range of motion is regain within few post-operative weeks. Non-weight bearing walking started from 2nd post-operative day for each patient.
Primary aim of post-operative rehabilitation is to regain a significant range of motion and start weight-bearing walking as early as possible. Quadriceps strengthening, stretching exercises of hamstring, hip, knee, and ankle range of motion started from post-operative day 1.
Early phase(1st week)
- Improve early hip and knee range of motion.
- Relief surgical site pain and discharge the patient as early as possible.
- Prevent the deep vein thrombosis and embolism incidences.
- Walking with walker without bearing weight on operated limb started from second post-operative day.
Suture removal done between post-operative day 12–14. Partial weight bearing walking was started by 6 weeks of surgery in all patients and full weight-bearing walking started after 12 weeks in most of the patients.
In this study, 68 intertrochanteric fracture patients were included in the study, of which 34 patients were treated by PFN and another 34 patients were treated by PFNA2 (Fig. 4). All patients were come for follow-up 2 weekly till radiological union and then every month until 6-month postoperatively. Clinically fracture site tenderness, range of movement, any deformity recorded in each visit, and radiological sign of union were assessed by anteroposterior and cross-table lateral radiograph of operated hip. Functional outcome was measured by HHS at 3-week, 3-month, and 6-month follow-up. All patients were operated within 2–4 days of admission.

The mean age was 66.2 ± 15.8 in PFNA2 group ranging from 25 to 87 years. The age group in PFN varied from 23 to 90 years with average age of 63.1 ± 16 years (Fig. 5). Majority of the patients were male (63.2%) in both groups whereas female constituting 36.8% (Fig. 6). Left side was predominantly affected in both groups, around 54.4 % of all patients (Fig. 7).
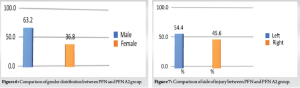
Domestic fall was the most common injury mode (61.7%), whereas road traffic accident was mode of injury in 38.3% of cases (Fig. 8).
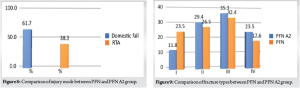
Boyd and griffin type III was the most common subtype constituting 33.8% of all patients, followed by type II (27.9%), type IV (20.6%) and then type I (17.7%) (Fig. 9). Comparison of demographic characteristics between PFN and PFNA2 shown in Table 1.

Surgical duration was recorded from skin incision to skin closure. The mean surgical duration was 74.1 min in PFN A2 group while 82.2 min in PFN group (Fig. 10). Mean surgical duration in both groups was statistically different (P = 0.039).
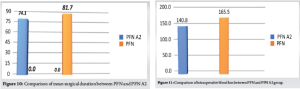
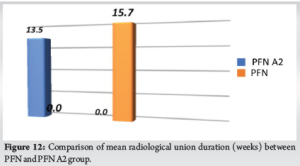
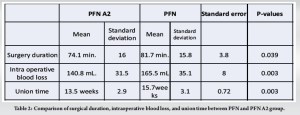
Intraoperative blood loss was assessed using blood soaked gauze piece and G-pad. The mean intraoperative blood loss was 140.8 ml in the group those who treated with PFNA2 and 165.5 mL in PFN group (Fig. 11). Difference between both the groups was statistically significant (P = 0.003). Union was assessed by anteroposterior, cross-table lateral view of Pelvis with both hip radiograph. The mean union time in PFNA2 group was 13.5 weeks and those patients treated with PFN was 15.7 weeks (Fig. 12). There was a statistically significant difference in Union time between both groups (P = 0.003). Comparison of surgical duration, intraoperative blood loss, and union time between PFN and PFN A2 is shown in Table 2.
Modified HHS assessed by the standard scoring sheet which consists of following points pain around hip, functional activity, hip range of motion, and any deformity present/absent, Based on the score patients, outcome is categorized as poor (<70), fair (70–79), good (80–89), and excellent (90–100). Modified HHS was assessed on 6th week, 3rd month, and 6th month.
Our study showed that mean HHS at 6-week follow-up was 70 for PFN A2 group and 66.1 for PFN group, at 3-month follow-up was 76.8 for PFN A2 group and 73.2 for PFN group, at 6-month follow-up was 83.1 for PFN A2 group and 79.8 for PFN group. There was no statistically significant difference between PFNA2 and PFN group at 6 weeks, 3-month, and 6 month follow-up. Comparison of HHS at 6 weeks, 3 months, and 6 months is shown in Table 3.
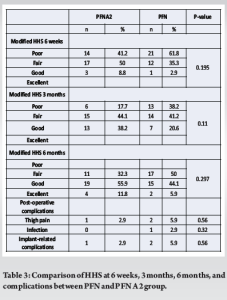
In our study, mainly three types of post-operative complications were observed -thigh pain, infection, implant-related complications (screw pullout and reverse z effect). Post-operative complications were higher in PFN group compare to PFN A2 group which was statistically not significant (Table 3).
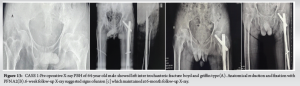
Case 1
A 64-year-old male patient presented with the left hip pain following a RTA (Fig. 13). X-ray PBH showed an intertrochanteric fracture boyd and griffin type 1(A). Patient underwent through CRIF with PFN A2. Immediate post-operative X-ray showed anatomical reduction and optimal position of helical blade (B). Six-week follow-up X-ray showed sign of union (C) which was maintained final 6-month follow-up X-ray (D).
Case 2
A 76-year-old male came to opd with left hip pain following a domestic fall (Fig. 14). Anteroposterior view of X-ray PBH suggested left intertrochanteric fracture boyd and griffin type 2(A). Patient underwent CRIF with PFN -A. Post-operative radiograph showed adequate reduction and optimal screw position (B,C). Three-month follow-up X-ray showed signs of union (D).

Complications
Case 1
A 70-year-old female came to OPD with the complaint of the left hip pain following a domestic fall. X-ray PBH suggested left inter trochanteric fracture boyd and griffin type 2 (Fig.15 [left]) which was underwent through CRIF with PFN A2 (Fig. 15 [middle]). Post-operative X-ray showed adequate fracture reduction. On 4-month post-surgery follow-up, patient presented with pain and swelling over left hip. X-ray suggested helical blade cutout with collapse at fracture site (Fig. 15 [right]). Then, the patient was managed with bipolar hemiarthroplasty.
Case 2
A 67-year-old male presented with pain over the right hip and swelling who had undergone CRIF with PFN, 1 month ago for a right intertrochanteric fracture (Fig. 16). Anteroposterior view X-ray PBH showed reverse z effect (B). Immediate post-operative X-ray showed anatomical reduction with optimal position of both screws (A).

Femoral intertrochanteric fracture one of the most frequently occurring fractures in the elderly individual following trivial trauma and uncommon in young adult. Intertrochanteric fracture occurs in young adult due to high-intensity trauma [1].
Various treatment modalities available for intertrochanteric fractures are cephalomedullary nails, DHS, DCP, proximal femoral locking plates, and trochanteric stabilization plates. The utmost goal of the treatment is early mobilization of patients to prevent fracture diseases.
Preferred implant for most of the intertrochanteric fractures are cephalomedullary nail. Intramedullary nails are biomechanically more powerful than extramedullary plates [11,12,13,14]. Intramedullary nails provide biological, mechanical, and technical advantage over plate and screw fixation [15,16,17]. Intramedullary nails are inserted by close procedure with indirect fracture reduction, least soft-tissue damage, and maintaining vascularity of the fracture area [18] and Debris generates during reaming act as a graft at fracture site.
PFNA2 is biomechanically superior than conventional PFN especially in elderly osteoporotic patients. Helical blade is inserted by hammering without reaming, so bonestock is preserve in femoral head and neck. Cancellous bone compacts around the blade, provides significant purchase, and prevents varus collapse, rotational stress [19,20].
Another advantage of PNA2 is relatively small incision required for single helical blade insertion when compare with conventional 2 screw PFN (derotation and lag screw).
In this study, mean age of the patients was 66.2 years in PFN A2 group and 63.1 years in PFN group. In contrast, Sharma et al. reported statistically significant mean age difference between PFN A2 (74.12years) and PFN( 60.78years) group [21], whereas, Bhardwaj et al. reported almost similar mean age in both study groups (PFNA2:66.4 years and PFN: 66.2 years) [22]. Simmermacher et al. and Sadic et al. observed significantly high average age in their study group [23,24].
In our study, we found that males are predominantly affected in both groups and domestic fall was the most common mode of injury in both groups followed by RTA. Singh et al. recorded male predominance with a ratio of 1.2:1 similar to this study [25]. Bhardwaj et al. reported that males (64%) were commonly involved than females (36%) in both study group [22]. In contrast, Park et al. and Yadav and Dakshinamoorthy observed females are significantly injured in both PFN A2 and PFN group [26,27].
Gadhe et al. reported that domestic fall was the most common mode of injury in both groups [28]. Shah et al. also observed majority of fracture occurs due to domestic fall or slippage, similar to this study [29].
In present study, majority of patients had the left-sided injury (54.4%). Singh and Bhartiya also reported similar results regard to side of injury in their study [30]. Based on Boyd and griffin classification, type III was the most common type in both groups. In contrast, Shah et al. reported that type II was the most common type among all types [29].
This study shows statistically significant difference between PFN and PFNA2 groups with respect to intraoperative blood loss, surgery duration, radiological union, functional outcome, and complications.
Our study showed remarkably less mean intra operative blood loss (140.8 mL) and surgical duration (74.1 min) in PFNA2 group when compared with PFN group (intraoperative blood loss 165.5 mL, surgical duration 81.7 min). et al. found duration of surgery was significantly lesser in helical blade group which is similar to this study [21]. Kashid et al. and Mohan et al. also recorded less surgical duration and blood loss in PFN A2 group [1,31].
Radiological union was evaluated in OPD by X-ray PBH anteroposterior and lateral view until 6 months. Union was seen in all 68 patients (100%). This study shows that mean union period was lesser in PFN A2 group (13.5 weeks) than PFN (15.7 weeks). Shah et al. reported average union time for PFN A2 group was 13.6 weeks whereas 14.8 weeks for PFN [29]. Harshwardhan et al. reported less union time and surgical duration in those patients operated with PFN A2 [33].
Functional outcome measurement based on modified HHS at 6 months in PFNA2 was found excellent in 11.8% of patients, good in 55.9% of patients, fair in 32.3% of cases whereas excellent outcome seen in 5.9% of patients, good in 44.1 % patients, and fair in 50% patients those who were treated by PFN. In our study, mean modified HHS was 76.8 in PFN A2 group and 73.2 in PFN group at 3-month follow-up which was increased at 6-month follow-up (PFN A 2 group: 83.1 and PFN group: 79.8). No statistically significant difference in functional outcome at 3- and 6-month follow-up. Sharma et al. reported average modified HHS was 75.37 in PFN group and 78.85 for PFN A2 group with no significant difference in their final follow-up [21]. Kashid et al. recorded mean HHS at 1-year follow-up which was 86.8 in helical blade nail group and 88.5 in conventional two-screw nail group(1). Singh and Bhartiya, Stern et al. observed almost equal functional outcomes in both groups [30,34].
Complications like screw cut out, screw back out, and reverse z effect cause biomechanical failure of implant. This study shows complication rate of PFN group (17.6%) was higher than PFNA2 group(5.9%) which was not statistically significant. Mora et al., Choo et al. found less incidence of post-operative complications in PFN A2 than PFN group [5,35] similar to our study. Gardenbroek et al., Loo et al. recorded more late complications and resurgery in PFN A2 group than the conventional PFN group [32,35,36]. Park et al. reported significantly better social functional score and less complications in the PFN A2 group [26]. Mallya et al., Ghimire et al. showed that PFN A2 had better functional outcome than PFN with less complications [37,38]. Kumar and Srivastava reported mean blood loss and surgical duration was significantly lesser in PFN A2 group when compare with PFN group with low implant-related complications like screw/blade cutout and implant breakage [39].
Limitations of the study were single-centered comparative study with shorter duration of follow-up and small sample size. Another limitation of the study was: osteoporosis cannot be assessed by DEXA scan due to financial issues. More randomized control trials with longer period of follow-up and larger sample size over a wide range of population is required to evaluate more precise functional outcomes of PFN and PFNA2 in intertrochanteric fracture.
Our study infer that PFN A2 has significant advantages when compared to conventional PFN like significantly less surgical duration and intraoperative blood loss with faster union time with smaller incision. Functional outcome is slightly better in PFN A2 group. Implant-related complications are lesser in PFN A2 that indicate biomechanical dominance of helical blade device over conventional dual screw system.
Our study concludes that PFN A2 is a better option than PFN for all types of intertrochanteric fracture in adult individuals.
PFN A2 significantly lessens intraoperative blood loss, surgical duration, union over PFN. Functional outcome improves in PFN A2 but statistically not significant in PFN A2 group. PFN A2 is the most effective option for all type of intertrochanteric fracture.
References
- 1.Kashid MR, Gogia T, Prabhakara A, Jafri MA, Shaktawat DS, Shinde G. Comparative study between proximal femoral nail and proximal femoral nail antirotation in management of unstable trochanteric fractures. Int J Res Orthop 2016;2:354-8. [Google Scholar | PubMed]
- 2.Melton LJ 3rd, Kearns AE, Atkinson EJ, Bolander ME, Achenbach SJ, Huddleston JM, et al. Secular trends in hip fracture incidence and recurrence. Osteoporos Int 2009;20:687-94. [Google Scholar | PubMed]
- 3.Salphale Y, Gadegone WM, Ramteke A, Karandikar N, Shinde R, Lalwani P. Prox-imal femoral nail in reverse trochanteric femoral fractures: An analysis of 53 cases at one year follow-up. Surg Sci 2016;7:300-8. [Google Scholar | PubMed]
- 4.Siu AL, Penrod JD, Boockvar KS, Koval K, Strauss E, Morrison RS. Early ambulation after hip fracture: Effects on function and mortality. Arch Intern Med 2006;166:766-71. [Google Scholar | PubMed]
- 5.Choo SK, Oh HK, Choi JY. PFNA and PFN in intertrochanteric fractures-comparison study of sliding. J Korean Hip Soc 2010;22:79-85. [Google Scholar | PubMed]
- 6.Kulkarni GS, Limaye, R, Kulkarni M, Kulkarni S. Intertrochanteric fractures. Indian J Orthop 2006;40:16-23. [Google Scholar | PubMed]
- 7.Hohendorff B, Meyer P, Menezes D, Meier L, Elke R. Behandlungsergebnisse und Komplikationen nach PFN-Osteosynthese [Treatment results and complications after PFN osteosynthesis]. Unfallchirurg 2005;108:938, 940, 941-6 passim. [Google Scholar | PubMed]
- 8.Gao H, Bai X, Chen W, Li Y, Zhao L, Liu C, et al. Clinical and functional comparison of dynamic hip screws and intramedullary nails for treating proximal femur metastases in older individuals. Chin J Cancer Res 2020;32:395-402. [Google Scholar | PubMed]
- 9.Raviraj A, Anand A, Chakravarthy M, Pai S. Proximal femoral nail antirotation (PFNA) for treatment of osteoporotic proximal femoral fractures. Eur J Orthop Surg Traumatol 2012;22:301-5. [Google Scholar | PubMed]
- 10.Strauss E, Frank J, Lee J, Kummer FJ, Tejwani N. Helical blade versus sliding hip screw for treatment of unstable intertrochanteric hip fractures: A biomechanical evaluation. Injury 2006;37:984-9. [Google Scholar | PubMed]
- 11.Loubignac F, Chabas JF. A newly designed locked intramedullary nail for trochanteric hip fractures fixation: Results of the first 100 Trochanteric implantations. Orthop Traumatol Surg Res 2009;95:139-44. [Google Scholar | PubMed]
- 12.Kubiak EN, Bong M, Park SS, Kummer F, Egol K, Koval KJ. Intramedullary fixation of unstable intertrochanteric hip fractures: One or two lag screws. J Orthop Trauma 2004;18:12-17. [Google Scholar | PubMed]
- 13.Butt MS, Krikler SJ, Nafie S, Ali MS. Comparison of dynamic hip screw and gamma nail: A prospective, randomized, controlled trial. Injury 1995;26:615-8. [Google Scholar | PubMed]
- 14.Anglen JO, Weinstein JN. Nail or plate fixation of intertrochanteric hip fractures: Changing pattern of practice. A review of the American board of orthopaedic surgery database. J Bone Joint Surg Am 2008;90:700-7. [Google Scholar | PubMed]
- 15.Parker MJ, Handoll HH. Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Syst Rev 2010;9:Cd000093. [Google Scholar | PubMed]
- 16.Zhang K, Zhang S, Yang J, Dong W, Wang S, Cheng Y, et al. Proximal femoral nail vs. dynamic hip screw in treatment of intertrochanteric fractures: A meta-analysis. Med Sci Monit 2014;20:1628-33. [Google Scholar | PubMed]
- 17.Garg B, Marimuthu K, Kumar V, Malhotra R, Kotwal PP. Outcome of short proximal femoral nail antirotation and dynamic hip screw for fixation of unstable trochanteric fractures. A randomised prospective comparative trial. Hip Int 2011;21:531-6. Retraction in: Spencer RF. Hip Int 2012;22:487. [Google Scholar | PubMed]
- 18.Gavaskar A, Subramanian M, Tummala N. Results of proximal femoral nail antirotation for low velocity trochanteric fractures in the elderly. Indian J Orthop 2012;46:556-60. [Google Scholar | PubMed]
- 19.Kaushal A, Anand A, Sethy P, Priyadarshi S. Comparative study of functional and radiological outcome of pertrochanteric fracture fixation by proximal femoral nail antirotation 2 and old proximal femoral nail. J Orthop Dis Traumatol 2023;6:228-33. [Google Scholar | PubMed]
- 20.Rai B, Singh J, Singh V, Singh G, Pal B, Kumar D, et al. Evaluation of the outcomes of proximal femoral nail antirotation II in the treatment of trochanteric fracture in elderly patients. Cureus 2022;14:e24896. [Google Scholar | PubMed]
- 21.Sharma A, Mahajan A, John B. A comparison of the clinico-radiological outcomes with proximal femoral nail (PFN) and proximal femoral nail antirotation (PFNA) in fixation of unstable intertrochanteric fractures. J Clin Diagn Res 2017;11:RC05-9. [Google Scholar | PubMed]
- 22.Bhardwaj S, Sakale H, Agrawal AC, Kar B, Dash RN, Rai A, et al. A comparison of the clinicoradiological outcomes of intertrochanteric fractures treated using proximal femoral nail and proximal femoral nail anti-rotation. Cureus 2024;16:e60639. [Google Scholar | PubMed]
- 23.Simmermacher RK, Ljungqvist J, Bail H, Hockertz T, Vochteloo AJ, Ochs U, et al. The new proximal femoral nail antirotation (PFNA) in daily practice: Results of a multicentre clinical study. Injury 2008;39:932-9. [Google Scholar | PubMed]
- 24.Sadic S, Custovic S, Jasarevic M, Fazlic M, Smajic N, Hrustic A, et al. Proximal femoral nail antirotation in treatment of fractures of proximal femur. Med Arch 2014;68:173-7. [Google Scholar | PubMed]
- 25.Singh S. Proximal femoral nail versus proximal femoral nail antirotation: Functional and radiological outcome in intertrochanteric fractures of femur. Cureus 2021;13:e19093. [Google Scholar | PubMed]
- 26.Park JH, Lee YS, Park JW, Wang JH, Kim JG. A comparative study of screw and helical proximal femoral nails for the treatment of intertrochanteric fractures. Orthopedics 2010;33:81-5. [Google Scholar | PubMed]
- 27.Yadav S, Dakshinamoorthy R. Comparison of twin screw derotation type versus single helical blade type cephalomedullary nail in trochanteric fractures in geriatric population. Cureus 2022;14:e31557. [Google Scholar | PubMed]
- 28.Gadhe SS, Bhor P, Patel I, Vatkar AJ, Kale S, Kanade G. Comparative study of PFNA vs PFNA 2 in unstable intertrochanteric fractures: A randomised control study of 50 cases. Int J Orthop Sci 2019;5:162-4. [Google Scholar | PubMed]
- 29.Shah MR, Shah MM, Shah IM, Shah KR. Surgical and functional outcomes of the results of conventional two-screw proximal femoral nail (PFN) versus helical-blade anti-rotation proximal femoral nail (PFNA2). Cureus 2023;15:e43698. [Google Scholar | PubMed]
- 30.Singh SK, Bhartiya RK. A comparative study of unstable intertrochanteric fracture by proximal femoral nail versus proximal femoral nail anti-rotation among adult patients. Gal Int J Health Sci Res 2021;6:27-33. [Google Scholar | PubMed]
- 31.Mohan S, Shivaprakash U, Sridhar S. PFNA v/S PFN in the management of unstable intertrochanteric fracture S. J Evol Med Dent Sci 2015;4:4086-91. [Google Scholar | PubMed]
- 32.Gardenbroek T, Segers M, Simmermacher R, Hammacher E. The proximal femoral nail antirotation: An identifiable improvement in the treatment of unstable pertrochanteric fractures? J Trauma 2011;71:169-74. [Google Scholar | PubMed]
- 33.Harshwardhan H, Jain S, Sharma M. An outcome analysis of intertrochanteric fracture of femur managed with proximal femoral nail antirotation II. Int J Res Orthop 2019;5:699. [Google Scholar | PubMed]
- 34.Stern R, Lübbeke A, Suva D, Miozzari H, Hoffmeyer P. Prospective randomised study comparing screw versus helical blade in the treatment of low-energy trochanteric fractures. Int Orthop 2011;35:1855-61. [Google Scholar | PubMed]
- 35.Mora A, Marimon I, Rius M, Brill W, Corral A, Gaya S. PFN versus PFNA in treatment of trochanteric femoral fractures: A prospective study. Bone Joint J Orthop Proceed 2011;93:136. [Google Scholar | PubMed]
- 36.Loo WL, Loh J, Lee HC. Review of proximal nail antirotation (PFNA) and PFNA-2-our local experience. Malays Orthop J 2011;5:1-5. [Google Scholar | PubMed]
- 37.Mallya S, Kamath SU, Madegowda A, Krishnamurthy SL, Jain MK, Holla R. Comparison of radiological and functional outcome of unstable intertrochanteric femur fractures treated using PFN and PFNA-2 in patients with osteoporosis. Eur J Orthop Surg Traumatol 2019;29:1035-42. [Google Scholar | PubMed]
- 38.Ghimire K, Wod R, Pokharel J, Adhikari S, Gurung S, Baral N, et al. Outcome of intertrochanteric fracture managed with proximal femoral nail antirotation 2. Asian J Med Sci 2023;14:182-5. [Google Scholar | PubMed]
- 39.Kumar CN, Srivastava MP. Screw versus helical proximal femoral nail in the treatment of unstable trochanteric fractures in the elderly. J Clin Orthop Trauma 2019;10:779-84. [Google Scholar | PubMed]