Metacarpophalangeal joint dislocation has a typical pathoanatomy, which should be kept in mind and open reduction method should not be hesitated in appropriate cases.
Dr. Debanjan Das, Orthopaedics Consultant , Department of Orthopaedics, Tata Main Hospital, Jamadoba, Dhanbad, Jharkhand, India. Email- drdebanjad@yahoo.com
Introduction: Metacarpophalangeal (MCP) joint dislocation and its pathoanatomy was first discussed in detail in an article written by Kaplan et al . ,in 1957. They had identified certain features of complex, that is irreducible MCP joint dislocation through closed method to differentiate from a simple MCP joint dislocation, that is MCP joint dislocation that can be reduced by closed method. The complex MCP joint dislocations (mostly involving the index finger) are called Kaplan dislocations. Here, we describe two cases of MCP joint dislocations to highlight the differences between complex and simple MCP joint dislocation in their clinical appearances, X-rays, and management protocol.
Case Report: In the first case, the injured patient was a 17-year-old young cricketer, who sustained the injury while playing the game. After careful clinical examination and studying the X-rays, we assured the patient and treated his injury by closed reduction method. After undergoing the post-reduction splinting and physiotherapy, the patient has recovered completely and he is back to playing cricket. In the second case, the patient was an elderly lady; she got her left index finger dislocated while trying to forcefully hold a moving object. After careful clinical examination and studying the X-rays, we counselled her and treated her injury through open reduction method. After following the post-operative splinting and physiotherapy, the patient is doing well but her index finger extension is restricted in the terminal ranges.
Conclusion: The MCP joint dislocations have distinctive clinico - pathological patterns and we should carefully study them. We should not hesitate to adopt open reduction techniques in appropriately indicated patients.
Keywords: Simple, complex, metacarpophalangeal joint dislocation, noose effect, open and closed reduction methods
The metacarpophalangeal (MCP) joints from a condylar type of joint between the metacarpal head and base of proximal phalanx with their capsule extending from the base of the proximal phalanx to the neck of the meta carpals [1]. These joints are pretty stable joints with flexion, extension, adduction, abduction, and circumduction type of movements [2]. Finger MCP joint dislocations account for about 5% of upper extremity injuries [1]. These dislocations are relatively rare injuries and Farabeaf et al. in 1876 first descried about the MCP joint dislocations but their description was mostly related to thumb MCP dislocation [1]. Kaplan in the year 1957 described in detail about the pathoanatomy and irreducible nature of dorsal index MCP dislocation [3].
Case Report 1
A young boy of 17 years came to our emergency with complaints of acute pain and swelling of the left thumb base while playing cricket and trying to catch a ball. There was swelling around the thumb base, and any joint movement was painfully restricted. There was no associated skin dimpling and puckering around the thumb base. X-rays showed that there was dislocation of the thumb MCP joint with dorsal displacement of the proximal phalanx of left thumb. The dislocation was easily reduced under sedation and with gentle longitudinal traction. After reduction, the hand was splinted with plaster of paris thumb spica splinting for 2 weeks and then gradually thumb range of motion movements started. The patient is a junior professional cricketer, and he has returned successfully to his sport after 2 months.
Case Report 2
An elderly lady of around 60 years came to our hospital with severe pain in her left index finger base after she got injured while she was trying to hold a grip very forcefully. The left-hand index finger was kept semiflexed position in the proximal interphalangeal joint and slightly extended at the metacarpophalangeal joint. The index finger base was very tender and there was a visible dimple near the A1 flexion pulley area of the left index finger. There was no open injury. X-rays were done and it showed that 2nd MCP joint was dislocated with a small chip fracture of the 2nd metacarpal head. The dislocation was irreducible and it needed an open reduction, we approached through the dorsal approach to the MCP joint. After skin incision and carefully separating the extensor tendons, the joint capsule was identified, a longitudinal capsulotomy was done and the trapped volar plate was freed with a small curved periosteal elevator, after relocating the trapped volar plate, the dislocated phalanx could be easily relocated to its original position. The reduction was checked both clinically and radiologically with c-arm images. The small bone fragment was excised and the capsulotomy was closed with 2–0 vicryl. After checking the hemostasis, the wound was closed. The joint was splinted with MCP joint at 30° flexion, and stitches were removed after 2 weeks, range of motion exercises were started after 3 weeks, and patient was advised to limit the last 20° extension of the 2nd MCP joint.
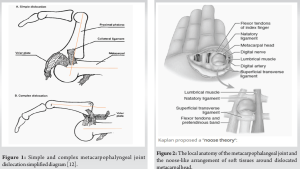



To understand the complexity of the MCP dislocation, we must first understand the role of the volar plate of the MCP joint. In Fig. 1, the volar plate is not trapped between the metacarpal head and the base of proximal phalanx; moreover, here, the dislocated proximal phalanx is making an angle of almost 90° to the metacarpal shaft.
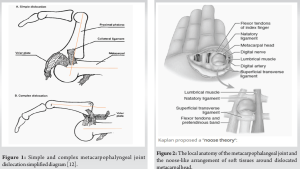
In Fig. 2, the volar plate is trapped between the metacarpal head and the dislocated proximal phalanx, and here, the dislocated proximal phalanx is staying almost parallel to the metacarpal shaft. The first clinical condition is termed as simple MCP joint dislocation, as here there is no obstruction of volar plate, and the dislocation can easily be reduced by closed methods. However, the second clinical scenario is called as the complex or the irreducible MCP dislocation as here the intervening obstructing volar plate blocks the dislocation by closed methods, and it needs open method to release the obstructing volar plate to achieve relocation [3]. The distinctive anatomy of simple and complex MCP joint dislocation is also evident in radiographs, as in the first case, the proximal phalanx almost lies perpendicular to the metacarpal shaft, and in the second case, the dislocated proximal phalanx lies almost parallel to the metacarpal shaft, the so-called bayonet appearance. This helps to alert the clinician about the nature of the dislocation. The complex dislocation of the metacarpophalangeal joint dorsally is called the Kaplan dislocation (Fig. 3-5). Although it can involve any fingers, the most common is the index finger MCP joint [4]. (Fig. 6). In his 1957 article, Kaplan described in detail the various anatomical structures around the MCP joint, especially emphasizing the button holing of the metacarpal head through the surrounding soft tissues and the interposition of the volar plate between the metacarpal neck and proximal phalanx base making close reduction very difficult [3]. The surrounding soft tissues produce a noose-like effect around the dislocated metacarpal if repeated closed reduction is tried without understanding the pathology [5]. The capsule of the MCP joint is strengthened by the volar plate ventrally. The radial side of the joint is reinforced by the lumbrical muscles and the ulnar side is strengthened by the flexor tendons of the digit along with pre-tendinous bands [5]. The superficial transverse ligament and the natatory ligament tighten around the metacarpal neck on repeated forceful reduction attempts, along with the extrinsic and intrinsic muscle tendons causing the noose effect as proposed by Kaplan [6]. There are various approaches described in literature to address this problem. Kaplan himself was fond of the volar approach [7] (Fig. 7 and 8). The volar approach approach helps to directly address the main interposing structure, the volar plate. It involves applying a curvilinear incision centering over the MCP joint. The A 1 pulley is often needed to be released to gain access to the dislocation. Mostly the entrapped volar plate can be freed without releasing it. However, it requires meticulous dissection as the dorsal digital artery and the digital nerves lie very close. Here, the volar plate remains intact, so chances of late dislocation or instability are minimal [8]. Becton et al., in their article proposed a simplified direct dorsal approach to treat this complex injury. Here, the dislocation is approached through the dorsal aspect by a curvilinear incision centering over the MCP joint. After releasing the skin and subcutaneous tissue, the joint capsule is approached. After releasing the joint capsule longitudinally, a white shining structure is found, that is the intervening volar plate, if attempts to slide the volar plate are not successful, then its needed to incise the volar plate longitudinally and slide it away to achieve reduction. Sometimes, the deep transverse collateral ligaments may also be needed to be released. Becton et al. also stated that the management of osteochondral fractures is easier by the dorsal approach. If the fragment is very small, it can be discarded or stitched with 2-o vicryl or if it is a lager fragment then it can be fixed with small transcutaneous k wire which can be removed percutaneously after 3 weeks [9]. Sandeep et al. in their case report described a percutaneous needling technique to incise the interposed volar plate and thus achieve a closed reduction [10].
Follow-up
We have got a 3-year follow-up for the case 1. The patient is a professional cricket player and he has gained his full range of motion of his injured finger. He has started playing his sport professionally. The second patient was an elderly lady with complex dislocation; we have a 2-year follow-up of the patient. She has gained almost full flexion of the injured finger but her extension is limited in terminal 20° and her finger movements are pain free (Fig. 9 and 10).
Complications
There are several complications reported in literature mostly post-traumatic arthritis due to repeated forceful attempts of reduction, iatrogenic injury, and finger stiffness. Premature physeal closure is also reported in pediatric cases [11].
The MCP joint dislocations should be considered in detail before coming to a management plan. We should counsel the patients properly about the nature of the injury before commencing the treatment. An open approach should be undertaken when indicated and should not be hesitated.
We should not hesitate to adopt an open reduction approach in complex metacarpophalangeal joint dislocations.
References
- 1.Rozmaryn LM. The collateral ligament of the digits of the hand: Anatomy, physiology, biomechanics, injury, and treatment. J Hand Surg Am 2017;42:904-15. [Google Scholar | PubMed]
- 2.Dinh P, Franklin A, Hutchinson B, Schnall SB, Fassola I. Metacarpophalangeal joint dislocation. J Am Acad Orthop Surg 2009;17:318-24. [Google Scholar | PubMed]
- 3.Kaplan EB. Dorsal dislocation of the metacarpophalangeal joint of the index finger. J Bone Joint Surg Am 1957;39:1081-6. [Google Scholar | PubMed]
- 4.Green DP, Butler TE Jr. Fractures and dislocations in the hand. In: Rockwood CA Jr., Green DP, Bucholz RW, Heckman JD, editors. Fractures in Adults. 4th ed., Vol. 1. Philidelphia PA: Lippincott-Raven; 1996. p. 607-700. [Google Scholar | PubMed]
- 5.Al-Qattan MM, Robertson GA. An anatomical study of the deep transverse metacarpal ligament. J Anat 1993;182:443-6. [Google Scholar | PubMed]
- 6.Johnson AE, Bagg MR. Ipsilateral complex dorsal dislocations of the index and long finger metacarpophalangeal joint. Am J Orthop (Belle Mead NJ) 2005;34:241-5. [Google Scholar | PubMed]
- 7.May JW Jr., Rohrich RJ, Sheppard J. Closed complex dorsal dislocation of the middle finger metacarpophalangeal joint: Anatomic considerations and treatment. Plast Reconstr Surg 1988;82:690-3. [Google Scholar | PubMed]
- 8.An MT, Kelley JP, Fahrenkopf MP, Kelpin JP, Adams NS, Do V. Complex metacarpophalangeal dislocation. Eplasty 2020;20:ic3. [Google Scholar | PubMed]
- 9.Becton JL, Christaian JD Jr., Goodwin HN, Jackson JG 3rd. A simplified technique for treating the complex dislocation of the index metacarpophalangeal joint. J Bone Joint Surg Am 1975;57:698-700. [Google Scholar | PubMed]
- 10.Yadav SK, Nayak B, Mittal S. New approach to second metacarpophalangeal joint dislocation management: The SKY needling technique. Eur J Orthop Surg Traumatol 2021;31:189-92. [Google Scholar | PubMed]
- 11.Rubin G, Orbach H, Rinott M, Rozen N. Complex dorsal metacarpophalangeal dislocation: Long-term follow-up. J Hand Surg Am 2016;41:e229-33. [Google Scholar | PubMed]
- 12.Gerrand CH, Jarrett PM. A dislocated finger. Postgrad Med J 1998;74:249-51. [Google Scholar | PubMed]







